Cervical carcinoma in situ, the precursor to cervical cancer, is a condition that demands attention.
With various treatment options available, including cutting-edge immunotherapy, the battle against this disease has taken an exciting turn.
Join us on a journey through the stages, treatments, and potential breakthroughs in the fight against cervical carcinoma in situ.
cervical carcinoma in situ
Cervical carcinoma in situ refers to a pre-cancerous condition where abnormal cells are present in the surface layer of cells lining the cervix, the lower part of the uterus.
It is classified as stage 0 according to the International Federation of Gynecology and Obstetrics (FIGO) staging system for cervical cancer.
At this stage, the cancer is confined to the surface layer and has not invaded deeper tissues.
Treatment options for cervical carcinoma in situ include local ablative measures such as cryosurgery, laser ablation, and loop excision, as well as excisional measures like conization.
In some cases, surgical removal of the uterus (total hysterectomy or radical hysterectomy) may be necessary.
Radiation therapy, including pelvic radiation therapy and brachytherapy, may also be recommended.
The choice of treatment depends on factors such as tumor size, depth of invasion, and lymph node involvement.
It is important to detect and treat cervical carcinoma in situ early to prevent its progression to advanced stages of cervical cancer.
Key Points:
- Cervical carcinoma in situ is a pre-cancerous condition with abnormal cells in the cervix.
- It is classified as stage 0 according to the FIGO staging system.
- The cancer is confined to the surface layer and has not invaded deeper tissues.
- Treatment options include local ablative measures and excisional measures.
- In some cases, surgical removal of the uterus may be necessary.
- Radiation therapy may also be recommended based on tumor factors.
cervical carcinoma in situ – Watch Video
💡
Pro Tips:
1. A study conducted in Denmark found that women diagnosed with cervical carcinoma in situ have a lower risk of developing invasive cervical cancer compared to those with invasive cervical cancer.
2. Cervical carcinoma in situ, also known as CIN 3, is considered a precancerous condition where abnormal cells are found on the surface of the cervix.
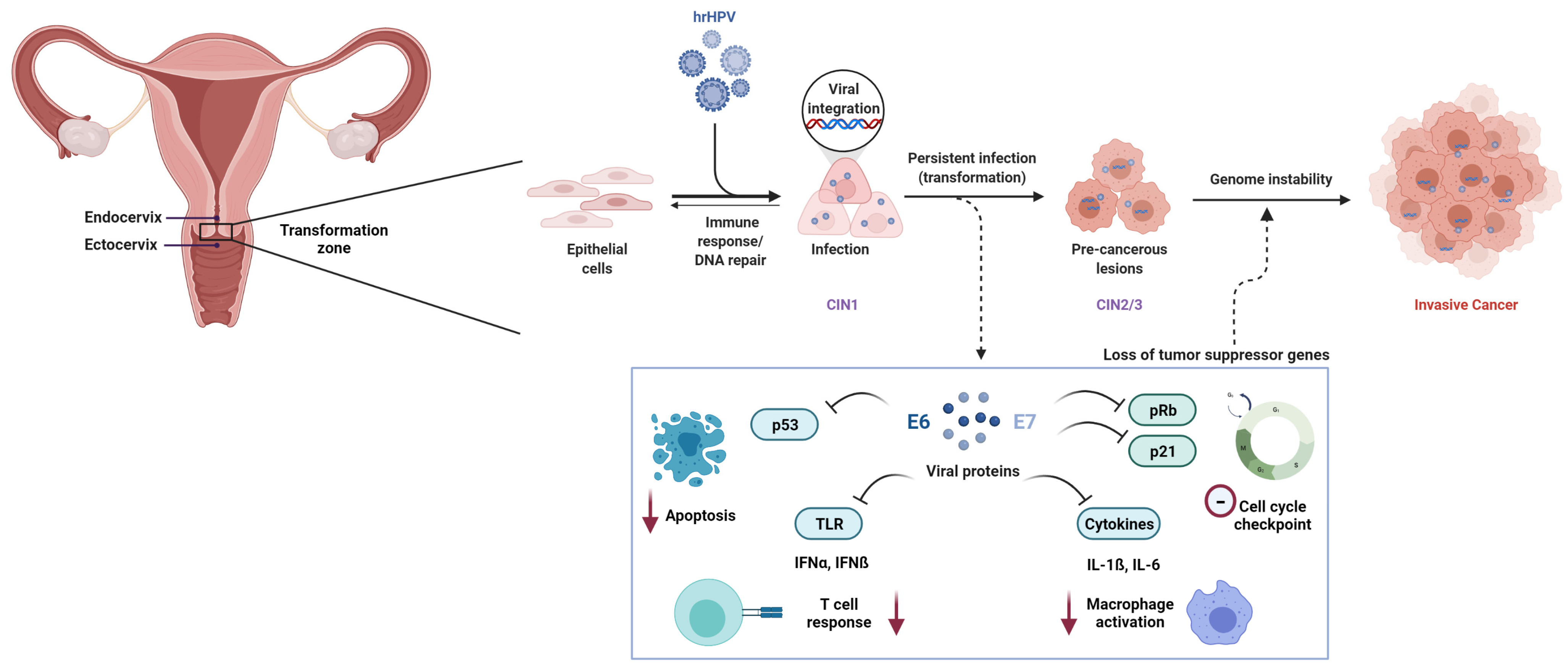
3. The human papillomavirus (HPV) is the most common cause of cervical carcinoma in situ. However, not all women infected with HPV develop the condition, as it can sometimes resolve on its own.
