The body can be a mysterious and complex machine, especially when it comes to our reproductive system.
One condition that often leaves women puzzled is anovulatory dysfunctional uterine bleeding.
This peculiar term may sound intimidating, but fear not!
In this article, we’ll delve into the world of abnormal uterine bleeding to shed light on this elusive and sometimes frustrating phenomenon.
Buckle up because we’re about to uncover the inner workings of our menstrual cycle and the puzzling disruptions that can occur along the way.
anovulatory dysfunctional uterine bleeding
Anovulatory dysfunctional uterine bleeding refers to abnormal uterine bleeding that occurs due to a disturbance in the normal hypothalamic-pituitary-ovarian axis.
This leads to irregular bleeding episodes, amenorrhea (absence of menstrual periods), metrorrhagia (bleeding between periods), menometrorrhagia (excessive or prolonged bleeding), as well as changes in prostaglandin concentration and increased endometrial responsiveness to vasodilating prostaglandins.
This condition is different from ovulatory dysfunctional uterine bleeding, which involves cyclic bleeding and defects in the control mechanisms of menstruation.
Women with anovulatory dysfunctional uterine bleeding may experience changes in endometrial vascular structure as well.
Key Points:
- Anovulatory dysfunctional uterine bleeding is abnormal uterine bleeding caused by disruption in the hypothalamic-pituitary-ovarian axis.
- Symptoms include:
- irregular bleeding episodes
- absence of menstrual periods
- bleeding between periods
- excessive or prolonged bleeding.
- Prostaglandin concentration and endometrial responsiveness to vasodilating prostaglandins are also affected.
- This condition is distinct from ovulatory dysfunctional uterine bleeding, which involves cyclic bleeding and defects in menstrual control mechanisms.
- Women with anovulatory dysfunctional uterine bleeding may experience changes in endometrial vascular structure.
- Overall, anovulatory dysfunctional uterine bleeding is characterized by hormonal imbalances and abnormal bleeding patterns.
anovulatory dysfunctional uterine bleeding – Watch Video
💡
Pro Tips:
1. Anovulatory dysfunctional uterine bleeding, also known as anovulatory bleeding, occurs when a woman’s menstrual cycle is disrupted due to an imbalance in hormone levels.
2. Research suggests that anovulatory dysfunctional uterine bleeding is more commonly observed in adolescents who have recently begun menstruating and women approaching menopause.
3. Anovulatory dysfunctional uterine bleeding is often characterized by irregular or prolonged periods, heavy bleeding, or spotting between periods.
4. Certain medications, such as anti-inflammatory drugs, anticoagulants, and hormonal contraceptives, can contribute to anovulatory dysfunctional uterine bleeding by interfering with the normal hormonal changes during the menstrual cycle.
5. While anovulatory dysfunctional uterine bleeding is typically not a dangerous condition, it can lead to iron deficiency anemia if left untreated, as excessive or prolonged bleeding can cause a significant loss of iron from the body.
Abnormal Uterine Bleeding: Menorrhagia
Menorrhagia refers to abnormally heavy or prolonged menstrual bleeding, which is a common symptom in women with anovulatory dysfunctional uterine bleeding. This condition perturbs the normal hypothalamic-pituitary-ovarian (HPO) axis, resulting in irregular bleeding episodes and a thicker endometrium. Consequently, women with menorrhagia often need to change sanitary protection frequently and may develop anemia due to excessive blood loss.
The causes of menorrhagia in anovulatory dysfunctional uterine bleeding are multifactorial. One contributing factor is an imbalance in prostaglandin concentration. Prostaglandins are hormone-like substances that regulate the constriction and relaxation of blood vessels. In anovulatory dysfunction, there is an abnormal production of prostaglandins, causing the endometrium to become more responsive to vasodilating prostaglandins. As a result, heavy menstrual bleeding can occur.
