Picture this: you’re sitting in a doctor’s office, anxiously awaiting test results that could change your life.
The doctor enters the room and drops a bombshell – you have cervical dysplasia, a condition known as cervical intraepithelial neoplasia (CIN).
What does this mean?
How did it happen?
And most importantly, what can be done to prevent it from turning into cervical cancer?
Join us as we explore the intriguing world of CIN, its causes, screenings, and the vital steps you can take to protect yourself.
Get ready to delve into the fascinating realm of cervical health – trust us, you won’t want to miss it.
cervical intraepithelial neoplasm
Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia, is a precancerous condition where abnormal cells grow on the surface of the cervix.
It is primarily found in sexually active individuals assigned female at birth who have a cervix, most commonly occurring in women of childbearing age.
CIN is graded on a scale from one to three, with CIN 1 affecting about one-third of the thickness of the epithelium, CIN 2 affecting about one-third to two-thirds, and CIN 3 affecting more than two-thirds.
CIN is primarily caused by chronic infection of the cervix with high-risk types of human papillomavirus (HPV), particularly types 16 or 18.
While most cases of CIN either remain stable or resolve on their own, a small percentage can progress to cervical cancer if left untreated.
Screening for CIN can be done through Pap smears or HPV testing, with treatment involving the removal or destruction of abnormal cells.
HPV vaccination is the primary prevention method, but it does not protect against all cancer-causing HPV types.
Management and treatment are crucial in secondary prevention for cervical cancer cases.
Key Points:
- Cervical intraepithelial neoplasia (CIN) is a precancerous condition where abnormal cells grow on the cervix.
- CIN is primarily found in sexually active individuals assigned female at birth who have a cervix, occurring most commonly in women of childbearing age.
- CIN is graded on a scale from one to three, with CIN 1 affecting about one-third of the epithelium, CIN 2 affecting one-third to two-thirds, and CIN 3 affecting more than two-thirds.
- Chronic infection of the cervix with high-risk types of HPV, particularly types 16 or 18, is the primary cause of CIN.
- While most cases of CIN remain stable or resolve on their own, a small percentage can progress to cervical cancer if left untreated.
- Screening for CIN can be done through Pap smears or HPV testing, with treatment involving the removal or destruction of abnormal cells.
cervical intraepithelial neoplasm – Watch Video
💡
Pro Tips:
1. Cervical intraepithelial neoplasm (CIN) is also known as dysplasia, a condition characterized by abnormal cell growth on the surface of the cervix.
2. CIN is often caused by persistent infection with the human papillomavirus (HPV), a sexually transmitted infection that affects both men and women.
3. In most cases, CIN is detected through routine Pap smear screenings, which can help identify abnormal cell changes before they develop into cancer.
4. There are three levels of CIN, ranging from mild (CIN 1) to moderate (CIN 2) to severe (CIN 3). CIN 3 is considered a significant precancerous condition and requires prompt medical attention.
5. If left untreated, severe CIN (CIN 3) can progress to cervical cancer. However, when detected early, most cases of CIN can be effectively treated, preventing the development of invasive cancer.
