Vaginal discomfort?
Unusual discharge?
Ladies, listen up!
Candida albicans vaginitis might be the culprit behind these pesky symptoms.
But fear not!
In this succinct read, we’ll unveil the secrets of this common infection and how you can banish it with the power of antifungal medication.
Get ready to take back control!
candida albicans vaginitis
Candida albicans vaginitis, also known as vaginal candidiasis, is a common infection caused by a yeast called Candida.
It occurs when there is an overgrowth of Candida in the vagina, typically due to hormonal changes or a weakened immune system.
Symptoms include itching, soreness, pain during sex or urination, and abnormal discharge.
Risk factors for developing vaginal candidiasis include pregnancy, contraceptive use, diabetes, a weakened immune system, and recent antibiotic use.
Diagnosis is usually done by examining a sample of vaginal discharge.
Treatment involves using antifungal medication, either applied inside the vagina or taken orally.
Severe or recurrent infections may require additional treatments.
Key Points:
- Candida albicans vaginitis is a common infection caused by yeast called Candida.
- It is characterized by an overgrowth of Candida in the vagina due to hormonal changes or a weakened immune system.
- Symptoms include itching, soreness, pain during sex or urination, and abnormal discharge.
- Risk factors for developing vaginal candidiasis include pregnancy, contraceptive use, diabetes, weakened immune system, and recent antibiotic use.
- Diagnosis is typically done by examining a sample of vaginal discharge.
- Treatment involves antifungal medication applied inside the vagina or taken orally, with additional treatments for severe or recurrent infections.
candida albicans vaginitis – Watch Video
💡
Pro Tips:
1. Candida albicans, the fungus responsible for vaginitis, was first identified and named in 1923 by a French mycologist named Christine Marie Berkhout.
2. It is estimated that approximately 75% of all women will experience at least one episode of Candida albicans vaginitis in their lifetime.
3. Despite being commonly referred to as a yeast infection, Candida albicans is actually a type of fungus that naturally resides in small amounts within the vagina of most women.
4. Candida albicans vaginitis can potentially be sexually transmitted, although the risk of transmission is relatively low compared to other sexually transmitted infections.
5. Certain factors such as pregnancy, the use of antibiotics, diabetes, or a weakened immune system can increase the likelihood of developing Candida albicans vaginitis.
Introduction to Candida Albicans Vaginitis
Candida albicans vaginitis, also known as vaginal candidiasis, is a common infection caused by a yeast called Candida. Candida is a type of fungus that normally resides on the skin and inside the body without causing any harm. However, certain factors can disrupt the balance of microorganisms in the vagina, leading to an overgrowth of Candida and resulting in an infection.
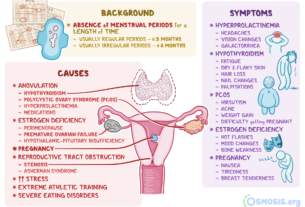
Causes: Vaginal candidiasis can be caused by various factors, including antibiotic use, pregnancy, chronic health conditions, weakened immune system, uncontrolled diabetes, hormonal changes, high estrogen levels, and sexual activity.
Symptoms: Common symptoms of vaginal candidiasis include itching, burning, redness, swelling, abnormal discharge, and painful urination.
Risk Factors: Certain factors increase the risk of developing vaginal candidiasis, such as frequent antibiotic use, unprotected sex, pregnancy, uncontrolled diabetes, and use of hormonal contraceptives.
Preventive Measures: To prevent vaginal candidiasis, it is recommended to maintain proper hygiene, avoid douching, wear breathable underwear, avoid tight-fitting clothes, limit the use of antibiotics, and avoid unnecessary use of hormonal contraceptives.
Prevalence: Vaginal candidiasis is a widespread condition that affects many women worldwide. It is estimated that about 75% of women will experience vaginal candidiasis at least once in their lifetime.
Diagnosis: Diagnosis of vaginal candidiasis is usually based on the symptoms, a physical examination, and laboratory tests, such as a vaginal swab culture.
Treatment Options: Antifungal medications are commonly used to treat vaginal candidiasis. These medications can be applied directly to the vagina, taken orally, or used as a combination of both. It is important to complete the full course of treatment to ensure the infection is fully eradicated.
It is essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment if you suspect a vaginal candidiasis infection.