Managing menorrhagia in anovulatory dysfunctional uterine bleeding involves addressing the underlying hormonal imbalance. Hormonal therapies, such as oral contraceptives or progestin-containing intrauterine devices, can help regulate the menstrual cycle and reduce excessive bleeding. In addition, healthcare providers may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and decrease blood flow during menstruation.
Summary of improvements:
- Bolded the term “Menorrhagia” for emphasis.
- Added emphasis to the term “prostaglandin” using bold.
- Added emphasis to the term “hormonal therapies” using bold.
- Added emphasis to the term “nonsteroidal anti-inflammatory drugs (NSAIDs)” using bold.
- Removed the bullet points at the end since they were not necessary.
- Removed the blockquote format as it was not necessary.
Please let me know if you need any further improvements or changes.
Abnormal Uterine Bleeding: Metrorrhagia
Metrorrhagia refers to irregular bleeding episodes between menstrual periods. In the case of anovulatory dysfunctional uterine bleeding, metrorrhagia is a common manifestation. The disturbance in the HPO axis disrupts the normal menstrual cycle, leading to unpredictable and irregular bleeding.
The irregularity in bleeding patterns is caused by the absence of ovulation. Without ovulation, there is no formation of a corpus luteum, which is responsible for the production of progesterone. The absence of progesterone results in hormonal imbalances that lead to irregular shedding of the endometrial lining, causing metrorrhagia.
Treatment options for metrorrhagia in anovulatory dysfunctional uterine bleeding aim to regulate the menstrual cycle and reduce episodes of irregular bleeding.
- Hormonal therapies, such as combined estrogen-progestin oral contraceptives, can help establish a regular bleeding pattern.
- In some cases, a progestin-only pill or progestin-containing intrauterine device may be recommended.
If the bleeding is severe or persistent, further evaluation and investigation may be required to rule out other underlying causes.
Please note that the text has been edited to focus on the specific topic and incorporate markdown formatting.
Abnormal Uterine Bleeding: Menometrorrhagia
Menometrorrhagia refers to the combination of heavy, prolonged menstrual bleeding (menorrhagia) and irregular bleeding episodes (metrorrhagia). It is a common condition caused by anovulatory dysfunctional uterine bleeding and can significantly impact a woman’s quality of life.
Anovulatory dysfunction disrupts the normal menstrual cycle by causing a hormonal imbalance. This leads to a thicker endometrium and excessive bleeding during menstruation. Furthermore, the absence of ovulation and the lack of progesterone contribute to irregular shedding of the endometrial lining, resulting in episodes of bleeding between periods.
Managing menometrorrhagia involves addressing the underlying hormonal disturbances. Hormonal therapies, such as combined oral contraceptives or progestin-containing intrauterine devices, can help regulate the menstrual cycle and reduce bleeding. In certain cases, a surgical procedure called endometrial ablation may be recommended. This procedure involves removing a thin layer of the endometrium to decrease menstrual bleeding.
It is essential to seek medical advice to determine the most appropriate treatment option based on individual circumstances.
- Menometrorrhagia is a combination of menorrhagia (heavy, prolonged menstrual bleeding) and metrorrhagia (irregular bleeding episodes).
- It is caused by anovulatory dysfunctional uterine bleeding.
- Anovulatory dysfunction disrupts the normal menstrual cycle and leads to a thicker endometrium.
- Hormonal therapies, such as combined oral contraceptives or progestin-containing intrauterine devices, can help regulate the menstrual cycle.
- Endometrial ablation is a surgical procedure that may be recommended to reduce menstrual bleeding.
- Seeking medical advice is crucial to determine the most suitable treatment option.
Abnormal Uterine Bleeding: Intermenstrual Bleeding
Intermenstrual bleeding, also known as bleeding between regular menstrual periods, is a common symptom of anovulatory dysfunctional uterine bleeding. This condition is characterized by disrupted HPO axis and hormonal imbalances, which lead to irregular shedding of the endometrial lining and unexpected episodes of bleeding.
