Picture this: In a vibrant world of endless possibilities, where our bodies are temples of exploration and pleasure, lurks an invisible threat.
With a deceptive name like Cervical Intraepithelial Neoplasia (CIN), this mysterious villain hides in the shadows, affecting the lives of individuals from all walks of life, regardless of their sexual orientation or past encounters.
Unveiling the truth behind this silent danger, we delve into the world of human papillomavirus (HPV), unravelling its potential to transform innocent cells of the cervix into a catastrophic foe.
Brace yourself, for this is a story that concerns us all.
cin
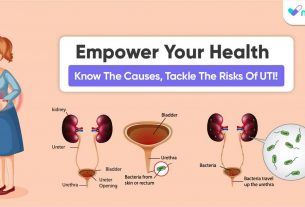
CIN (cervical intraepithelial neoplasia) is mainly caused by an infection called the human papilloma virus (HPV).
HPV is a common sexually transmitted infection that can affect the cervix.
There are over 100 types of HPV, but the high-risk types are the ones that cause abnormal cell changes in the cervix.
Usually, the body’s immune system can clear the infection without causing any symptoms or damage.
However, in some cases, the immune system fails to eliminate the virus, leading to prolonged HPV infection and potential damage to the cervix.
This damage may eventually develop into CIN.
HPV can be transmitted through various sexual activities, and using barrier contraception can reduce the risk but does not provide complete protection.
Cervical dysplasia, or CIN, is a precancerous condition where abnormal cells grow on the surface of the cervix.
Most people with cervical dysplasia do not develop cancer, and it takes years for cancer to form.
Cervical dysplasia mainly affects sexually active individuals assigned female at birth, and it is most common among women aged 25 to 35.
Key Points:
- CIN is caused by an infection called the human papilloma virus (HPV).
- HPV is a common sexually transmitted infection that can affect the cervix.
- There are over 100 types of HPV, but high-risk types cause abnormal cell changes in the cervix.
- In most cases, the immune system can clear the HPV infection without symptoms, but some cases lead to prolonged infection and potential cervix damage.
- HPV can be transmitted through sexual activities and using barrier contraception may reduce the risk but does not guarantee protection.
- Cervical dysplasia, or CIN, is a precancerous condition where abnormal cells grow on the cervix surface.
cin – Watch Video
💡
Pro Tips:
1. Cin, an abbreviation for “community information network,” was a popular term used in the late 1980s and 1990s to describe early online platforms and bulletin board systems (BBS) that connected people in local communities.
2. The legendary French film director Jean-Luc Godard famously said, “A story should have a beginning, a middle, and an end…but not necessarily in that order.” This unconventional approach to storytelling is evident in his influential film “Breathless” (? bout de souffle).
3. Did you know that the scent of cin, or cinnamon, has been found to improve cognitive function and memory? Research suggests that the aroma can enhance cognitive processing and boost performance on certain tasks.
4. Cin, a traditional Chinese word meaning “kindness” or “grace,” has deep cultural significance. It is often used to describe desirable qualities in individuals and is highly valued in Chinese society.
5. The island of C??n, located off the coast of Croatia, is home to an incredible phenomenon known as the Blue Cave. This natural wonder gets its name from the mesmerizing blue light that illuminates its interior, creating an otherworldly experience for visitors.
The Link Between Hpv And Cervical Intraepithelial Neoplasia (Cin)
Cervical intraepithelial neoplasia (CIN) is primarily caused by the human papillomavirus (HPV) infection. HPV, a common virus with over 100 strains, can affect the cervix. However, it’s essential to note that not all types of HPV lead to CIN. High-risk HPV strains specifically are responsible for causing abnormal cell changes in the cervix.
Please use bullet points at the end:
- Cervical intraepithelial neoplasia (CIN) is caused by the human papillomavirus (HPV) infection.
- HPV is a common virus with over 100 strains.
- Not all types of HPV lead to CIN.
- High-risk HPV strains cause abnormal cell changes in the cervix.
Understanding The Different Types Of Human Papillomavirus (Hpv)
The human papillomavirus (HPV) is a diverse group of over 100 strains. However, only certain strains affect the cervix and lead to the development of Cervical Intraepithelial Neoplasia (CIN). It is the high-risk HPV strains that are specifically associated with abnormal cell changes in the cervix and consequently pose an increased risk of cervical cancer.
- HPV comprises over 100 identified strains.
- Not all HPV strains affect the cervix or lead to CIN.
- The high-risk HPV strains are linked to abnormal cell changes in the cervix.
- High-risk HPV strains increase the risk of cervical cancer.
Remember, early detection and regular screenings play a crucial role in the prevention and early treatment of cervical cancer.
High-Risk Hpv: The Culprit Behind Abnormal Cell Changes In The Cervix
High-risk HPV strains are the specific types that cause abnormal cell changes in the cervix, leading to the development of CIN. While the body’s immune system is typically capable of naturally clearing the HPV infection, in some cases, the immune response is not sufficient in eliminating the virus. This can result in a persistent HPV infection, increasing the risk of cervix damage that may eventually progress to CIN.
- High-risk HPV strains cause abnormal cell changes in the cervix
- Immune system may not clear HPV infection in some cases
- Persistent HPV infection increases the risk of cervix damage
- Cervix damage can progress to CIN.
The Body’s Immune System And Hpv Infection Clearance
During an HPV infection, the body’s immune system plays a crucial role in clearing the virus naturally.
In many cases, the immune response is successful, leading to the elimination of the infection without any noticeable symptoms or long-term consequences.
However, in certain instances, the immune system fails to clear the infection completely, allowing the virus to persist in the body for extended periods.
To summarize:
- HPV infection triggers the body’s immune system response.
- Successful immune response leads to the elimination of the infection.