Understanding Candida and Its Causes
Candida albicans is the most common type of Candida species responsible for vaginal infections. Normally, the vagina hosts a mix of bacteria and yeast, including Candida. However, when there is a disturbance in the vaginal environment, such as hormonal changes, a weakened immune system, or the use of certain medications, like antibiotics, Candida may start to grow rapidly and cause an infection. Hormonal changes during pregnancy or the menstrual cycle can create an ideal environment for Candida overgrowth.
–Candida albicans is the most common type of Candida species responsible for vaginal infections
- The vaginal environment can be disturbed by hormonal changes, a weakened immune system, or the use of certain medications like antibiotics
- Hormonal changes during pregnancy or the menstrual cycle can create an ideal environment for Candida overgrowth.
Identifying Symptoms of Vaginal Candidiasis
Symptoms of vaginal candidiasis (also known as a yeast infection) can vary, but commonly include itching, soreness, pain during sexual intercourse or urination, and abnormal discharge. The discharge is typically thick, white, and often described as being similar to cottage cheese.
In some cases, women may also experience redness and swelling of the vulva in addition to these symptoms. However, it’s important to note that not all women with Candida in their vagina experience symptoms. In fact, approximately 20% of women have Candida without any signs of infection.
If you suspect a yeast infection, it is recommended to seek medical advice for proper diagnosis and treatment.
Risk Factors for Vaginal Candidiasis
Certain factors increase the likelihood of developing a vaginal candidiasis infection. Pregnancy, use of hormonal contraceptives, uncontrolled diabetes, a weakened immune system (such as from HIV infection or chemotherapy), and recent antibiotic use are all known risk factors. Antibiotics can disrupt the balance of bacteria in the vagina, allowing Candida to grow more easily. Additionally, those who have previously had a vaginal candidiasis infection are more susceptible to recurrent episodes.
Preventive Measures for Vaginal Candidiasis
Taking preventive measures can reduce the risk of developing vaginal candidiasis. Wearing cotton underwear, which allows for better airflow and reduces moisture, can help create an environment less favorable for Candida growth. Additionally, practicing good genital hygiene, avoiding the use of scented soaps or douches, and taking antibiotics only as prescribed by a healthcare professional are important preventive measures. It is also advisable to avoid unnecessary hormonal contraceptive use and manage diabetes to reduce the risk of candidal infections.
Prevalence and Impact of Vaginal Candidiasis
Vaginal candidiasis is a prevalent condition in the United States. Candida albicans vaginitis is the second most common type of vaginal infection, following bacterial vaginal infections. More than 1.4 million outpatient visits are made each year for vaginal candidiasis. However, the actual number of cases is unknown as some women may self-treat or not seek medical attention for mild infections.
Vaginal candidiasis can greatly affect a woman’s quality of life, causing discomfort, pain, and possible disruptions in sexual activity.
Key points:
- Vaginal candidiasis is a common condition in the United States
- Candida albicans vaginitis is the second most common type of vaginal infection
- Over 1.4 million outpatient visits are made annually for vaginal candidiasis
- The actual number of cases is unknown due to self-treatment and lack of medical attention
- Can cause discomfort, pain, and disruptions in sexual activity
“Vaginal candidiasis can have a significant impact on women’s quality of life.”
Diagnosis of Vaginal Candidiasis
Diagnosing vaginal candidiasis typically involves examining a sample of vaginal discharge either under a microscope or by sending it to a laboratory for further analysis. A healthcare professional will be looking for the presence of Candida cells, as well as assessing the pH level and appearance of the discharge. Proper diagnosis is crucial as there are other vaginal infections that can present with similar symptoms. This ensures that appropriate treatment is given and prevents the unnecessary use of antifungal medications.
- Diagnosing vaginal candidiasis involves examining a sample of vaginal discharge under a microscope or sending it to a laboratory.
- Healthcare professionals may look for Candida cells, assess the pH level, and evaluate the appearance of the discharge.
- Proper diagnosis is essential to differentiate vaginal candidiasis from other similar infections.
- Confirming the diagnosis allows for appropriate treatment and prevents unnecessary use of antifungal medications.
It is important to confirm the diagnosis of vaginal candidiasis to ensure proper treatment and avoid unnecessary use of antifungal medications.
