Cervical cancer, a silent but deadly disease, lurks in the shadows, striking women without warning.
Yet, there is hope amidst the darkness.
Through screening and vaccination, we can unveil the enemy’s presence and conquer it.
Join us on a journey to uncover the secrets of cervical cancer and understand why early detection is our greatest weapon against it.
cancer of cervix
Cervical cancer is the growth of abnormal cells in the lining of the cervix.
It is primarily caused by persistent infection with high-risk types of HPV.
Common signs of cervical cancer include vaginal bleeding between periods, pain during intercourse, and changes in vaginal discharge.
Diagnosis involves a colposcopy with biopsy to locate and examine abnormal cells.
Treatment options depend on the stage of the disease and range from surgery to chemotherapy and radiation therapy.
The introduction of the National Cervical Screening Program and HPV vaccine has contributed to a decrease in the incidence of cervical cancer in Australia.
Timely detection and treatment can effectively treat cervical cancer, although fertility may be impacted.
Key Points:
- Cervical cancer is caused by the growth of abnormal cells in the lining of the cervix.
- Persistent infection with high-risk types of HPV is the primary cause of cervical cancer.
- Common signs of cervical cancer include vaginal bleeding between periods, pain during intercourse, and changes in vaginal discharge.
- Diagnosis involves a colposcopy with biopsy to locate and examine abnormal cells.
- Treatment options for cervical cancer range from surgery to chemotherapy and radiation therapy, depending on the stage of the disease.
- The introduction of the National Cervical Screening Program and HPV vaccine has contributed to a decrease in the incidence of cervical cancer in Australia.
cancer of cervix – Watch Video
💡
Pro Tips:
1. In the early twentieth century, there was a widespread misconception that cervical cancer was caused by bicycle riding. This unfounded belief led to the implementation of measures such as creating special bicycle seats with holes, which were thought to reduce the risk of developing the disease.
2. An unusual risk factor for cervical cancer is the use of talcum powder in the genital area. Research has suggested that talcum powder particles can travel up the female reproductive tract, potentially increasing the risk of cancer development in the cervix.
3. The human papillomavirus (HPV) is the primary cause of cervical cancer. There are more than 200 known types of HPV, but only a few high-risk strains, such as HPV 16 and 18, are strongly associated with the development of cervical cancer.
4. Some studies have indicated that long-term use of certain hormonal contraceptives, such as birth control pills, may slightly increase the risk of developing cervical cancer. However, the overall benefits of contraception in preventing unwanted pregnancies often outweigh the minor increase in cancer risk.
5. Cervical cancer is one of the most preventable types of cancer. Regular screenings, such as Pap smears or HPV tests, can detect pre-cancerous changes in the cervix, allowing for early intervention and treatment.
Types Of Cervical Cancer: Squamous Cell Carcinoma And Adenocarcinoma
Cervical cancer can be classified into different types based on the specific cells that are affected. The most common type is squamous cell carcinoma, accounting for approximately 70% of cervical cancer cases. Squamous cells are thin, flat cells that cover the outer surface of the cervix. Adenocarcinoma is another type of cervical cancer, although less common, accounting for around 25% of cases. Adenocarcinoma develops in the glandular cells that line the cervical canal.
Incidence Of Cervical Cancer In 2023: Over 900 Cases
According to recent data, over 900 people were diagnosed with cervical cancer in 2023 in Australia alone. The average age of diagnosis is around 50 years old. These numbers highlight the importance of early detection and prevention strategies to reduce the burden of cervical cancer on women’s lives.
Decrease In Cervical Cancer Rates Since National Screening And HPV Vaccine Programs
Fortunately, the incidence of cervical cancer has decreased in recent years, thanks to the implementation of the National Cervical Screening Program in 1991 and the national HPV vaccine program in 2007. These initiatives have played a significant role in raising awareness about cervical cancer and promoting regular screenings and vaccinations. The introduction of these programs has led to a decline in the number of cases, emphasizing the importance of preventive measures in combating cervical cancer.
- The incidence of cervical cancer has decreased in recent years.
- The National Cervical Screening Program was implemented in 1991.