Understanding Cervical Dysplasia: Abnormal Cell Growth On The Cervix
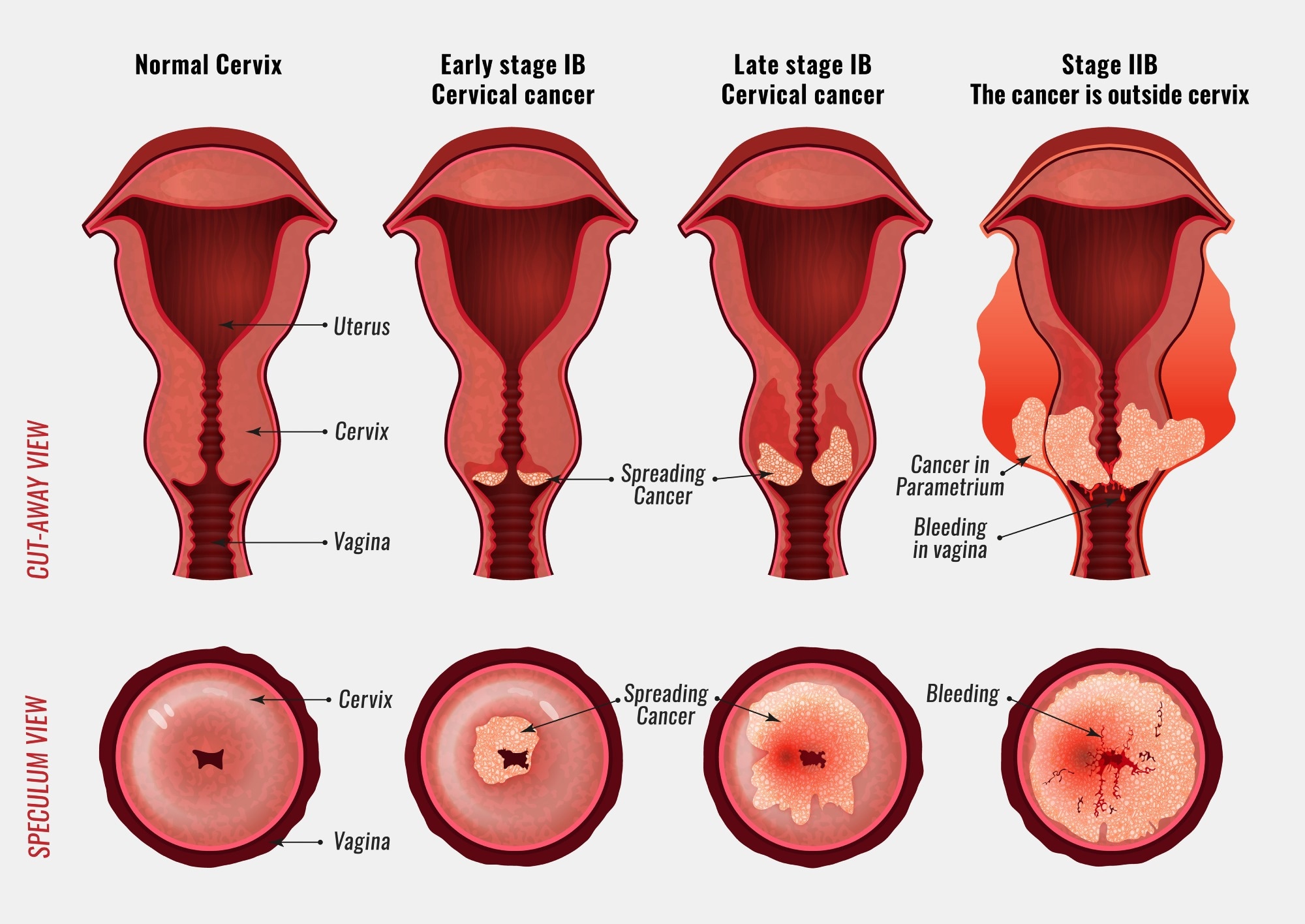
Cervical dysplasia, also known as cervical intraepithelial neoplasia (CIN), is a precancerous condition characterized by the growth of abnormal cells on the surface of the cervix. The cervix is the narrow passage connecting the uterus and the vagina. Cervical dysplasia is commonly seen in sexually active individuals who have a cervix and are assigned female at birth (AFAB). It primarily affects women of childbearing age, typically between 25 and 35 years old.
Cervical dysplasia is classified on a scale from one to three, with CIN 1 only affecting about one-third of the thickness of the epithelium. In contrast, CIN 2 affects about one-third to two-thirds of the epithelium, and CIN 3 affects more than two-thirds. This classification helps healthcare professionals determine the severity of the condition and plan appropriate treatment methods. However, it is important to note that most cases of cervical dysplasia do not progress to cancer.