Treatment Options for Vaginal Candidiasis
The primary treatment for vaginal candidiasis is using antifungal medication. Antifungals can be applied topically in the form of creams, suppositories, or tablets, or taken orally. Common medications include fluconazole, miconazole, and clotrimazole. The choice of treatment depends on the severity of the infection, patient preference, and healthcare provider’s recommendation. It is essential to complete the full course of treatment to ensure the complete eradication of Candida and prevent recurrent episodes.
Additional Treatments for Severe or Recurrent Infections
In some cases, severe or recurrent vaginal candidiasis infections may require additional treatments. This may include longer courses of antifungal medication, alternative antifungal agents, or the use of maintenance therapy to prevent future infections. Additionally, for women with underlying conditions that contribute to Candida overgrowth, such as poorly controlled diabetes or a weakened immune system, managing these conditions effectively is crucial for preventing recurrent infections.
Gaps in Knowledge and Research on Vaginal Candidiasis
Despite the prevalence and impact of vaginal candidiasis, there are still some gaps in knowledge and research regarding this condition. Further research is required to better understand the underlying factors that contribute to Candida overgrowth and the mechanisms by which certain risk factors increase the likelihood of infection. Additionally, more studies are needed to develop better preventive measures, treatments, and strategies for managing recurrent or severe vaginal candidiasis infections.
- Vaginal candidiasis is a common infection caused by an overgrowth of Candida yeast in the vagina.
- Understanding the causes, symptoms, risk factors, preventive measures, prevalence, diagnosis, and treatment options for vaginal candidiasis is crucial for effective management of this condition.
- By taking preventive measures, seeking timely diagnosis, and following appropriate treatment, women can reduce the burden of vaginal candidiasis and maintain their overall well-being.
💡
You may need to know these questions about candida albicans vaginitis
What causes Candida albicans in female?
Candida albicans is a type of yeast that can cause infections in the vagina in females. It is typically harmless, but certain factors can lead to its overgrowth and cause an infection. One common cause is the use of antibiotics, which can disrupt the natural balance of microorganisms in the vagina, allowing Candida albicans to multiply. Additionally, a weakened immune system can make a person more susceptible to infections, including those caused by Candida albicans. Therefore, it is important for females to maintain a healthy lifestyle and be mindful of the factors that could increase their risk of developing a Candida infection.
Is Candida a yeast infection or BV?
Candida is a yeast infection, whereas BV is caused by an overgrowth of bacteria in the vagina. Candida infections occur when there is an overgrowth of the Candida fungus, while BV is the result of an imbalance in the bacteria present in the vagina. Therefore, these two conditions are distinct from each other and caused by different microorganisms.
Is candidiasis a STD?
Candidiasis, commonly known as yeast infections, is not classified as a sexually transmitted disease (STD). However, it is important to note that yeast infections can be transmitted to a partner through sexual activity. While yeast infections are typically caused by the overgrowth of candida, a type of fungus naturally found in the body, sexual contact can introduce additional yeast into the genital area, potentially leading to an infection in either partner. Hence, although candidiasis is not inherently an STD, it can be transmitted during sexual intercourse.
How can the presence of candida albicans in the vagina be confirmed and differentiated from other causes of vaginitis?
The presence of candida albicans in the vagina can be confirmed and differentiated from other causes of vaginitis through various methods. One common method is by conducting a microscopic examination of a vaginal swab. A healthcare provider can collect a sample of vaginal discharge and examine it under a microscope to identify the presence of candida albicans. The yeast cells of candida albicans will be visible in the sample.
Additionally, a culture test can also be performed to confirm the presence of candida albicans. In this test, a sample of the vaginal discharge is cultured in a laboratory to allow the yeast to grow. If candida albicans is present, it will grow and can be identified.
To differentiate candida albicans from other causes of vaginitis, such as bacterial vaginosis or trichomoniasis, further tests may be required. These tests can include pH testing, checking for the presence of clue cells, or testing for the presence of other microorganisms. Consulting with a healthcare provider is crucial for an accurate diagnosis and appropriate treatment.
Reference source
https://www.cdc.gov/std/treatment-guidelines/candidiasis.htm
https://www.medicalnewstoday.com/articles/322722
https://www.healthline.com/health/bacterial-vaginosis-vs-yeast-infection
https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html