- The national HPV vaccine program was introduced in 2007.
- These initiatives have raised awareness about cervical cancer.
- Regular screenings and vaccinations are promoted.
- The number of cases has declined.
Signs Of Cervical Cancer: Bleeding, Pain, And Changes In Discharge
Identifying the signs and symptoms of cervical cancer is crucial for early detection. Women should be aware of the following warning signs:
- Vaginal bleeding between periods
- Longer or heavier menstrual bleeding
- Pain during intercourse
- Bleeding after intercourse
- Pelvic pain
- Changes in vaginal discharge
- Vaginal bleeding after menopause
Experiencing any of these symptoms should prompt women to seek medical attention for further evaluation.
HPV Infection As The Primary Cause Of Cervical Cancer
Persistent infection with high-risk types of human papillomavirus (HPV) is the primary cause of almost all cases of cervical cancer. HPV is a common sexually transmitted infection that can lead to abnormal cell growth in the cervix. It is important to note that not all women infected with HPV will develop cervical cancer, but the risk increases significantly with a prolonged infection.
Regular screenings and HPV vaccinations are crucial to reduce the risk of developing cervical cancer associated with HPV infection.
- Persistent infection with high-risk types of HPV is the primary cause of almost all cases of cervical cancer
- HPV is a common sexually transmitted infection that can lead to abnormal cell growth in the cervix
- Not all women infected with HPV will develop cervical cancer, but the risk increases significantly with a prolonged infection
- Regular screenings and HPV vaccinations are crucial to reduce the risk of developing cervical cancer associated with HPV infection.
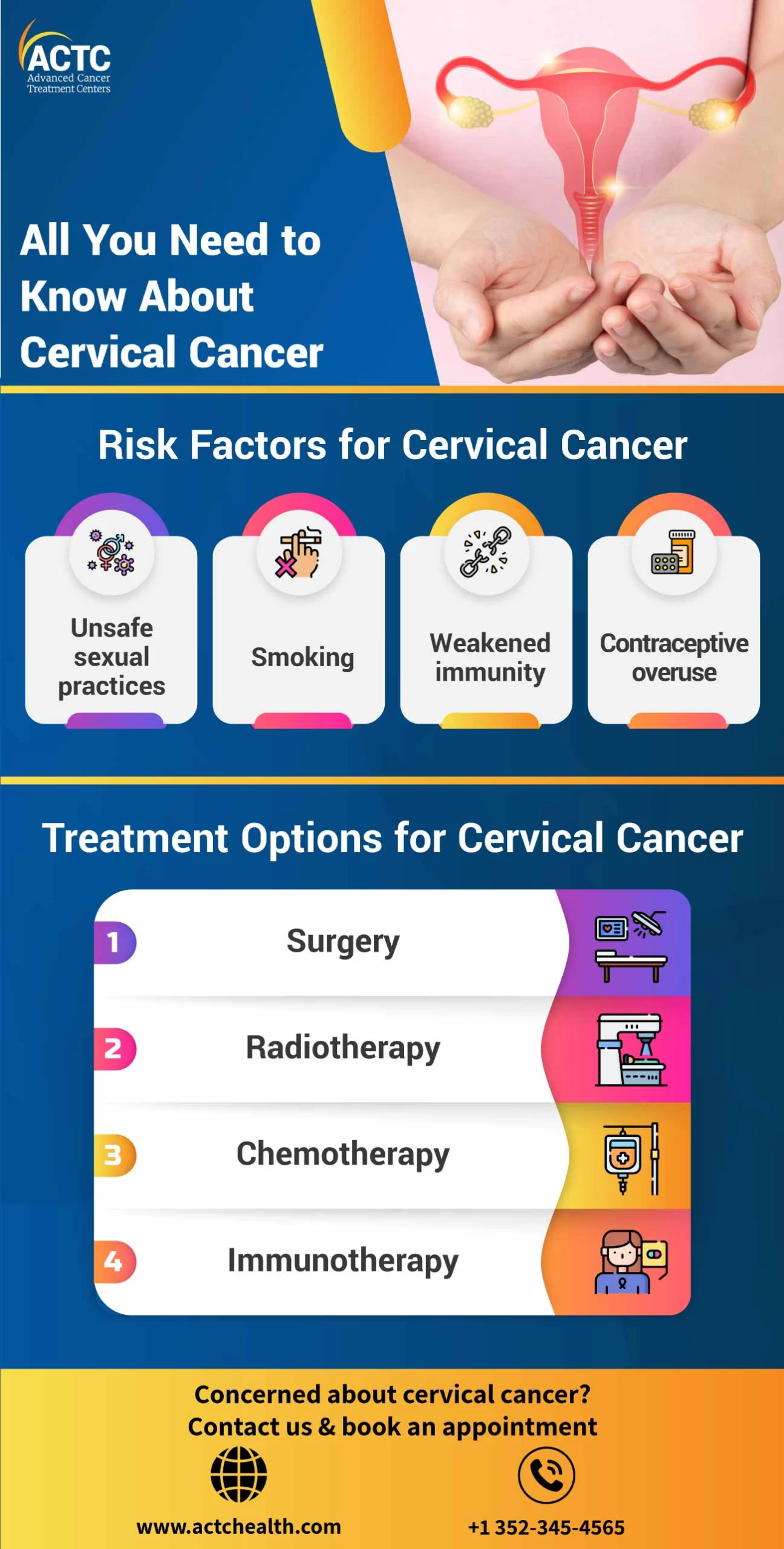
Other Risk Factors For Cervical Cancer: Smoking And Contraceptive Pill Use
While HPV infection is the leading cause of cervical cancer, other risk factors can also contribute to its development. Smoking has been identified as a significant risk factor, as the chemicals present in tobacco can damage the DNA of cervical cells, increasing the likelihood of cancerous changes. Additionally, long-term use of the contraceptive pill has been associated with a slightly increased risk of cervical cancer.
To summarize:
- HPV infection is the leading cause of cervical cancer.
- Smoking is a significant risk factor, as it can damage cervical cells’ DNA.
- Long-term use of the contraceptive pill is associated with a slightly increased risk.
It is important for women to be aware of these risk factors and discuss them with their healthcare providers.