Cervical Dysplasia And Cin: Two Terms For The Same Precancerous Condition
Cervical dysplasia and cervical intraepithelial neoplasia (CIN) are terms used interchangeably to describe a precancerous condition. CIN refers to the abnormal growth of cells on the cervix’s surface that may develop into cervical cancer if left untreated. The severity of this condition is graded on a scale from one to three, with CIN 3 being the most severe.
The presence of human papillomavirus (HPV) infection is necessary for the development of CIN. HPV is a common sexually transmitted infection, and while many individuals with HPV do not develop cervical dysplasia or cervical cancer, the infection often resolves without intervention. However, individuals with persistent HPV infections lasting more than one or two years have a higher risk of developing a higher grade of CIN.
Most Cases Of Cervical Dysplasia Do Not Progress To Cancer
While cervical dysplasia is a precancerous condition, it is important to note that most cases do not progress to cancer. In fact, the majority of individuals with cervical dysplasia, especially those with lower-grade classifications such as CIN 1, have a high likelihood of spontaneous regression or elimination of the abnormal cells. The immune system plays a crucial role in combating cervical dysplasia, and many cases resolve without the need for intervention.
However, it is crucial to monitor cervical dysplasia closely, as a small percentage of cases may progress to cervical cancer if left untreated. Regular screening and follow-up appointments with healthcare professionals are essential for early detection and timely intervention if necessary.
- Regular screening and follow-up appointments with healthcare professionals
- Proactive approach to healthcare
- Early detection and timely intervention
Grading Cervical Dysplasia: Cin 1, Cin 2, And Cin 3 Explained
Cervical dysplasia is classified into three grades: CIN 1, CIN 2, and CIN 3, to determine the severity of the condition. CIN 1 refers to mild dysplasia, where abnormal cells affect about one-third of the thickness of the epithelium. CIN 2 indicates moderate dysplasia, with abnormal cells affecting about one-third to two-thirds of the epithelium. CIN 3, also known as severe dysplasia or carcinoma in situ (CIS), shows abnormal cell growth in more than two-thirds of the epithelium.
The classification of cervical dysplasia helps healthcare professionals determine appropriate treatment plans and interventions. Lower-grade dysplasia, such as CIN 1, is often closely monitored as it may resolve on its own without intervention. On the other hand, higher-grade dysplasia, such as CIN 2 and CIN 3, may require more aggressive treatment methods to remove or destroy the abnormal cells.
Cervical Dysplasia And Its Impact On AFAB Individuals
Cervical dysplasia primarily affects individuals assigned female at birth (AFAB) who have a cervix and are sexually active. The cervix is a vital reproductive organ located at the lower end of the uterus, entering the upper part of the vagina. AFAB individuals are at a higher risk of developing cervical dysplasia due to the presence of a cervix and their susceptibility to human papillomavirus (HPV) infections.
It is important for AFAB individuals to prioritize regular screenings and follow-up appointments to monitor their cervical health. Early detection and intervention can significantly reduce the risk of cervical dysplasia progressing to cervical cancer. Healthcare providers play a crucial role in educating AFAB individuals about the importance of HPV vaccinations, safe sex practices, and regular check-ups to prevent and manage cervical dysplasia effectively.
- AFAB individuals with a cervix and sexually active are primarily affected by cervical dysplasia.
- Cervix is a vital reproductive organ located at the lower end of the uterus, entering the upper part of the vagina.
- AFAB individuals are at a higher risk due to the presence of a cervix and susceptibility to HPV infections.
“Early detection and intervention can significantly reduce the risk of cervical dysplasia progressing to cervical cancer.”
Cervical Dysplasia: Common Among Women Of Childbearing Age
Cervical dysplasia is most commonly seen among women of childbearing age, typically between the ages of 25 and 35. During this period, women are more likely to be sexually active, and their hormones may fluctuate due to menstrual cycles and potential pregnancies. These factors can influence the development and progression of cervical dysplasia.