4. Historically, cervical carcinoma in situ was referred to as “cervical intraepithelial neoplasia grade 3” (CIN 3). The change in terminology was made to better reflect the true nature of the condition as a potential precursor to cancer.
5. Regular Pap smears and human papillomavirus (HPV) vaccinations have shown substantial success in detecting and preventing cervical carcinoma in situ, reducing the risk of it progressing to invasive cancer.
Carcinoma In Situ
Carcinoma in situ refers to the presence of abnormal cells in the surface layer of cells lining the cervix, without invasion into nearby tissues. It is considered a pre-cancerous condition, which means that if left untreated, it may progress into invasive cervical cancer. Carcinoma in situ is often detected during routine cervical cancer screening tests, such as Pap smears or HPV testing. Early detection and treatment of carcinoma in situ are crucial in preventing the development of cervical cancer.
The term “carcinoma in situ” is commonly used to describe pre-cancerous lesions in various organs, not just the cervix. It indicates that the abnormal cells have not yet invaded surrounding tissues and have the potential to become cancerous. In the case of cervical carcinoma in situ, the abnormal cells are confined to the epithelial layer of the cervix.
Cervical Cancer
Cervical cancer is a common and serious type of cancer affecting the cervix, which is the lower part of the uterus connecting to the vagina. It poses a significant public health concern worldwide, ranking as the fourth most prevalent cancer among women.
The primary cause of most cervical cancer cases stems from persistent infections with specific strains of the human papillomavirus (HPV).
To better understand the extent of the disease and guide treatment decisions, the International Federation of Gynecology and Obstetrics (FIGO) has developed a staging system for cervical cancer. This classification is based on various factors, including the size and depth of the tumor, involvement of lymph nodes, and the presence of metastasis to distant areas.
The stages of cervical cancer include:
- Stage 0: Early stage where the abnormal cells are confined to the surface of the cervix.
- Stage I: Cancer limited to the cervix but has not spread to nearby tissues or organs.
- Stage II: Cancer has progressed beyond the cervix and invaded nearby tissues or organs.
- Stage III: Cancer has spread to the lower part of the vagina or to pelvic sidewalls.
- Stage IV: Cancer has spread to distant organs or parts of the body.
In summary, cervical cancer is a prevalent disease with a significant global impact. Understanding its staging system can assist in determining the severity and appropriate treatment approach for affected individuals.
International Federation Of Gynecology And Obstetrics (FIGO)
The International Federation of Gynecology and Obstetrics (FIGO) is a nonprofit organization focused on promoting women’s health worldwide. FIGO has been instrumental in developing and standardizing guidelines for managing gynecologic cancers, notably cervical cancer. One of FIGO’s notable contributions is its staging system, which is extensively utilized by healthcare professionals to determine the severity of cervical cancer and guide treatment decisions.
FIGO’s staging system categorizes cervical cancer into different stages, taking into account factors such as tumor size, depth of invasion, lymph node involvement, and metastasis to distant sites. This system enables clinicians to provide accurate prognosis information and develop appropriate treatment plans for patients diagnosed with cervical cancer.
Staging System
The FIGO staging system is used by healthcare professionals to classify and describe the extent of cervical cancer, helping guide treatment decisions. Here are the stages:
- Stage 0: Carcinoma in situ, where abnormal cells are confined to the surface layer of cells lining the cervix.
- Stage I: Cancer is confined to the cervix.
- Stage II: Cancer has spread beyond the cervix but not to the pelvic sidewall or lower third of the vagina.
- Stage III: Cancer has invaded the pelvic sidewall or lower third of the vagina and/or has caused kidney problems.
- Stage IV: Cancer has spread to adjacent organs, like the bladder or rectum, or has metastasized to distant sites, such as the lungs, liver, brain, or bone.
The staging system provides healthcare professionals with important information about the extent and severity of the cancer, enabling them to determine the most appropriate treatment options for each patient.
