The cervix, an often overlooked and mysterious part of the female reproductive system, holds secrets that can have a profound impact on a woman’s health.
From the risk of sexually transmitted infections to the potential for cervical cancer, understanding and caring for this small yet mighty organ is crucial.
In this article, we will delve into the depths of cervicitis, exploring its causes, prevention, and the vital importance of screenings.
Prepare to be enlightened and empowered as we unravel the enigma of the cervix.
cervix
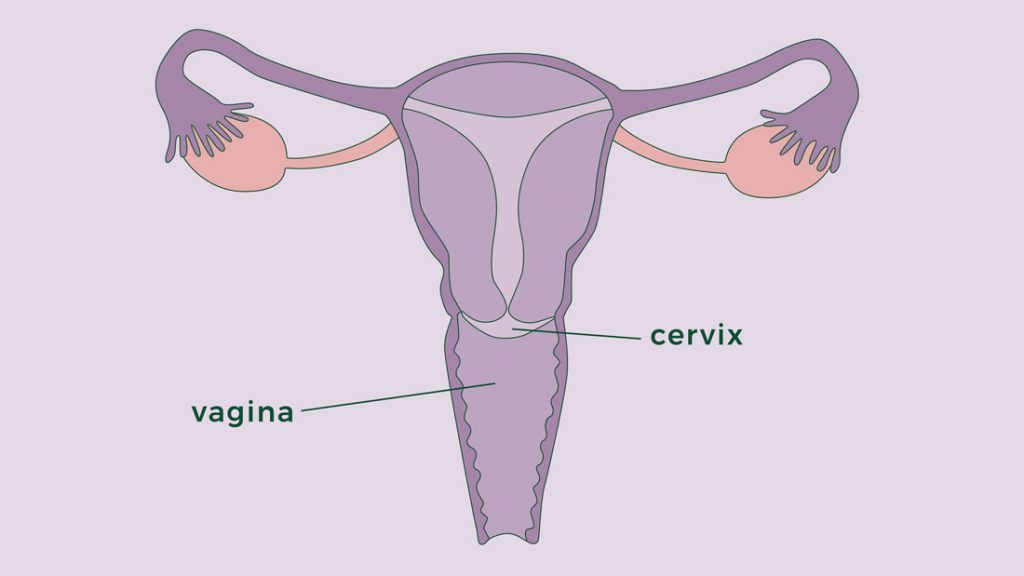
The cervix is the lower, narrow end of the uterus that opens into the vagina.
It is located inside the pelvic cavity, approximately 3 to 6 inches inside the vaginal canal.
The cervix consists of the internal OS, endocervical canal, ectocervix, and external OS.
It is wider in the middle and narrows at both ends.
Symptoms of cervicitis, which is inflammation of the cervix, include bleeding between menstrual periods, pain during intercourse or pelvic exams, and abnormal vaginal discharge.
Cervicitis can be caused by sexually transmitted infections (STIs) such as chlamydia and gonorrhea, as well as noninfectious factors like allergic reactions to contraceptives or feminine hygiene products.
High-risk sexual behavior, early age of sexual intercourse, and a history of STIs are risk factors for cervicitis.
If left untreated, complications can include pelvic inflammatory disease, fertility problems, and an increased risk of acquiring HIV.
To prevent cervicitis, consistent and correct use of condoms and being in a committed, monogamous relationship are recommended.
The cervix is about an inch long and varies in size, and its texture and location change during the menstrual cycle.
It is made of fibromuscular tissue and contains different types of cells.
The transitional zone (TZ) is the focus of cervical cancer screenings.
Key Points:
- The cervix is the lower end of the uterus that opens into the vagina.
- It is located inside the pelvic cavity, approximately 3 to 6 inches inside the vaginal canal.
- The cervix includes the internal and external OS, endocervical canal, and ectocervix.
- Cervicitis, inflammation of the cervix, can cause symptoms like bleeding, pain during intercourse, and abnormal discharge.
- Cervicitis can be caused by STIs and noninfectious factors like allergic reactions.
- Complications of untreated cervicitis can include pelvic inflammatory disease, fertility problems, and increased HIV risk.
cervix – Watch Video
💡
Pro Tips:
1. The cervix, also known as the neck of the uterus, contains specialized cells called columnar epithelial cells that produce mucus. This mucus changes in consistency throughout a woman’s menstrual cycle, becoming thinner and more slippery when ovulation occurs, facilitating sperm transport and fertility.
2. The term “cervix” is derived from Latin, meaning “neck.” It was first used to describe the narrow, cylindrical shape and position of this reproductive organ within the female body.
3. The cervix undergoes structural changes during pregnancy to form what is known as the cervical mucus plug. This plug seals off the opening of the cervix, providing protection against infections and helping to maintain the pregnancy by preventing the amniotic sac from rupturing prematurely.
4. While the majority of cervix-related issues are benign, the cervix can be affected by various conditions, including cervical polyps. These are small growths that arise from the cervical canal and often go unnoticed unless they cause symptoms like abnormal bleeding.
