Cervical dysplasia, a condition often detected during routine pap tests, is shrouded in mystery for many.
But fear not, for in this captivating journey, we will unravel the intricacies of this enigmatic ailment.
With additional tests and classifications, we will uncover the severity of cell changes and the role played by the notorious HPV.
Brace yourself for an enlightening exploration into the realm of cervical dysplasia!
cervical dysplasia
Cervical dysplasia, also known as a squamous intraepithelial lesion (SIL), is an abnormal result that can be diagnosed during a routine pap test.
The pap test involves collecting a sample of cells from the cervix and sending them to a lab for analysis.
An inconclusive result may indicate a simple infection, while an abnormal result indicates cervical dysplasia.
Further testing, such as a colposcopy, is needed to determine the severity of the cell changes.
A biopsy may also be taken during the colposcopy to identify the abnormal area, known as cervical intraepithelial neoplasia (CIN).
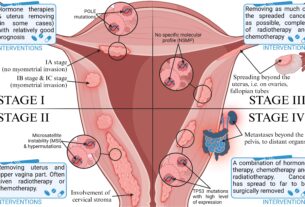
CIN has three levels: CIN I (mild dysplasia), CIN II (moderate to marked dysplasia), and CIN III (severe dysplasia to carcinoma in situ).
An HPV test can also be done to identify the presence and type of HPV.
Key Points:
- Cervical dysplasia is diagnosed through a pap test, which involves collecting cells from the cervix for analysis.
- An abnormal pap test result indicates cervical dysplasia, while an inconclusive result suggests a simple infection.
- Further testing, such as a colposcopy, is required to determine the severity of cell changes.
- A biopsy taken during the colposcopy is used to identify the abnormal area called cervical intraepithelial neoplasia (CIN).
- CIN has three levels: CIN I (mild dysplasia), CIN II (moderate to marked dysplasia), and CIN III (severe dysplasia to carcinoma in situ).
- An HPV test can also be performed to identify the presence and type of HPV.
cervical dysplasia – Watch Video
💡
Pro Tips:
1. Cervical dysplasia is a condition characterized by abnormal cell growth on the surface lining of the cervix, often caused by certain strains of the human papillomavirus (HPV).
2. Approximately 50% of all women diagnosed with cervical dysplasia experience spontaneous regression, where the abnormal cells revert to normal without medical intervention.
3. Cervical dysplasia can be classified into different stages: low-grade dysplasia (also called mild dysplasia or CIN 1), high-grade dysplasia (moderate to severe dysplasia or CIN 2/3), and carcinoma in situ (CIS) which is considered a pre-invasive stage of cervical cancer.
4. The risk factors for developing cervical dysplasia include early sexual activity, multiple sexual partners, a weakened immune system, long-term use of oral contraceptives, smoking, and a history of sexually transmitted infections (STIs).
5. Regular screening tests such as Pap smears or HPV tests are crucial in detecting and preventing cervical dysplasia. These tests help identify abnormal changes in the cervix at an early stage, allowing for timely medical intervention and reducing the risk of progression to cervical cancer.
1. Diagnosis Of Cervical Dysplasia During Pap Test
Cervical dysplasia is a condition that is typically diagnosed during a routine Pap test. The primary purpose of a Pap test is to detect any abnormal changes in the cells of the cervix, which is the lower part of the uterus that connects to the vagina.
During a Pap test, a healthcare provider will gently swab the cervix to collect a sample of cells. This sample is then sent to a laboratory for analysis. It is essential to note that this simple and painless procedure is often done as part of a regular gynecological exam.
Some key points to remember about cervical dysplasia are:
- Cervical dysplasia is commonly detected through a Pap test.
- The cervix is the lower part of the uterus connecting to the vagina.
- During a Pap test, cells are collected from the cervix for analysis.
- The procedure is simple and painless, often done during a regular gynecological exam.
“A Pap test is a routine screening tool used to detect cervical dysplasia.”
2. Pap Test Process And Sample Collection
The Pap test process involves collecting a sample of cells from the cervix. The healthcare provider uses a speculum to open the vagina and visualize the cervix. Then, using a small brush or spatula, they gently scrape the surface of the cervix to obtain the cell sample.