Pre-Cancer
Carcinoma in situ is a pre-cancerous condition often detected during routine cervical cancer screening tests. It indicates abnormal changes in the cervix cells that can potentially lead to cancer if left untreated. Detecting and treating these pre-cancerous lesions early is crucial in preventing invasive cervical cancer.
There are several risk factors associated with the development of pre-cancerous and cancerous changes in the cervix, including:
- Infection with certain types of human papillomavirus (HPV), which is a sexually transmitted infection.
- Smoking
- A weakened immune system
- Long-term use of oral contraceptives
- Multiple sexual partners
- A history of sexually transmitted infections
Regular cervical cancer screenings, such as Pap smears or HPV testing, can help detect pre-cancerous changes early and allow for prompt treatment.
Cancer Treatment
The treatment of cervical cancer depends on the stage of the disease, tumor size and depth, lymph node involvement, and the presence of metastasis. There are several treatment options available, including:
- Local ablative measures: These include cryosurgery, laser ablation, or loop excision, which are used to destroy or remove pre-cancerous or cancerous cells.
- Surgical procedures: Conization, lymph node dissection, total hysterectomy, or radical hysterectomy may be necessary to remove the tumor or affected tissues.
- Radiation therapy: This may include pelvic radiation therapy and high-risk factors such as combined external beam radiation or brachytherapy. It can be used alone or in combination with surgery.
- Chemotherapy: Platinum-based doublet regimens or combination therapies including docetaxel, gemcitabine, ifosfamide, 5-fluorouracil, mitomycin, irinotecan, topotecan, pemetrexed, vinorelbine, or bevacizumab are commonly employed in the treatment of advanced cervical cancer.
Each treatment option carries its own risks and benefits, and the choice of treatment is based on individual patient factors, stage of cancer, and the presence of any other health conditions. It is important for patients to discuss the available treatment options with their healthcare team to make informed decisions and ensure the best possible outcomes.
- Local ablative measures: cryosurgery, laser ablation, loop excision
- Surgical procedures: conization, lymph node dissection, total hysterectomy, radical hysterectomy
- Radiation therapy: pelvic radiation therapy, combined external beam radiation, brachytherapy
- Chemotherapy: platinum-based doublet regimens, combination therapies including docetaxel, gemcitabine, ifosfamide, 5-fluorouracil, mitomycin, irinotecan, topotecan, pemetrexed, vinorelbine, bevacizumab
Advanced Cancer
Advanced cervical cancer refers to cancer that has spread beyond the cervix to nearby tissues, organs, or distant sites. It is typically classified as stage II, stage III, or stage IV, depending on the extent of spread. Advanced cancer requires more aggressive treatment approaches in order to combat the disease.
Treatment options for advanced cervical cancer may include:
- Surgery: Surgical procedures such as radical hysterectomy, extensive lymphadenectomy, or lymph node dissection may be performed to remove the tumor and affected tissues.
- Radiation therapy: Radiation therapy, including postoperative irradiation or combined external beam radiation and brachytherapy, is often administered to destroy remaining cancer cells or shrink tumors.
- Chemotherapy: Chemotherapy, using platinum-based doublet regimens or other drugs such as docetaxel, gemcitabine, ifosfamide, 5-fluorouracil, mitomycin, irinotecan, topotecan, pemetrexed, vinorelbine, or bevacizumab, may also be utilized to kill cancer cells or slow down their growth.
The treatment approach for advanced cervical cancer aims to improve overall survival, shrink tumors, alleviate symptoms, and enhance quality of life. Individualized treatment plans are created in consultation with a multidisciplinary healthcare team, taking into account the patient’s overall health, stage of cancer, and personal preferences.
- The treatment options for advanced cervical cancer may include surgery, radiation therapy, and chemotherapy.
- Surgical procedures such as radical hysterectomy, extensive lymphadenectomy, or lymph node dissection may be performed.
- Radiation therapy, including postoperative irradiation or combined external beam radiation and brachytherapy may be administered.
- Chemotherapy, using platinum-based doublet regimens or other drugs such as docetaxel, gemcitabine, ifosfamide, 5-fluorouracil, mitomycin, irinotecan, topotecan, pemetrexed, vinorelbine, or bevacizumab, may be utilized.
- The treatment aims to improve overall survival, shrink tumors, alleviate symptoms, and enhance quality of life.
Tumor Size And Depth
In the staging of cervical cancer, two important factors are considered: tumor size and depth of invasion. These factors are crucial in determining the extent of the disease and guiding treatment decisions.
- Tumor size refers to the physical dimensions of the cancerous growth.
- Depth of invasion refers to how far the cancer has grown into the surrounding tissues.
Accurate assessment of tumor size and depth of invasion is achieved through microscopic examination. Additionally, visible tumors can be measured and evaluated during physical examinations or imaging tests. The information obtained from these assessments is vital in helping healthcare professionals determine the most appropriate treatment options for patients diagnosed with cervical cancer.