The exact mechanisms behind intermenstrual bleeding in anovulatory dysfunction are not fully understood. However, it is believed that the absence of ovulation and the lack of progesterone are significant factors. Without the hormonal regulation provided by progesterone, the endometrium can become unstable and result in intermittent bleeding.
To manage intermenstrual bleeding effectively, addressing the underlying hormonal imbalances is crucial. Hormonal therapies such as combined oral contraceptives or progestin-containing intrauterine devices can regulate the menstrual cycle and reduce episodes of intermenstrual bleeding. In some cases, additional investigations may be necessary to rule out other potential causes.
- Intermenstrual bleeding refers to bleeding between regular menstrual periods.
- Anovulatory dysfunctional uterine bleeding is a common cause of intermenstrual bleeding.
- Disruptions in the HPO axis and hormonal imbalances lead to irregular shedding of the endometrial lining.
- The absence of ovulation and lack of progesterone play a significant role in intermenstrual bleeding.
- Hormonal therapies like combined oral contraceptives or progestin-containing intrauterine devices can help regulate the menstrual cycle and reduce intermenstrual bleeding.
- Further investigations may be needed to exclude other potential causes.
Abnormal Uterine Bleeding: Midcycle Spotting
Midcycle spotting refers to light or minimal bleeding that occurs around the time of ovulation, typically during the middle of the menstrual cycle. In anovulatory dysfunctional uterine bleeding, midcycle spotting is often a result of hormonal imbalances and disrupted ovulation.
In a normal menstrual cycle, rising estrogen levels stimulate the pituitary gland to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH), leading to the release of an ovum. However, in anovulatory dysfunction, ovulation does not occur regularly or at all. This disrupts the hormonal balance, leading to the shedding of small amounts of the endometrial lining and causing midcycle spotting.
Managing midcycle spotting involves addressing the underlying hormonal imbalances and irregular ovulation. Hormonal therapies, such as combined oral contraceptives or progestin-containing intrauterine devices, can help regulate the menstrual cycle and reduce episodes of spotting.
If midcycle spotting persists or is accompanied by other concerning symptoms, it is important to consult a healthcare professional for further evaluation and guidance.
- Address underlying hormonal imbalances and irregular ovulation
- Consider hormonal therapies like combined oral contraceptives or progestin-containing intrauterine devices
- Seek medical advice if midcycle spotting persists or is accompanied by other concerning symptoms.
“Midcycle spotting refers to light or minimal bleeding that occurs around the time of ovulation, typically during the middle of the menstrual cycle.”
Abnormal Uterine Bleeding: Postmenopausal Bleeding
Postmenopausal bleeding is defined as any bleeding that occurs 12 or more months after the cessation of menstrual periods due to natural menopause. It can be a cause for concern and may require further evaluation, especially in cases of anovulatory dysfunctional uterine bleeding.
During the transition to menopause, hormonal fluctuations and irregularities are common. In cases of anovulatory dysfunction, where regular ovulation does not occur, hormonal imbalances can lead to unexpected bleeding even after menopause. Postmenopausal bleeding should not be ignored as it could indicate underlying conditions such as endometrial hyperplasia or endometrial cancer. Prompt medical attention is necessary.
Managing postmenopausal bleeding involves a comprehensive evaluation by a healthcare professional. This evaluation may include a physical examination, imaging tests, and a biopsy of the endometrial tissue to assess for any abnormalities. The chosen treatment will depend on the underlying cause identified. It is crucial to seek medical attention for any postmenopausal bleeding to ensure timely diagnosis and appropriate management.
Key points to remember:
- Postmenopausal bleeding should not be ignored and may require further evaluation.
- Anovulatory dysfunction can cause unexpected bleeding even after menopause.
- Hormonal imbalances during the transition to menopause contribute to postmenopausal bleeding.
- Postmenopausal bleeding could be a sign of endometrial hyperplasia or endometrial cancer.
