In a world where secrets can lurk beneath the surface, a silent threat silently wreaks havoc.
Enter cervied intraepithelial carcinoma – a formidable enemy that few know about.
This invisible villain, caused predominantly by the Human Papillomavirus (HPV), hides in the shadows and spreads through intimate encounters.
But beware, for even the strongest armor may prove powerless against its cunning ways.
In this article, we explore the intricate dance between HPV and CIN, revealing the truths that lie beyond the veil of protection.
cervied intraepithelial carcinoma
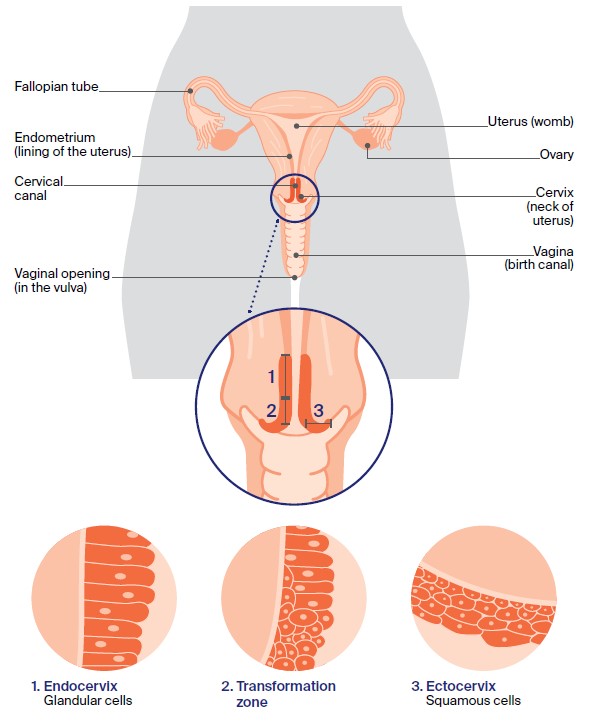
Cervical intraepithelial carcinoma (CIN) is primarily caused by the human papillomavirus (HPV) infection.
HPV is a common virus that can affect the cervix, and there are over 100 types of HPV, with some being high-risk and capable of causing abnormal cell changes in the cervix.
While the body’s immune system can usually clear the infection naturally, in some cases, the virus may persist for a longer period, leading to the development of CIN.
It is important to note that HPV can be contracted through various sexual activities and the use of barrier contraception, while helpful, does not provide complete protection against the virus.
Key Points:
- Cervical intraepithelial carcinoma is mainly caused by HPV infection.
- There are over 100 types of HPV, some of which are high-risk and can cause abnormal cell changes in the cervix.
- The body’s immune system can usually clear the HPV infection naturally, but in some cases, the virus may persist and lead to CIN.
- HPV can be contracted through various sexual activities.
- The use of barrier contraception does not provide complete protection against HPV.
- HPV infection is a common virus that can affect the cervix.
cervied intraepithelial carcinoma – Watch Video
💡
Pro Tips:
1. Cervied intraepithelial carcinoma, also known as CIN, is a pre-cancerous condition that affects the cervix in women.
2. CIN is primarily caused by an infection with the Human Papillomavirus (HPV), which is a sexually transmitted virus.
3. Around 70% of cases of CIN regress naturally over time without any medical intervention or treatment.
4. Research suggests that long-term use of oral contraceptives (birth control pills) may slightly increase the risk of developing CIN.
5. Regular screenings, such as the Pap smear or HPV test, can help detect CIN early and prevent its progression to cervical cancer.
The Main Cause Of Cervical Intraepithelial Carcinoma (CIN)
Cervical Intraepithelial Carcinoma (CIN) is primarily caused by the human papillomavirus (HPV). HPV triggers abnormal cell changes in the cervix, leading to the development of CIN. Over 100 different types of HPV exist, but it is the high-risk types that have the most significant impact on the cervix. It is worth noting that the body’s immune system can often naturally clear the HPV infection without showing any symptoms. However, if the immune system fails to eradicate the infection, the virus can persist in the body for longer periods, increasing the likelihood of developing CIN.
- The human papillomavirus (HPV) is responsible for causing Cervical Intraepithelial Carcinoma (CIN).
- CIN is a result of abnormal cell changes in the cervix triggered by HPV.
- High-risk types of HPV have a more significant impact on the cervix.
- The body’s immune system can often clear HPV naturally without symptoms.
- Persistent HPV infections increase the risk of developing CIN over time.
Human Papilloma Virus (HPV) And Cervical Intraepithelial Carcinoma (CIN)
HPV is a widely recognized and acknowledged risk factor for the development of CIN. This virus can easily be transmitted through various forms of sexual contact, making it highly prevalent among sexually active individuals.