- Microscopic examination for accurate assessment
- Measurement of visible tumors during physical examinations or imaging tests
“In the staging of cervical cancer, tumor size and depth of invasion play a crucial role in determining the extent of the disease and guiding treatment decisions.”
Local Ablative Measures
Local ablative measures are therapeutic interventions used to destroy or remove pre-cancerous or cancerous cells in the cervix. These measures aim to prevent the progression of pre-cancerous lesions to invasive cervical cancer.
Cryosurgery, involving freezing the abnormal cells, is one of the local ablative measures used to treat carcinoma in situ.
Another method is laser ablation, which uses a high-intensity laser beam to remove the abnormal cells.
Loop excision, also known as large loop excision of the transformation zone (LLETZ), is another technique that involves using an electrical loop to remove the affected tissue.
Local ablative measures are generally effective in removing pre-cancerous or cancerous cells, with minimal risk of complications. However, regular follow-up visits and cervical cancer screenings are essential to monitor the progression of the disease and detect any recurrent or persistent cancer.
- Cryosurgery: involves freezing abnormal cells
- Laser ablation: uses high-intensity laser beam
- Loop excision or LLETZ: uses electrical loop to remove tissue
Regular follow-up visits and cervical cancer screenings are essential.
Treatment Options
The treatment options for cervical cancer depend on various factors, including the stage of the disease, tumor size, lymph node involvement, and the presence of metastasis. A multidisciplinary approach involving healthcare professionals from different specializations, such as gynecologic oncologists, radiation oncologists, and medical oncologists, is often utilized to provide the most comprehensive and effective treatment.
Treatment options for cervical cancer include:
- Surgery: Surgical removal of the tumor and affected tissues may involve procedures such as conization, total or radical hysterectomy, or lymph node dissection.
- Radiation therapy: This can include external beam radiation therapy or brachytherapy. It utilizes high-energy X-rays or radioactive sources to kill cancer cells or shrink tumors.
- Chemotherapy: This refers to the use of drugs that can kill cancer cells or inhibit their growth. It is often used in combination with other treatment modalities.
The selection of treatment options depends on individual patient factors, including overall health, preferences, and the stage and characteristics of the cancer. Treatment plans are tailored to each patient to achieve the best possible outcomes in terms of overall survival, tumor shrinkage, and preservation of quality of life. It is important for patients to have open and thorough discussions with their healthcare team to understand the available treatment options and make informed decisions.
💡
You may need to know these questions about cervical carcinoma in situ
What stage is cervical carcinoma in situ?
Cervical carcinoma in situ is classified as Stage 0 of cervical cancer. At this stage, the cancerous cells are confined to the surface layer of cells lining the cervix. Although it is not considered invasive cancer, carcinoma in situ is a serious condition as it signifies the presence of precancerous cells. If left untreated, these cells have the potential to progress into full-fledged cervical cancer. Therefore, early diagnosis and proper medical intervention are crucial in preventing the advancement of carcinoma in situ to a more severe stage.
What is the treatment for carcinoma in situ of cervix?
The treatment for carcinoma in situ of the cervix, also known as stage 0 cancer, involves local ablative or excisional measures. These procedures include cryosurgery, laser ablation, and loop excision, which effectively remove the pre-cancerous cells. Surgical removal is commonly preferred as it enables additional pathological evaluation to ensure no microinvasive disease is present. Following treatment, lifelong surveillance is necessary to monitor for any recurrence or development of invasive cancer.
Is carcinoma in situ of the cervix curable?
Carcinoma in situ of the cervix, also known as stage 0 cervical cancer, is highly curable. When diagnosed with cervical dysplasia or when precancerous cells are found, surgery is typically the sole treatment required to remove the abnormal areas on the cervix. By surgically removing these precancerous cells, the risk of progression to invasive cervical cancer is greatly diminished. Thus, early detection and timely surgical intervention offer an excellent prognosis for individuals diagnosed with carcinoma in situ of the cervix, ensuring a high likelihood of curability.
What is the prognosis for cervical adenocarcinoma in situ?
The prognosis for cervical adenocarcinoma in situ can vary depending on various factors. Longitudinal studies indicate that a significant percentage of patients with untreated in situ cervical cancer may develop invasive carcinoma within a decade. However, there is also the possibility of a faster progression, with approximately 10% of patients experiencing the transition from in situ to invasive cancer in less than a year. Early detection and timely intervention are crucial in improving the prognosis, as they can potentially prevent or effectively manage the progression of the disease.
Reference source
https://www.uptodate.com/contents/cervical-adenocarcinoma-in-situ
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=34&contentid=17233-1
https://emedicine.medscape.com/article/253513-treatment
https://www.dana-farber.org/cervical-cancer/treatment/