5. Research suggests that the cervix not only serves as a barrier to protect against infections, but it also plays a role in shaping the immune response during pregnancy. It contains immune cells that help to maintain a delicate balance between defending against pathogens while tolerating the presence of the developing fetus.
Introduction To Cervicitis
Cervicitis is a medical condition characterized by inflammation of the cervix – the lower, narrow end of the uterus that opens into the vagina. The cervix plays a crucial role in the female reproductive system as it serves as a pathway for sperm to travel into the uterus and it also helps protect the uterus from infections.
When the cervix becomes inflamed, it can lead to various symptoms and complications. Cervicitis is a common condition that affects many women, and it can be caused by a variety of factors, including sexually transmitted infections (STIs) and noninfectious causes.
Symptoms Of Cervicitis
Cervicitis is a condition that can cause various symptoms, although some women may not have any symptoms at all. Common symptoms of cervicitis include:
- Bleeding between menstrual periods: This can be a cause of concern for women, especially when accompanied by pain or discomfort.
- Pain during sexual intercourse or pelvic examinations: This can have a significant impact on a woman’s sexual and reproductive health.
- Abnormal vaginal discharge: The discharge may have a foul odor or an unusual color, which can indicate an infection or inflammation of the cervix.
It’s important for women experiencing these symptoms to seek medical attention for proper diagnosis and treatment.
Causes Of Cervicitis
Cervicitis is a condition that can be caused by several factors, with sexually transmitted infections (STIs) like chlamydia and gonorrhea being common culprits. These infections are primarily transmitted through unprotected sexual activity and, if left untreated, can result in inflammation of the cervix. But it’s not just STIs that can cause cervicitis. It can also occur due to noninfectious causes, including allergic reactions to contraceptives or latex in condoms, as well as reactions to feminine hygiene products. These allergic reactions can cause irritation and inflammation in the cervix. It is worth mentioning that some cases of cervicitis may not have an identifiable cause.
Risk Factors For Cervicitis
Several risk factors increase the likelihood of developing cervicitis. High-risk sexual behavior, including having multiple sexual partners and engaging in unprotected sex, can expose individuals to STIs and increase the risk of cervicitis. Early age of sexual intercourse is also a risk factor, as the cervix may be more vulnerable to infections and inflammations at a younger age. History of previous STIs puts individuals at a higher risk of developing cervicitis, as the inflammation may persist or reoccur. It is important for individuals to be aware of these risk factors and take necessary precautions to reduce their risk of cervicitis.
- High-risk sexual behavior, such as having multiple sexual partners and engaging in unprotected sex
- Early age of sexual intercourse
- History of previous STIs
“It is important for individuals to be aware of these risk factors and take necessary precautions to reduce their risk of cervicitis.”
Complications Of Cervicitis
If left untreated, cervicitis can lead to various complications. One of the most significant complications is pelvic inflammatory disease (PID), which is an infection that can spread to the uterus, fallopian tubes, and ovaries. PID can cause severe pain, fertility problems, and increase the risk of ectopic pregnancies.
Moreover, untreated cervicitis can also increase the risk of getting HIV, as the inflamed cervix provides an easier entry point for the virus during sexual activity.
It is essential to seek medical attention and receive appropriate treatment for cervicitis to prevent these complications.
- Complications of untreated cervicitis include:
- Pelvic inflammatory disease (PID)
- Spread of infection to uterus, fallopian tubes, and ovaries
- Severe pain
- Fertility problems
- Increased risk of ectopic pregnancies
- Increased risk of HIV infection during sexual activity
Prevention Of Cervicitis
Preventing cervicitis involves taking certain precautions. Consistent and correct use of condoms can greatly reduce the risk of contracting STIs, including those that can cause cervicitis. Being in a committed, monogamous relationship with a partner who is free of STIs also helps prevent cervicitis. It is important to be aware of one’s sexual health and undergo regular screenings for STIs to detect and treat any infections early on. Additionally, practicing good hygiene and avoiding potential allergens, such as certain contraceptive products or feminine hygiene products, can help prevent irritations and inflammations of the cervix.
- Consistent and correct use of condoms: This is a crucial step in preventing cervicitis as condoms act as a barrier and greatly reduce the risk of contracting STIs, including those that can cause cervicitis.
- Being in a committed, monogamous relationship: Being in a relationship with a partner who is free of STIs minimizes the chances of cervicitis transmission.
- Regular screenings for STIs: It is essential to be proactive about one’s sexual health by undergoing regular screenings for STIs. Early detection and treatment of any infections can prevent cervicitis.
- Practicing good hygiene: Maintaining good hygiene habits is important to prevent cervicitis. Avoiding potential allergens, such as certain contraceptive products or feminine hygiene products, can help prevent irritations and inflammations of the cervix.
Blockquote: “Prevention is always better than cure. Taking precautions, such as using condoms, being in a monogamous relationship, getting regular STI screenings, and practicing good hygiene, can significantly lower the risk of cervicitis.”