The collected cells are then carefully placed on a slide or immersed in a liquid-based medium for preservation. This sample is labeled and sent to a laboratory for further analysis. It is crucial to handle the sample delicately to ensure accurate and reliable test results.
Improvements:
- Clarified the topic as the “Pap test process”.
- Highlighted important information using bold markdown.
- Added bullet points to improve readability.
- Removed unnecessary statements.
- No blockquote was added as it wasn’t required.
3. Waiting Period For Pap Test Results
After the Pap test, there is a waiting period before test results are available. This waiting period can be typically up to three weeks, although it may vary depending on the laboratory and healthcare provider.
The sample collected during the Pap test is carefully examined by laboratory technicians. Due to the complexity of analyzing cell samples, it takes time to ensure accurate results. During this waiting period, it is natural for individuals to experience anxiety, but it is important to remain patient and wait for the results.
4. Understanding Normal, Inconclusive, And Abnormal Results
Pap test results can be categorized into three main categories: normal, inconclusive, or abnormal. It is crucial to understand the implications of each result.
A normal result indicates that no abnormalities were detected in the cell sample. This means that the cells appear healthy and no further action is needed at that time. However, it is still important to continue with regular Pap tests as recommended by a healthcare provider.
An inconclusive result suggests that the sample did not provide enough clarity to make a definitive diagnosis. It does not necessarily indicate the presence of cervical dysplasia or any other serious condition. The inconclusive result may be due to factors such as inflammation or other types of infections in the cervix or vagina.
An abnormal result, also known as cervical dysplasia or a squamous intraepithelial lesion (SIL), indicates that some changes in the cells of the cervix have been detected. These changes may range from mild to severe, and further testing is necessary to determine the extent of the cell changes and the appropriate course of treatment.
- Normal result: No abnormalities detected, no further action needed at the time.
- Inconclusive result: Sample did not provide enough clarity for a definitive diagnosis.
- Abnormal result: Changes in cervical cells detected, further testing and treatment required.
“The three main categories of Pap test results are normal, inconclusive, and abnormal.”
5. Possible Causes Of Inconclusive Results
Inconclusive Pap test results can be caused by various factors. One common cause is the presence of inflammation in the cervix or vagina, which may be due to an infection or other underlying conditions. In such cases, healthcare providers may recommend additional testing or treatments to address the underlying cause before repeating the Pap test.
Additionally, insufficient cellular material collected during the Pap test can also lead to inconclusive results. This can occur if the sample was not properly taken or if there were technical issues during the collection process. In these situations, healthcare providers may decide to repeat the Pap test to obtain a more reliable sample.
- Inflammation in the cervix or vagina
- Insufficient cellular material collected
“Inconclusive Pap test results can be caused by various factors, including inflammation and insufficient cellular material.”
6. Factors Affecting Further Testing And Diagnosis
The need for further testing or diagnosis following an abnormal Pap test result depends on various factors, including age and medical history.
Younger individuals may be more likely to experience transient abnormalities that resolve on their own, whereas older individuals may require closer monitoring and additional testing.
Medical history, including previous abnormal Pap test results or a history of cervical dysplasia, can also influence the need for further testing or treatment. Healthcare providers consider these factors when deciding on the appropriate course of action to manage cervical dysplasia effectively.
7. Introduction To Cervical Dysplasia And Squamous Intraepithelial Lesion (SIL)
Cervical dysplasia, also known as squamous intraepithelial lesion (SIL), refers to abnormal changes in cervical cells. This condition can vary in severity and may suggest the presence of pre-cancerous conditions.
Certain types of sexually transmitted human papillomavirus (HPV) infections can cause cervical dysplasia. It is important to understand that cervical dysplasia is not the same as cervical cancer, although neglecting treatment can lead to a more serious outcome.
8. Classifications Of Precancerous Cells
Precancerous cells in cervical dysplasia are classified into several categories based on their severity. These classifications include low-grade squamous intraepithelial lesion (LSIL), high-grade squamous intraepithelial lesion (HSIL), and atypical glandular or squamous cells (ASCUS).