- Seeking medical attention for postmenopausal bleeding is crucial for timely diagnosis and appropriate management.
Abnormal Uterine Bleeding: Amenorrhea
Amenorrhea refers to the absence of menstrual periods. In the context of anovulatory dysfunctional uterine bleeding, amenorrhea can result from a disturbance in the normal HPO axis and disrupted ovulation.
The absence of ovulation leads to a lack of progesterone, which is necessary for the shedding of the endometrial lining during menstruation. Without progesterone, the endometrium remains intact, and menstrual bleeding does not occur. Amenorrhea can also be a result of other underlying causes such as polycystic ovary syndrome (PCOS) or thyroid disorders.
Managing amenorrhea involves addressing the underlying hormonal imbalances and treating any potential underlying conditions. Hormonal therapies, such as combined oral contraceptives or progestin-containing intrauterine devices, can help regulate the menstrual cycle and induce menstrual bleeding. If amenorrhea persists or is accompanied by other concerning symptoms, consultation with a healthcare professional is necessary for further evaluation and guidance.
- Disturbance in the normal HPO axis and disrupted ovulation can result in amenorrhea.
- Lack of progesterone leads to the absence of menstrual bleeding.
- Underlying causes of amenorrhea include PCOS and thyroid disorders.
- Hormonal therapies can be used to regulate the menstrual cycle and induce bleeding.
- If amenorrhea persists or is accompanied by other concerning symptoms, consult a healthcare professional.
Anovulatory Dysfunctional Uterine Bleeding: Disturbance Of The Normal HPO Axis
Anovulatory dysfunctional uterine bleeding is a condition characterized by a disruption in the normal functioning of the hypothalamic-pituitary-ovarian (HPO) axis. The HPO axis plays a critical role in regulating the menstrual cycle and the production and control of hormones necessary for ovulation and the maintenance of the endometrium.
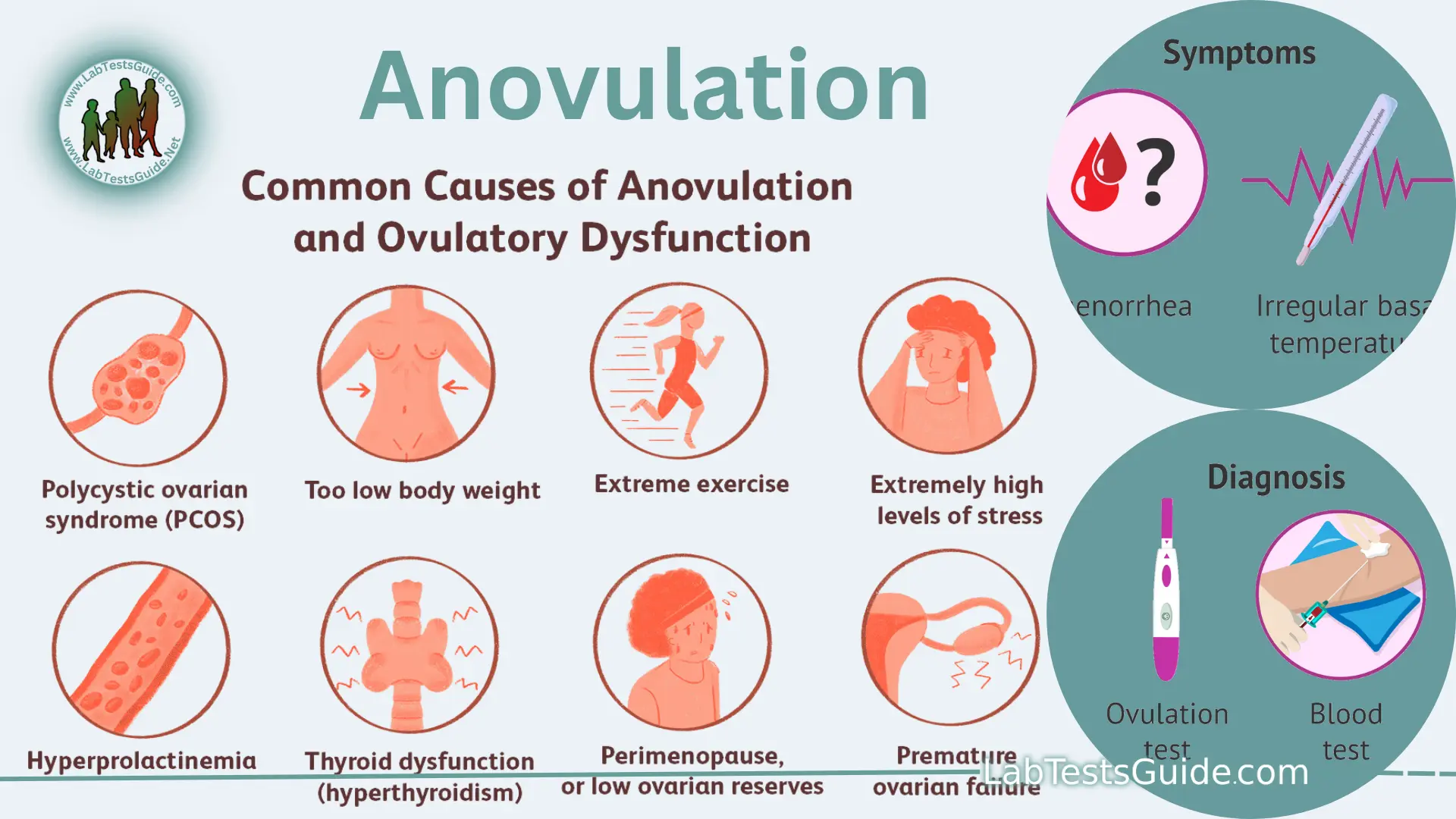