Location And Structure Of The Cervix
The cervix is situated within the pelvic cavity, about 3 to 6 inches inside the vaginal canal. It starts at the base of the uterus and descends towards the upper part of the vagina. The cervix has a wider middle portion and becomes narrower at both ends, which are the openings connecting to the uterus and vagina. It comprises various components, namely the internal os, endocervical canal, ectocervix, and external os. Together, these structures have a significant role in the female reproductive system and are susceptible to inflammation and infections.
- The cervix is located inside the pelvic cavity, approximately 3 to 6 inches inside the vaginal canal.
- It begins at the base of the uterus and extends downward onto the upper part of the vagina.
- The cervix is wider in the middle and narrows at both ends, where it opens into the uterus and vagina.
- The cervix consists of several parts, including the internal os, endocervical canal, ectocervix, and external os.
- These structures collectively play a vital role in the female reproductive system and can be affected by inflammation and infections.
The Transformation Zone
The transformation zone (TZ) of the cervix is the most common site for abnormal cell growth and is therefore of great significance in screening for cervical cancer. It refers to the area where different types of cells meet, and it is this zone that is examined during routine cervical screenings.
The TZ can undergo changes in response to menstrual cycle hormones, which affect the texture and location of the cervix. Understanding the transformation zone is crucial in detecting any abnormalities and addressing them promptly.
- The transformation zone (TZ) is the most common site for abnormal cell growth in the cervix.
- It is of great significance in screening for cervical cancer.
- The TZ is the area where different types of cells meet.
- Routine cervical screenings examine this zone.
- Menstrual cycle hormones can cause changes in the TZ, affecting the texture and location of the cervix.
- Understanding the transformation zone is crucial for detecting and addressing abnormalities promptly.
“Understanding the transformation zone is crucial in detecting any abnormalities and addressing them promptly.”
Anatomy Of The Cervix
The cervix is a vital component of the female reproductive system. It measures approximately an inch in length and can vary in size among women. Composed of fibromuscular tissue, the cervix is lined with glandular cells and squamous cells.
Notably, the outermost part of the cervix and the vagina are covered with different types of cells. The cervix itself contains two distinct cell types: columnar cells, which cover the inner part of the cervix, and squamous cells, which cover the outermost part of the cervix and extend into the vagina.
Understanding this intricate anatomy is crucial for maintaining and promoting overall reproductive health in females.
Importance Of Screening For Cervical Cancer
Regular screenings for cervical cancer are essential for early detection and treatment of abnormal cell growth in the cervix. By examining the transformation zone of the cervix, healthcare professionals can identify precancerous or cancerous changes and initiate appropriate interventions. Early detection and treatment greatly increase the chances of successful outcomes. Screening methods, such as the Pap test and HPV testing, are vital tools in preventing cervical cancer and ensuring the overall health and well-being of women. It is crucial for women to prioritize regular screenings and follow their healthcare providers’ recommendations.
💡
You may need to know these questions about cervix
What does the female cervix do?
The female cervix plays a pivotal role in reproductive processes. Acting as a gateway to the uterus, it facilitates the passage of sperm to reach and fertilize eggs. Additionally, when not in a state of pregnancy, it serves as a protective barrier against foreign substances such as tampons or bath water, ensuring that only necessary elements enter the body. During pregnancy, the cervix assists in maintaining the baby in the correct position until it achieves full development. Overall, the cervix acts as a crucial regulator in reproductive health and safeguarding the well-being of the female body.
What does it mean to feel your cervix?
Feeling your cervix can be an opportunity to gather valuable information about your reproductive health. The sensation of the cervix can vary depending on factors such as menstrual cycle phase. For some, it may feel soft and pliable, resembling the texture of the tip of your nose. Conversely, others describe it as a round structure with a slight impression in the middle, similar to a donut. These differences can indicate whether the cervix is open or closed, as well as its firmness. Monitoring these variations can aid in understanding one’s fertility and menstrual cycle patterns.
What does a low cervix look like?
The low cervix appears as the lowermost portion of the uterus, where it attaches to the vagina. It can be visually likened to a small round donut-shaped structure or a fleshy O, featuring a small central opening. Typically measuring around an inch or approximately 2.5 cm in diameter, its position may vary throughout the menstrual cycle.
Why does cervix pain happen?
Cervix pain can occur due to a condition called cervicitis, which is often caused by sexually transmitted infections (STIs). STIs such as gonorrhea, chlamydia, trichomoniasis, and genital herpes can lead to inflammation of the cervix, resulting in discomfort. These infections are typically transmitted through sexual contact, and if left untreated, they can cause irritation and inflammation in the cervix, leading to pain and discomfort. It is important to seek medical attention if experiencing cervix pain, as it may be a sign of underlying STIs that require treatment.
Reference source
https://medlineplus.gov/ency/article/002317.htm
https://my.clevelandclinic.org/health/body/23279-cervix
https://en.wikipedia.org/wiki/Cervix
https://integrisok.com/resources/on-your-health/2019/may/everything-you-need-to-know-about-your-cervix