It is crucial for women in this age group to prioritize regular cervical screenings, such as Pap smears or HPV tests. These screening methods can detect any abnormal cell growth on the surface of the cervix at an early stage, allowing for prompt intervention and treatment, if necessary. By staying proactive about cervical health, women can reduce the risk of cervical dysplasia progressing to cancer and ensure their overall well-being.
- Women between the ages of 25 and 35 are most susceptible to cervical dysplasia
- Sexual activity and hormonal changes during this period can affect the development of cervical dysplasia
- Regular cervical screenings, such as Pap smears or HPV tests, are crucial for early detection
- Early intervention and treatment can prevent cervical dysplasia from progressing to cancer.
The Prevalence Of Cervical Dysplasia In The United States
Cervical dysplasia is a prevalent condition in the United States, affecting a significant number of cisgender women each year. It is estimated that between 250,000 and 1 million American women are diagnosed with cervical dysplasia annually. These numbers highlight the importance of raising awareness about cervical health and promoting regular screenings and vaccinations to prevent the development and progression of cervical dysplasia.
Healthcare providers play a crucial role in educating women about the risk factors, symptoms, and available preventive measures regarding cervical dysplasia. By disseminating accurate information and providing accessible healthcare services, the incidence of cervical dysplasia and its potential complications, such as cervical cancer, can be significantly reduced.
The Role Of HPV Infection In The Development Of Cervical Dysplasia
Human papillomavirus (HPV) infection is a necessary factor in the development of cervical dysplasia. HPV is a common sexually transmitted infection, and there are over 100 different types of HPV. Approximately 40 types affect the anogenital area, including the cervix. Infection with high-risk types of HPV, such as HPV 16 or 18, is closely associated with the development of cervical dysplasia and cervical cancer.
It is important to note that most women with HPV infection do not develop high-grade intraepithelial lesions or cancer. The majority of HPV infections resolve spontaneously, especially in individuals with a healthy immune system. However, persistent HPV infection, lasting for more than one or two years, increases the risk of developing higher grades of cervical dysplasia.
Regular HPV testing and vaccinations play a vital role in the prevention and management of cervical dysplasia. HPV testing can identify high-risk types of HPV responsible for cervical dysplasia, enabling healthcare providers to monitor and intervene effectively. HPV vaccinations, such as the Gardasil or Cervarix vaccines, are the primary prevention method for cervical dysplasia and cervical cancer. However, it is important to note that these vaccines do not protect against all types of HPV known to cause cancer.
Most CIN Cases Resolve On Their Own, But Some Progress To Cancer
Cervical intraepithelial neoplasia (CIN) refers to abnormal cell growth on the cervix. Most CIN cases either stabilize or resolve on their own without intervention. Within one year, about 70% of CIN 1 cases and 90% of CIN 2 cases regress. However, a small percentage of cases may progress to more severe stages, such as cervical carcinoma in situ (CIS) or invasive cancer. The progression rates vary based on the grade of dysplasia, with approximately 11% of CIN 1 and 22% of CIN 2 cases progressing to CIS. For CIN 3 cases, the estimated likelihood of progression to invasive cancer is at least 12%. Therefore, close monitoring and management of CIN cases, even if they are low-grade, is crucial. Regular screenings and follow-up appointments are essential for early detection of progression and to initiate appropriate treatment measures if necessary.
Symptoms, Risk Factors, And Diagnosis Of Cervical Dysplasia
Cervical dysplasia typically does not present specific symptoms on its own. However, if the condition progresses to cervical cancer, individuals may experience symptoms such as abnormal bleeding, abnormal discharge, changes in bladder or bowel function, pelvic pain, or an abnormal appearance or palpation of the cervix.
Several risk factors increase the likelihood of developing cervical dysplasia, including:
- Infection with high-risk types of HPV
- Immunodeficiency
- Poor diet
- Engaging in sexual activity with multiple partners
- Lack of condom use
- Cigarette smoking
These factors emphasize the importance of safe sex practices, healthy lifestyle choices, and regular check-ups for early detection and intervention.