Diagnosis Of Cervical Cancer: Colposcopy With Biopsy
To diagnose cervical cancer, doctors perform a colposcopy with biopsy. This procedure involves using a specialized microscope called a colposcope to closely examine the cervix. If any abnormal areas are detected, a small sample of tissue is collected for further analysis. The biopsy is crucial in identifying cancerous cells and obtaining information about the stage of the disease.
- Doctors perform a colposcopy with biopsy to diagnose cervical cancer.
- A colposcope, a special microscope, is used during this procedure.
- Abnormal areas found during the colposcopy are further analyzed.
- The biopsy helps in determining the presence of cancerous cells.
- It also provides information about the stage of the disease.
Treatment Options For Cervical Cancer: Surgery, Chemotherapy, And Radiation Therapy
Treatment options for cervical cancer depend on various factors, such as the stage of the disease and the patient’s overall health. Common treatment modalities include surgery, chemotherapy, and radiation therapy.
- Early-stage cervical cancer can often be effectively treated with surgery, such as a hysterectomy, where the uterus and cervix are removed.
- In advanced cases, combinations of chemotherapy and radiation therapy may be recommended to target cancerous cells and prevent their spread.
It is important to consider individual circumstances and consult with a healthcare professional to determine the most appropriate treatment plan for each patient.
- Surgery: Hysterectomy is a common surgical procedure for treating early-stage cervical cancer. It involves the removal of the uterus and cervix.
- Chemotherapy: The use of drugs to kill cancer cells or stop them from growing. It is often used in combination with other treatments for advanced cervical cancer.
- Radiation therapy: High-energy radiation beams are directed at the cancer cells to destroy them. It can be administered externally or internally.
Remember, treatment decisions should be made in consultation with a healthcare professional, taking into account the specific stage of cervical cancer and the patient’s overall health.
Transition From Pap Smear To Cervical Screening Test
In Australia, the Pap smear test has been replaced by the new Cervical Screening Test. This test is more accurate in detecting high-risk HPV infections, which can lead to cervical cancer. It is recommended for women aged 25 to 74 years, and routine screening intervals have changed from two to five years. The transition to the Cervical Screening Test reflects advancements in technology and a better understanding of HPV-related cervical abnormalities.