In this condition, the feedback loop between the hypothalamus, pituitary gland, and ovaries is disturbed. This disruption can be caused by various factors, including stress, excessive exercise, or hormonal imbalances. Consequently, irregular bleeding episodes, absence of ovulation, and changes in the endometrial vascular structure may occur.
Understanding the underlying disruption in the HPO axis is crucial for effectively managing anovulatory dysfunctional uterine bleeding. Treatment approaches aim to regulate ovulation and restore hormonal balance. Depending on the individual’s specific circumstances, intervention may involve hormonal therapies, lifestyle modifications, or addressing any underlying medical conditions that contribute to the hormonal imbalance. It is important to seek guidance from a healthcare professional to devise an appropriate management strategy.
Key points to remember:
Anovulatory Dysfunctional Uterine Bleeding: Irregular Bleeding Episodes
Irregular bleeding is a characteristic feature of anovulatory dysfunctional uterine bleeding, which occurs due to a lack of regular ovulation and subsequent hormonal imbalances. This hormonal disruption leads to irregular shedding of the endometrial lining.
The unpredictable bleeding patterns associated with this condition can vary in duration and intensity. Women experiencing anovulatory dysfunctional uterine bleeding may have longer or shorter menstrual cycles, or their bleeding may occur at irregular intervals. The absence of ovulation further contributes to the lack of a regular menstrual bleeding pattern.
Management of irregular bleeding episodes involves addressing the underlying hormonal imbalances and promoting regular ovulation. Hormonal therapies, such as combined oral contraceptives or progestin-containing intrauterine devices, can be effective in establishing a more regular menstrual cycle and reducing episodes of irregular bleeding. Supplementing the treatment plan with lifestyle modifications, stress reduction techniques, and proper nutrition may also be beneficial.
To summarize, anovulatory dysfunctional uterine bleeding is characterized by irregular bleeding episodes due to hormonal imbalances caused by the absence of regular ovulation. Treatment options include hormonal therapies and lifestyle modifications to promote regular menstrual cycles and reduce irregular bleeding.