The diagnosis of cervical dysplasia or cervical carcinoma requires a biopsy for analysis. This can be performed during a colposcopy with directed biopsy, which involves examining the cervix under magnification and taking a tissue sample for laboratory analysis. The Bethesda System for Reporting Cervical/Vaginal Cytologic Diagnoses provides a uniform way to describe abnormal epithelial cells and aids in the accurate diagnosis and management of cervical dysplasia.
Screening for cervical dysplasia can be done through a Pap smear or testing for HPV. Pap smear results may vary in accuracy, highlighting the need for regular screenings and follow-up evaluations. Abnormal Pap smear results may lead to further diagnostic procedures, such as colposcopy. HPV testing can identify high-risk HPV types responsible for cervical dysplasia and guide healthcare providers in determining the appropriate course of action.
In conclusion, understanding and raising awareness about cervical dysplasia are essential in ensuring timely diagnosis, appropriate treatment, and effective prevention strategies. Close monitoring, regular screenings, and follow-up appointments are critical for individuals with cervical dysplasia. By staying proactive and informed, individuals can take control of their cervical health and reduce the risk of complications, such as cervical cancer.
- Regular check-ups for early detection and intervention
- Safe sex practices and healthy lifestyle choices
- The Bethesda System for accurate diagnosis and management
- Regular screenings and follow-up evaluations for Pap smear
- HPV testing to guide healthcare providers
💡
You may need to know these questions about cervical intraepithelial neoplasm
What is a cervical intraepithelial neoplasia?
Cervical intraepithelial neoplasia (CIN) refers to a precancerous state of the uterine cervix where there are abnormal changes in the cells of the cervical tissue. The cervix, which is the lower part of the uterus, has two different types of epithelium – squamous epithelium covering the ectocervix and glandular epithelium covering the endocervix and cervical canal. CIN typically involves abnormal growth and proliferation of cells in the squamous epithelium, indicating a potential progression towards cervical cancer if left untreated. It is important to detect and monitor CIN early through regular screenings such as Pap tests to prevent the development of cervical cancer.
Is cervical intraepithelial neoplasia a form of cancer?
Cervical intraepithelial neoplasia (CIN) is not a form of cancer itself. Rather, it refers to the abnormal changes in the cervical cells that can potentially progress into cervical cancer if left untreated. While CIN does not indicate the presence of cancer, it serves as an important indicator for early intervention to prevent the development of cervical cancer in the future.
How serious is cervical intraepithelial neoplasia?
Cervical intraepithelial neoplasia (CIN) is a condition where abnormal cells are found on the surface of the cervix. While CIN 1 and CIN 2 are generally considered less severe and have a lower risk of progressing to cancer, CIN 3 is a direct precursor to cervical cancer. Treatment is always recommended for CIN 3 cases due to its potential seriousness. The risk of progression to cancer depends not only on age and CIN grade but also on other factors such as the patient’s HPV and cytology results preceding the CIN diagnosis. These additional factors should be considered when assessing the severity and potential implications of cervical intraepithelial neoplasia.
What causes intraepithelial neoplasia of the cervix?
Intraepithelial neoplasia of the cervix, also known as CIN, is primarily caused by a long-term infection of the cervix with HPV. This chronic infection is particularly associated with high-risk HPV types 16 or 18. These high-risk types of HPV have been established as the main culprits behind the development of CIN. The presence of HPV in the cervix can lead to cellular changes and abnormal growth of the cervical cells, potentially progressing to cervical cancer if left untreated. It is crucial to detect and manage HPV infections to prevent the development of CIN.
Reference source
https://www.uptodate.com/contents/cervical-intraepithelial-neoplasia-terminology-incidence-pathogenesis-and-prevention
https://www.macmillan.org.uk/cancer-information-and-support/worried-about-cancer/pre-cancerous-and-genetic-conditions/cin
https://www.uptodate.com/contents/cervical-intraepithelial-neoplasia-management
https://en.wikipedia.org/wiki/Cervical_intraepithelial_neoplasia