It is important to note that HPV can affect both males and females, and sexual orientation or relationship status is not a determining factor in its spread. Even individuals who have not been sexually active for years are still vulnerable to HPV infection.
Due to its ability to live on the skin around the entire genital area, the virus can easily be transmitted through skin-to-skin genital contact or even the sharing of sex toys.
While using barrier contraception like condoms may reduce the risk of HPV transmission, it does not provide complete protection against the virus.
- HPV is a recognized risk factor for the development of CIN
- HPV is transmitted through various forms of sexual contact
- It can affect both males and females, regardless of sexual orientation or relationship status
- Even individuals who have not been sexually active for years can still be vulnerable to HPV infection
- HPV can be transmitted through skin-to-skin genital contact and sharing of sex toys
- Condoms may reduce the risk of HPV transmission, but do not provide complete protection against the virus.
“HPV is a widely recognized and acknowledged risk factor for the development of CIN.”
The Different Types Of HPV That Affect The Cervix
HPV encompasses various types, but only certain strains have the potential to cause abnormal cell changes in the cervix. These types are classified as high-risk HPV. The most prevalent of these high-risk types are HPV-16 and HPV-18, which are responsible for the majority of cervical cancer cases worldwide. Other high-risk types include HPV-31, HPV-33, HPV-45, and HPV-58. It is important to identify the specific HPV type in cases of CIN accurately. This information aids healthcare professionals in managing the condition effectively and taking the necessary steps to monitor and treat any precancerous or cancerous changes in the cervix.
How The Immune System Responds To HPV Infection
The human immune system is essential for defending the body against infections, such as HPV. Upon HPV infection, the immune system recognizes the virus as foreign and initiates a defense mechanism to eliminate it. In most cases, this immune response effectively clears the HPV infection, resolving the issue without any long-term consequences. It is important to note that this clearance may occur without noticeable symptoms. However, in some cases, the immune response may be inadequate, leading to the persistence of the virus within the body. This increases the risk of developing CIN (cervical intraepithelial neoplasia) and its associated complications.
Key points:
- The immune system plays a crucial role in protecting against HPV.
- HPV infection triggers the immune system’s defense mechanism.
- Adequate immune response leads to clearance of HPV infection.
- Insufficient immune response increases the risk of developing CIN and complications.
Remember, the immune system is the body’s first line of defense against viruses like HPV.
When The Immune System Cannot Clear The HPV Infection
There are instances where the immune system fails to clear the HPV infection efficiently. In such cases, the virus can persist within the body, leading to long-term effects on the cervix. Smaller amounts of high-risk HPV can continue to stimulate the growth of abnormal cells within the cervix, eventually leading to CIN. Factors that may affect the immune system’s ability to clear the HPV infection include:
- weakened immune response due to age
- tobacco use
- stress
- other infections
- certain immune system disorders or medications.
Regular check-ups, including cervical screenings, are crucial for detecting any abnormalities early on and managing the condition promptly.
Long-Term Effects Of HPV On The Cervix
Prolonged infection with high-risk HPV can have serious consequences for the cervix. Over time, the virus can cause damage to the cells and the DNA within the cervical tissue, leading to the development of precancerous lesions. If left untreated, these lesions can progress to cervical cancer. It is important to note that not all cases of CIN progress to cancer. With regular monitoring and early intervention, CIN can typically be managed effectively to prevent further progression. Cervical cancer, however, can be life-threatening. Therefore, it is crucial for individuals to stay updated with recommended screening guidelines and receive timely treatment if any abnormalities are detected.
The Widespread Prevalence Of HPV
HPV is one of the most common sexually transmitted infections worldwide. It is estimated that the majority of sexually active individuals will contract HPV at some point in their lives, regardless of their sexual orientation or relationship status.
The high prevalence of HPV highlights the importance of proactive measures such as regular cervical screenings and HPV vaccinations.
- HPV is a sexually transmitted infection
- Majority of sexually active individuals will contract HPV
- Proactive measures include regular cervical screenings and HPV vaccinations
Vaccinations against HPV are now available and recommended for both males and females. These vaccines can provide protection against the most common high-risk types of HPV responsible for the development of cervical cancer, thus reducing the overall burden of CIN (cervical intraepithelial neoplasia) and cervical cancer in the population.
- HPV vaccines recommended for both males and females
- Protects against high-risk types of HPV
- Reduces the burden of CIN and cervical cancer
“The high prevalence of HPV highlights the importance of proactive measures such as regular cervical screenings and HPV vaccinations.”
HPV Transmission And Sexual Activity
Sexual activity is the primary route of HPV transmission. The virus can be transmitted through various forms of sexual contact, including vaginal, anal, and oral sex. It is important to note that even individuals who have not engaged in sexual activity for an extended period can still acquire HPV if they come into contact with the virus. Therefore, it is crucial for individuals to take necessary precautions and practice safe sexual behaviors. This includes using barrier contraception such as condoms or dental dams consistently and correctly, as well as getting vaccinated against HPV.