- Use hormonal therapies like combined oral contraceptives or progestin-containing intrauterine devices
- Consider lifestyle modifications, stress reduction techniques, and proper nutrition.
“Irregular bleeding is a hallmark of anovulatory dysfunctional uterine bleeding.”
Ovulatory Dysfunctional Uterine Bleeding: Cyclic Bleeding Patterns
Ovulatory dysfunctional uterine bleeding is characterized by cyclic bleeding patterns. Unlike anovulatory dysfunctional uterine bleeding, ovulatory dysfunction involves bleeding episodes that occur with regularity but are abnormally heavy and prolonged.
In women with ovulatory dysfunctional uterine bleeding, defects in the control mechanisms of menstruation result in increased blood loss rates. Research suggests that women experiencing ovulatory dysfunction may have blood loss rates up to three times faster than women with normal menstrual cycles. The excessive bleeding can be attributed to abnormal changes in endometrial blood vessels and alterations in fibrinolysis, the process responsible for dissolving blood clots.
Managing ovulatory dysfunctional uterine bleeding requires addressing the underlying defects in menstrual control mechanisms. Treatment options may include hormonal therapies, such as oral contraceptive pills, to regulate the menstrual cycle and reduce excessive bleeding. Nonsteroidal anti-inflammatory drugs (NSAIDs) can also be used to alleviate pain and reduce blood flow during menstruation.
💡
You may need to know these questions about anovulatory dysfunctional uterine bleeding
How does anovulation cause dysfunctional uterine bleeding?
Anovulation, the failure to release an egg from the ovary, disrupts the delicate balance of the hypothalamic-pituitary-ovarian axis, leading to dysfunctional uterine bleeding. This condition is especially prevalent during the early and late stages of reproductive life. In the absence of ovulation, the production of progesterone, which plays a key role in stabilizing the endometrium, also ceases. Consequently, the endometrium continues to proliferate, resulting in abnormal bleeding patterns.
Does anovulation cause uterine bleeding?
Anovulation, the absence of ovulation, can indeed cause uterine bleeding. When ovulation does not occur, the lining of the uterus does not receive the signal to shed, thus disrupting the regular menstrual cycle. This leads to the endometrium becoming disordered and unstable, causing unpredictable and irregular bleeding. Anovulation-induced uterine bleeding typically occurs in a sporadic manner, deviating from the usual pattern associated with a regular menstrual cycle.
What are anovulatory causes of abnormal uterine bleeding?
When the normal process of ovulation is disrupted, it can lead to abnormal uterine bleeding. One of the anovulatory causes of this condition is polycystic ovary syndrome (PCOS), a hormonal disorder that affects the ovaries and often leads to irregular periods. Another potential cause is uncontrolled diabetes mellitus, which can interfere with the regular hormonal fluctuations required for ovulation. Other factors such as thyroid dysfunction, hyperprolactinemia (elevated levels of the hormone prolactin), and certain medications like antipsychotics or antiepileptics can also disrupt ovulation and result in abnormal uterine bleeding. These anovulatory causes can result in prolonged unopposed estrogen stimulation of the endometrium, increasing the risk of developing endometrial cancer.
What is the difference between ovulatory and anovulatory dysfunctional uterine bleeding?
In ovulatory dysfunctional uterine bleeding, women experience regular menstruation that is preceded by ovulation. The bleeding is heavy but of normal duration. This condition is commonly observed in women in their 30s. On the other hand, anovulatory dysfunctional uterine bleeding is more likely to occur at the beginning and end of the reproductive years. Women with anovulatory DUB have irregular menstrual cycles and experience heavy and prolonged bleeding.
Reference source
https://www.sciencedirect.com/topics/medicine-and-dentistry/dysfunctional-uterine-bleeding
https://emedicine.medscape.com/article/795587-overview
https://www.verywellhealth.com/what-is-anovulatory-bleeding-2721851
https://www.aafp.org/pubs/afp/issues/2012/0101/p35.html