In a world where discussions surrounding reproductive health often center around the presence, function, and care of the vagina, the absence of this essential organ is a topic that demands understanding.
Delving into the causes, diagnosis, and various treatment options, we embark on a journey of knowledge that challenges societal norms and sheds light on the experiences of those living with this unique condition.
Join us as we explore the intricacies and complexities surrounding the absence of a vagina, and discover the support and resources available for young women’s health care.
absence of vagina
Vaginal agenesis is a condition in which a person is born without a vagina.
Diagnosis involves various exams such as external genital exam, modified internal exam, ultrasound, and MRI.
Testing for MRKH syndrome, which is often associated with vaginal agenesis, includes examining chromosomes and genetic causes.
Treatment options for vaginal agenesis include creating a vagina if sexual intercourse is desired, and vaginal dilators are recommended as the first choice.
Dilators are used to stretch the vaginal canal to a normal length, and the success rate depends on consistent use and applied pressure.
Water-based lubricant may be necessary during intercourse.
Boston Children’s Hospital and the Center for Young Women’s Health offer specialized care for vaginal agenesis, providing diagnostic testing, treatment, counseling, and follow-up services.
They have multidisciplinary teams consisting of gynecologists, radiologists, nurse specialists, and social workers to offer comprehensive care options.
Key Points:
- Vaginal agenesis is a condition where a person is born without a vagina.
- Diagnosis involves a range of exams, including external and internal exams, ultrasound, and MRI.
- Testing for MRKH syndrome, often associated with vaginal agenesis, involves examining chromosomes and genetic causes.
- Treatment options include creating a vagina if desired, with vaginal dilators as the first choice.
- Dilators stretch the vaginal canal to a normal length, with success depending on consistent use and applied pressure.
- Water-based lubricant may be necessary during intercourse.
- Boston Children’s Hospital and the Center for Young Women’s Health offer specialized care for vaginal agenesis, including diagnostic testing, treatment, counseling, and follow-up services.
absence of vagina – Watch Video
💡
Pro Tips:
1. Despite the popular notion that all mammals possess a vagina, the platypus, an egg-laying mammal, remarkably lacks a typical vaginal opening. Instead, it has a cloaca, a single opening that serves for both reproductive and excretory functions.
2. Surprisingly, some female sharks, such as the great white shark, have a reproductive system devoid of a vaginal opening. During mating, male sharks insert their claspers, which are modified pelvic fins, into the female’s cloaca to transfer sperm.
3. The absence of a functional vagina can occur due to a medical condition called Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. This rare condition affects approximately 1 in every 4,500 individuals born female, where the vagina and uterus are either absent or significantly underdeveloped.
4. In certain species of flatworms, known as hermaphroditic flatworms, no distinct vaginas exist. Instead, these worms engage in a fascinating mating ritual called “penis fencing,” where they compete to inseminate each other by stabbing with their pointed penises. The first one to successfully inseminate becomes the father while the receptor becomes the mother.
5. In ancient Greek mythology, a tale exists that explains the absence of a vagina in the sculpture of the famous goddess Aphrodite. According to the story, Aphrodite was crafted by the gods using the foam of the sea, and during this process, her genitalia were purposely left unformed and absent, symbolizing her eternal purity and desirability.
Vaginal Agenesis: Definition And Causes
Vaginal agenesis is a rare condition characterized by the absence or underdevelopment of the vagina in individuals at birth. It is estimated to affect a small percentage of the population. The exact cause of vaginal agenesis is not fully understood, but it is believed to result from a combination of genetic and environmental factors. This condition can have significant implications for both physical and psychological well-being.
Some key points about vaginal agenesis:
- Vaginal agenesis is a condition where the vagina is either absent or underdeveloped at birth.
- It is a rare condition that affects a small percentage of the population.
- The exact cause of vaginal agenesis is not fully understood.
- The condition is believed to be influenced by a combination of genetic and environmental factors.
- Vaginal agenesis can have significant implications for both physical and psychological well-being.
In conclusion, vaginal agenesis is a rare condition with profound effects on individuals’ physical and psychological health.
Diagnosis Of Vaginal Agenesis: What To Expect
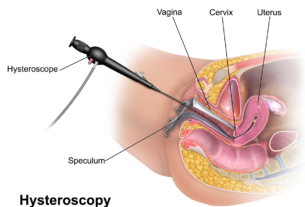
Diagnosing vaginal agenesis involves a series of medical examinations and tests. The process typically begins with an external genital exam, where a healthcare provider examines the external structures of the individual’s genitals. This is followed by a modified internal exam, where a speculum is inserted into the vaginal opening to visualize any abnormalities.
Further diagnostic procedures may include the use of ultrasound and magnetic resonance imaging (MRI) scans to get a more detailed picture of the reproductive organs. Additionally, a karyotype, which examines the individual’s chromosomes, may be performed to determine if there are any genetic causes for the condition.
Mrkh Syndrome And Vaginal Agenesis: Understanding The Link
Müllerian agenesis, also known as Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, is a condition often associated with vaginal agenesis. This congenital disorder is characterized by the absence of the uterus and upper two-thirds of the vagina. Diagnosis of MRKH syndrome usually occurs during the evaluation of individuals with vaginal agenesis.