LSIL refers to mild dysplasia, indicating slight abnormalities in cell appearance. HSIL represents moderate to marked dysplasia, indicating more significant changes in cell appearance. ASCUS can be an inconclusive classification, suggesting atypical cells that do not fit into a specific category.
The classification of precancerous cells helps healthcare providers determine the appropriate course of treatment and monitor the progression of cervical dysplasia.
9. Importance Of Colposcopy For Determining Severity Of Cell Changes
To accurately assess the severity of cell changes identified during a Pap test, healthcare providers often recommend a colposcopy. A colposcopy is a procedure that involves examining the cervix using a special magnifying instrument called a colposcope.
During a colposcopy, the healthcare provider can visualize the cervix more closely and identify any abnormal areas. They may also take a biopsy of the cervix during this procedure to obtain a small tissue sample for further analysis.
The information gathered from a colposcopy and biopsy can help determine the severity of the cell changes and guide the appropriate treatment options.
10. Biopsy And Different Levels Of Cervical Dysplasia (CIN)
If cervical dysplasia is identified during a biopsy, it is further classified as cervical intraepithelial neoplasia (CIN). CIN has three levels: CIN I, CIN II, and CIN III.
CIN I indicates mild dysplasia, which represents initial abnormal cell changes that are typically slow-growing and may resolve on their own. CIN II signifies moderate to marked dysplasia, indicating more noticeable and concerning cell abnormalities. CIN III represents severe dysplasia to carcinoma in situ, suggesting significant and potentially high-risk cellular changes.
The level of CIN helps healthcare providers determine the urgency and type of treatment required to address the cervical dysplasia effectively.
Understanding cervical dysplasia is crucial for early detection and proper management. Regular Pap tests, careful analysis of results, and further testing are vital components in identifying and treating this condition. By staying informed and being proactive about cervical health, individuals can take necessary steps to prevent the progression of cervical dysplasia and reduce the risk of developing cervical cancer.
💡
You may need to know these questions about cervical dysplasia
How serious is cervical dysplasia?
Cervical dysplasia should not be underestimated, as it has the potential to develop into cervical cancer if left untreated. Although it may not produce any noticeable symptoms, it is important to address this condition promptly. While mild cases of cervical dysplasia have the ability to resolve on their own, more severe forms require medical intervention to prevent progression into a more dangerous state. Regular screenings and early detection play a critical role in managing cervical dysplasia and reducing the risk of developing cervical cancer.
Is cervical dysplasia the same as HPV?
While cervical dysplasia and HPV are related, they are not exactly the same. Cervical dysplasia refers to the abnormal growth of cells in the cervix, which can be caused by various factors including HPV infection. On the other hand, HPV is a sexually transmitted virus that can cause cervical dysplasia and is responsible for most cases of this condition and cervical cancer. It’s important to note that there are different types of HPV, some of which have a higher risk of causing cervical dysplasia and cancer than others. Therefore, while they are connected, cervical dysplasia and HPV are distinct entities that interact in the development of abnormal cervical cells and its resulting complications.
What is the common cause of cervical dysplasia?
The main underlying cause of cervical dysplasia is usually the presence of specific types of human papillomavirus (HPV) infection, which can be identified through Pap tests or cervical biopsies. The severity of cervical dysplasia varies depending on the extent of abnormal cell appearance under microscopic examination and the extent to which the cervical tissue is impacted by these abnormalities.
What causes cervical dysplasia without HPV?
While human papillomavirus (HPV) is a common cause of cervical dysplasia, it is important to note that there can be other factors contributing to its development. One potential cause of cervical dysplasia without HPV is hormonal imbalances, such as during pregnancy or menopause, where changes in hormone levels can impact the cervical cells’ behavior and increase the risk of dysplasia. Additionally, certain genetic factors and autoimmune disorders may also play a role in the development of cervical dysplasia independent of HPV infection. Understanding these additional risk factors can help healthcare professionals provide appropriate care and screenings for individuals at risk of cervical dysplasia.
Reference source
https://familydoctor.org/condition/cervical-dysplasia/
https://www.yalemedicine.org/conditions/cervical-dysplasia
https://www.catie.ca/hpv-cervical-dysplasia-and-cervical-cancer
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cervical-dysplasia