HPV Transmission Through Skin-To-Skin Contact
In addition to sexual activity, HPV can also be transmitted through skin-to-skin contact in the genital area. This means that even without penetration or the exchange of bodily fluids, HPV can still be passed on through intimate contact. Skin-to-skin genital contact includes activities such as genital rubbing or close contact without the use of barrier contraception. Moreover, sharing sex toys without proper cleaning and disinfection can also lead to HPV transmission. It is essential for individuals to be aware of these modes of transmission and take appropriate precautions to reduce their risk of acquiring or transmitting HPV.
- HPV can be transmitted through skin-to-skin contact in the genital area, even without penetration or exchange of bodily fluids.
- Activities such as genital rubbing or close contact without barrier contraception can lead to HPV transmission.
- Sharing sex toys without proper cleaning and disinfection can also increase the risk of HPV transmission.
- Individuals should be aware of these modes of transmission and take precautions to reduce the risk of acquiring or transmitting HPV.
Limitations Of Condom Use In Preventing HPV Infection
While using condoms or other types of barrier contraception is an important preventive measure against HPV transmission, it is crucial to understand that condoms do not provide complete protection. HPV can be present on areas of the skin not covered by the condom, such as the scrotum, vulva, or anal region. As a result, transmission can still occur through skin-to-skin contact. Additionally, HPV can infect areas that are not covered by condoms, such as the mouth and throat, making oral sex another potential route of transmission. Therefore, while condom use is highly recommended, it is important to combine it with other preventive measures such as regular screenings and HPV vaccinations to effectively reduce the risk of HPV infection.
- Using condoms or barrier contraception is important but provides incomplete protection.
- HPV can be present on uncovered skin areas, like the scrotum, vulva, or anal region.
- Skin-to-skin contact can still lead to transmission.
- Condoms do not fully protect against infection in the mouth and throat.
- Combining condom use with regular screenings and HPV vaccinations helps reduce the risk of HPV infection.
💡
You may need to know these questions about cervied intraepithelial carcinoma
What is the difference between cervical intraepithelial neoplasia and cervical cancer?
Cervical intraepithelial neoplasia (CIN) refers to abnormal changes in the cells of the cervix that are potentially pre-cancerous. It is commonly caused by high-risk HPV infections. It is important to note that the majority of CIN lesions regress on their own, without developing into invasive cervical cancer. Cervical cancer, on the other hand, occurs when CIN lesions persist or progress to the stage of invasive carcinoma. This means that the abnormal cells have invaded the underlying tissues of the cervix and potentially spread to other parts of the body. While CIN is a precursor to cervical cancer, it is not necessarily indicative of cancer development in all cases.
How serious is cervical intraepithelial neoplasia?
Cervical intraepithelial neoplasia (CIN) is a condition that requires serious attention, particularly in cases of CIN 3. CIN 3 is a direct precursor to cervical cancer, which highlights the importance of timely treatment. While age and CIN grade play a role in predicting the risk of cancer progression, it is crucial to consider additional factors such as the patient’s HPV and cytology results leading up to the diagnosis of CIN. These factors provide valuable insights into the individual’s specific risk and further emphasize the significance of addressing CIN promptly.
When does CIN become cancer?
The transformation of cervical intraepithelial neoplasia (CIN) into cancer typically occurs when CIN is left untreated and is accompanied by persistent human papillomavirus (HPV) infection. If left unchecked, approximately 5% of CIN 2 and 12% of CIN 3 cases have the potential to advance to invasive cancer. However, the progression from CIN to cancer usually takes between 10 to 20 years, allowing a substantial window for early detection and intervention. By identifying and treating CIN in its early stages, the risk of it evolving into cancer can be significantly reduced.
What percentage of CIN 3 turns into cancer?
Based on the available background information, it is estimated that approximately 12 to 40 percent of CIN 3 cases may progress to invasive cancer if left untreated. However, it is important to note that CIN 3 also has a spontaneous regression rate of 32 to 47 percent. Therefore, the exact percentage of CIN 3 cases that ultimately turn into cancer cannot be definitively determined without considering factors such as individual patient characteristics, treatment options, and response to treatment.
Reference source
https://www.macmillan.org.uk/cancer-information-and-support/worried-about-cancer/pre-cancerous-and-genetic-conditions/cin
https://my.clevelandclinic.org/health/diseases/15678-cervical-intraepithelial-neoplasia-cin
https://pubmed.ncbi.nlm.nih.gov/10626803/
https://www.uptodate.com/contents/cervical-intraepithelial-neoplasia-management