Testing for MRKH syndrome involves various procedures, such as karyotype analysis to examine the chromosomes and identify any genetic causes. It is important to highlight that not all individuals with vaginal agenesis have MRKH syndrome, suggesting that there may be other factors contributing to the condition.
To summarize:
- Müllerian agenesis or MRKH syndrome is commonly linked to vaginal agenesis.
- MRKH syndrome involves the absence of the uterus and upper two-thirds of the vagina.
- Diagnosis is typically made during evaluation of individuals with vaginal agenesis.
- Testing for MRKH syndrome includes a karyotype analysis to examine chromosomes.
- Not all cases of vaginal agenesis are attributed to MRKH syndrome, indicating other possible causes.
Options For Treating Vaginal Agenesis
Treatment options for vaginal agenesis aim to create a functional vagina, particularly for individuals who desire sexual intercourse. One of the primary treatment approaches involves the use of vaginal dilators.
Vaginal dilators are specially designed devices that are inserted into the vaginal canal to stretch and expand it gradually over time.
The success of dilator treatment depends on consistent use and applied pressure. Patients are typically advised to start with smaller dilators and gradually progress to larger sizes as the vaginal canal expands.
Dilator therapy may be accompanied by the use of water-based lubricants during intercourse to minimize discomfort.
- Treatment options for vaginal agenesis include vaginal dilators
- Vaginal dilators stretch and expand the vaginal canal
- Consistent use and applied pressure are key to the success of dilator treatment
- Start with smaller dilators and gradually progress to larger sizes
- Use water-based lubricants during intercourse to minimize discomfort.
“The success of dilator treatment depends on consistent use and applied pressure.”
Using Vaginal Dilators For Vaginal Agenesis Treatment
Vaginal dilators are commonly recommended as the primary treatment for individuals with vaginal agenesis. These medical devices are specifically designed to stretch and expand the vaginal canal.
- Dilators come in various sizes and are typically made of smooth, body-safe materials such as medical-grade silicone.
To use a vaginal dilator, the individual gently inserts it into the vaginal opening and gradually advances it deeper into the canal. This process needs to be repeated regularly to encourage gradual stretching and expansion of the vaginal tissue.
Important: Dilator therapy should always be conducted under the guidance and supervision of a healthcare professional.
-
Proper guidance and supervision from a healthcare professional is crucial for safe and effective dilator therapy.
-
Using vaginal dilators helps stretch and expand the vaginal canal in individuals with vaginal agenesis.
Note: Vaginal dilators are considered the first-line treatment for vaginal agenesis.
Stretching The Vaginal Canal: How Dilators Work
Vaginal dilators work by applying gentle and consistent pressure to the vaginal walls. This pressure encourages the tissues to stretch and expand over time, ultimately creating a functional vaginal canal. Dilators should be used regularly and according to a prescribed schedule to achieve the desired results.
Apart from stretching the vaginal canal, dilators also help to maintain the length and flexibility of the tissue. They can be a crucial component of the overall treatment plan for individuals with vaginal agenesis, offering them the potential to lead fulfilling and satisfying sexual lives.
The Importance Of Consistent Dilator Use For Success
Consistency is key when it comes to dilator therapy for vaginal agenesis. Regular and diligent use of the dilators is essential for achieving successful outcomes. It is important to follow the prescribed treatment plan provided by a healthcare professional and commit to the suggested schedule without skipping sessions.
Consistent use of dilators helps ensure gradual, long-term results. By incorporating dilator therapy into their daily routine, individuals with vaginal agenesis can effectively achieve the stretching and expansion necessary for a functional vagina.
- Dilator therapy requires regular and diligent use
- Follow the prescribed treatment plan provided by a healthcare professional
- Commit to the suggested schedule without skipping sessions
Overcoming Challenges: Lubricant Use During Intercourse
For individuals with vaginal agenesis, water-based lubricants can be a helpful tool during sexual intercourse. Since the natural lubrication process of the vagina may be absent or inadequate, using a lubricant can reduce friction, discomfort, and pain.
It is important to choose a water-based lubricant, as other types of lubricants may cause irritation or damage to the delicate vaginal tissue. Water-based lubricants are typically safe and compatible with medical devices like dilators.
Boston Children’s Hospital: Leading Care For Vaginal Agenesis
Boston Children’s Hospital is a renowned medical institution that provides expert care for vaginal agenesis. Their team of dedicated healthcare professionals specializes in diagnosing and treating individuals with reproductive organ anomalies, including vaginal agenesis.
The multidisciplinary team at Boston Children’s Hospital consists of experienced gynecologists, radiologists, nurse specialists, and social workers. They offer comprehensive services such as:
- Diagnostic testing
- Personalized treatment plans
- Counseling
- Ongoing follow-up care
Patients and their families can find support and guidance throughout their healthcare journey.
Boston Children’s Hospital is dedicated to providing high-quality care and support for individuals with vaginal agenesis. Our multidisciplinary team of healthcare professionals is here to guide you through every step of your treatment plan.