Australia’s Efforts To Eliminate Cervical Cancer: HPV Vaccine And National Screening Program
Australia is committed to being the first country to eliminate cervical cancer as a public health issue. The national HPV vaccine program has been instrumental in preventing cervical cancer. This program offers the Gardasil 9 vaccine, which protects against nine types of HPV, covering around 90% of cervical cancer cases. It is currently offered to Australian children aged 12 to 13 for free.
However, it is important to note that vaccination does not replace the need for regular cervical cancer screenings. The National Cervical Screening Program, along with the HPV vaccine initiative, plays a critical role in reducing the incidence and mortality rates associated with cervical cancer in Australia.
Cervical cancer is a serious health concern that affects many women globally. Understanding its causes, symptoms, prevention strategies, and treatment options is imperative to ensure early detection and effective management. Regular screenings and the HPV vaccine have played a pivotal role in decreasing the incidence of cervical cancer.
Australia’s commitment to eliminating cervical cancer highlights the significance of preventive measures and further research in this area. By prioritizing awareness, screening, and vaccination, we can continue to progress towards a future where cervical cancer is no longer a public health issue.
💡
You may need to know these questions about cancer of cervix
What are the 5 warning signs of cervical cancer?
Cervical cancer presents several warning signs that should be promptly addressed. Firstly, vaginal bleeding after sex can be an indication of cervical cancer. Secondly, another warning sign is vaginal bleeding after menopause. Additionally, any vaginal bleeding between periods or experiencing periods that are heavier or longer than usual should not be ignored. Moreover, the presence of watery vaginal discharge with a strong odor or blood should raise concerns. Lastly, pelvic pain or pain during sex can also be a potential warning sign of cervical cancer. If any of these signs are experienced, it is essential to consult a healthcare professional for further evaluation and appropriate management.
How serious is cervical cancer?
Cervical cancer is a potentially serious and life-threatening condition, with the severity varying depending on the stage of diagnosis. When detected early, the 5-year relative survival rate is 91%, indicating a relatively favorable prognosis. However, if the cancer has spread to nearby tissues, organs, or lymph nodes, the survival rate drops to 60%, highlighting the increased seriousness and challenges associated with advanced stages of the disease. Timely detection and appropriate treatment are crucial in improving outcomes and increasing survival rates for individuals affected by cervical cancer.
Is cervical cancer usually curable?
Cervical cancer is typically considered curable, especially if detected early. By diagnosing the cancer at an early stage, medical intervention can focus on preventing the spread of cancer cells. Treatment options may include surgical removal of the cancerous cells or radiation therapy, increasing the likelihood of a successful outcome. Regular screenings and awareness are crucial in detecting cervical cancer at its earliest stages for effective treatment and a higher chance of a cure.
It is important to note that the curability of cervical cancer depends on various factors, such as the stage and aggressiveness of the cancer, as well as the individual’s overall health. While early detection and intervention offer a high probability of a cure, advanced or metastasized cases may be more challenging to treat. Regular check-ups and awareness about the symptoms are vital in maintaining overall reproductive health and safeguarding against cervical cancer.
What are the symptoms of Stage 1 cervical cancer?
In Stage 1 cervical cancer, symptoms may include vaginal bleeding during or after sexual intercourse, as well as abnormal bleeding at any other time of the month. It is important to note that this includes bleeding after menopause, which is typically a cessation of monthly periods. Identifying these unusual bleeding patterns is crucial for prompt diagnosis and treatment of Stage 1 cervical cancer. Regular gynecological check-ups and awareness of changes in menstrual patterns can contribute to early detection, potentially increasing the chances of successful treatment and recovery.
Reference source
https://www.cancer.org.au/cancer-information/types-of-cancer/cervical-cancer
https://www.cancer.gov/types/cervical/symptoms
https://www.cancer.gov/types/cervical/survival
https://www.moffitt.org/cancers/cervical-cancer/faqs/how-treatable-is-cervical-cancer/