Anomalies Of The Reproductive Tract: Specialized Treatment For Vaginal Agenesis
The Center for Young Women’s Health at Boston Children’s Hospital is specifically dedicated to providing specialized treatment for reproductive organ anomalies, including vaginal agenesis. The center adopts a team approach, ensuring accurate diagnoses and exceptional care for young women.
In addition to personalized treatment options, they offer an array of programs, resources, and services that focus on:
- Gynecology
- Sexuality and health
- Development
- Fitness and nutrition
- Emotional health
The center strives to empower and support young women with vaginal agenesis, helping them navigate their reproductive health and overall well-being.
Vaginal agenesis is a complex condition that can have significant physical and psychological impacts on individuals. Accurate diagnosis and appropriate treatment are essential for managing this condition. Vaginal dilators, consistent use, and lubricant use can contribute to creating a functional vagina and fostering a fulfilling sexual life.
Institutions like Boston Children’s Hospital and the Center for Young Women’s Health provide specialized care, resources, and support for individuals with vaginal agenesis. With comprehensive medical guidance and emotional assistance, individuals with vaginal agenesis can overcome challenges and thrive in their overall well-being and quality of life.
💡
You may need to know these questions about absence of vagina
1. What medical conditions can lead to the absence of a vagina in females?
There are several medical conditions that can lead to the absence of a vagina in females. One such condition is called Mayer-Rokitansky-Küster-Hauser syndrome (MRKH). This is a congenital disorder where the vagina and uterus do not develop properly, resulting in the absence of a vagina. Women with MRKH syndrome typically have normal external genitalia but may have other reproductive abnormalities.
Another condition that can lead to the absence of a vagina is androgen insensitivity syndrome (AIS). In AIS, individuals with female chromosomes (XX) are partially or completely resistant to the effects of male hormones (androgens). This leads to differences in development, including the absence or underdevelopment of internal reproductive organs such as the uterus and vagina.
2. How does the absence of a vagina impact a person’s reproductive health and fertility?
The absence of a vagina, also known as vaginal agenesis or Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, can have an impact on a person’s reproductive health and fertility. Without a vagina, individuals with MRKH syndrome are unable to have natural vaginal intercourse, which can affect their ability to conceive naturally. However, it is essential to note that having MRKH syndrome does not necessarily mean infertility, as the person’s ovaries and uterus are usually unaffected.
In many cases, individuals with MRKH syndrome may undergo treatments such as surgery or dilation techniques to create or expand a functional vaginal canal, enabling them to have intercourse and potentially conceive through assisted reproductive technologies. In-vitro fertilization (IVF) and embryo transfer can be viable options for achieving pregnancy for those with MRKH syndrome who desire biological children. Overall, while the absence of a vagina can present challenges for reproductive health and fertility, various medical interventions exist to help individuals with MRKH syndrome in their journey towards parenthood.
3. What surgical options are available for individuals with the absence of a vagina who desire a functional reproductive system?
One surgical option available for individuals with the absence of a vagina who desire a functional reproductive system is vaginoplasty. Vaginoplasty is a surgical procedure that constructs a vagina using existing tissue or through the creation of a new canal. This procedure aims to create a functional and anatomically correct vaginal opening, allowing for sexual intercourse and facilitating the possibility of reproductive options such as in vitro fertilization (IVF) or embryo transfer.
Another surgical option that can be considered is the creation of a neovagina using tissue grafts or a dilator-based technique. This procedure involves forming a vaginal canal using tissue grafts or gradually stretching the existing tissue to create depth and width. Although this method does not provide the same level of functionality as vaginoplasty, it can still allow for sexual intercourse and may also enable reproductive options through assisted reproductive technologies. The choice of surgical procedure depends on an individual’s specific circumstances and desired outcomes.
4. What psychological and emotional challenges may individuals with the absence of a vagina face, and what support is available to them?
Individuals with the absence of a vagina, such as those with Mayer-Rokitansky-Küster-Hauser syndrome or transgender women, may face significant psychological and emotional challenges. The absence of a vagina can lead to feelings of gender dysphoria, body image issues, and a sense of incompleteness. This may also affect their self-esteem, relationships, and overall mental well-being.
Support for individuals with the absence of a vagina is available in various forms. Professional mental health counseling and therapy can provide a safe space for individuals to express their emotions, explore their feelings about their bodies, and develop coping mechanisms. Support groups and online communities can also be invaluable, as they allow individuals to connect with others who have shared experiences and can offer guidance, advice, and empathy. Additionally, medical interventions such as vaginoplasty can offer a physical solution for some individuals, while also contributing to their psychological well-being.
Reference source
https://www.childrenshospital.org/conditions/vaginal-agenesis
https://www.mayoclinic.org/diseases-conditions/vaginal-agenesis/symptoms-causes/syc-20355737
https://my.clevelandclinic.org/health/diseases/23458-vaginal-agenesis
https://www.urologyhealth.org/urology-a-z/v/vaginal-abnormalities-vaginal-agenesis