- In some cases, the immune system fails to clear the infection completely.
“The immune system is instrumental in clearing an HPV infection naturally.”
Prolonged Hpv Infection And Potential Cin Development
When the cervix is affected by an HPV infection over an extended period, it can result in damage that has the potential to progress to cervical intraepithelial neoplasia (CIN). CIN refers to a precancerous condition characterized by abnormal cell growth on the surface of the cervix. Not all individuals with CIN will develop cancer, and it often takes several years for cancer to form from this condition.
- Cervical intraepithelial neoplasia (CIN) is a precancerous condition caused by an HPV infection.
- Damage to the cervix from prolonged HPV infection can lead to CIN.
- CIN is characterized by abnormal cell growth on the cervix.
- Not all individuals with CIN will develop cancer.
- It takes several years for cancer to develop from CIN.
“CIN refers to a precancerous condition characterized by abnormal cell growth on the cervix.”
The Commonality Of Hpv Infections: Most People Experience It
HPV is an incredibly common virus, and most individuals will experience an HPV infection at some point in their lives. The widespread prevalence of HPV highlights the importance of understanding the risks and consequences associated with the virus. Being aware of the potential for HPV infection can empower individuals to take proactive steps in managing their sexual health.
Hpv And Sexual Orientation: Affects All Individuals Engaging In Sexual Activity
It is important to note that HPV can affect individuals of all sexual orientations who engage in sexual activity. This means that it can impact both people in long-term relationships as well as those who have not been sexually active for extended periods.
Additionally, the virus can live on the skin surrounding the entire genital area. It is highly transmissible through any type of sexual contact, regardless of whether it involves penetration or not.
To summarize:
- HPV can affect individuals of all sexual orientations, regardless of their relationship status or sexual activity history.
- The virus can be present on the entire genital area, making transmission possible through any type of sexual contact.
“It is essential to understand that HPV can affect individuals of all sexual orientations who engage in sexual activity.”
Hpv Transmission: More Than Just Penetrative Intercourse
Contrary to popular belief, HPV transmission is not limited to penetrative intercourse. The virus can be spread through any form of sexual contact, including skin-to-skin genital contact or sharing sex toys. This highlights the importance of practicing safe and responsible sexual behavior, regardless of the specific sexual activities involved.
- HPV transmission is not limited to penetrative intercourse
- The virus can be spread through any form of sexual contact, including skin-to-skin genital contact or sharing sex toys
Limited Protection With Barrier Methods Against Hpv
While using a condom or other barrier methods during sexual activity may provide some level of protection against HPV infection, it is essential to recognize their limitations. Barrier methods reduce the risk of transmission but do not guarantee complete protection. This is because HPV can infect regions that are not covered by the barrier, such as the surrounding skin areas. Therefore, it is crucial to combine barrier methods with regular HPV screenings and vaccinations to effectively reduce the risk.
- Barrier methods reduce the risk of transmission but do not guarantee complete protection.
- HPV can infect regions that are not covered by the barrier, such as the surrounding skin areas.
- Combine barrier methods with regular HPV screenings and vaccinations to effectively reduce the risk.
Cervical Dysplasia: A Precursor To Cervical Intraepithelial Neoplasia (Cin)
Cervical dysplasia, also known as cervical intraepithelial neoplasia (CIN), is a precancerous condition characterized by the growth of abnormal cells on the surface of the cervix. The severity of the cell changes determines the classification of CIN into different stages. CIN 1 refers to abnormal cells affecting approximately one-third of the epithelium’s thickness, while CIN 2 and CIN 3 involve abnormal cells affecting one-third to two-thirds and more than two-thirds of the epithelium, respectively.
Understanding the link between HPV and cervical intraepithelial neoplasia (CIN) is crucial for addressing the risks and consequences associated with HPV infections. The high-risk HPV strains are responsible for the abnormal cell changes in the cervix, and prolonged infections can lead to the development of CIN. It is important for sexually active individuals of all orientations to be aware of the transmission methods of HPV and the limitations of barrier methods in preventing infection.
To reduce the risk and impact of HPV and CIN, it is recommended to regularly undergo screenings, get vaccinations, and practice responsible sexual behavior. By staying informed, taking preventive measures, and seeking medical advice, individuals can minimize the potential harm caused by HPV and effectively manage CIN.
- Regular screenings
- Vaccinations
- Responsible sexual behavior
💡
You may need to know these questions about cin
What does CIN means?
CIN stands for cervical intraepithelial neoplasia, which refers to abnormal cell changes in the lining of the cervix. Although CIN is not cancerous itself, if left untreated, it can progress and develop into cervical cancer. Interestingly, CIN does not present any noticeable symptoms, highlighting the importance of regular screenings and early detection to effectively manage this condition.
What is CIN medical?
CIN medical, also known as cervical intraepithelial neoplasia (CIN), is a condition characterized by the presence of abnormal cells on the surface layer of the cervix. These cells have not yet invaded deeper tissues, and the term “intraepithelial” specifically highlights their location. The growth of these abnormal cells is referred to as neoplasia. CIN medical is an important term in the field of gynecology and is used to describe a specific stage of cervical dysplasia.
Is CIN 1 a cancer risk?
CIN 1, a low-grade lesion, poses a relatively low risk of developing into cancer. Studies have indicated that CIN 1 lesions have a higher likelihood of regressing rather than progressing to malignancy [7]. In contrast, higher-grade lesions like CIN 2 and CIN 3 have a greater potential for advancing towards cancer and a lower chance of regression [8-14]. Therefore, individuals diagnosed with CIN 1 can find solace in knowing that their cancer risk is relatively low, considering its higher regression potential.
How long does it take HPV to turn into CIN1?
Based on the observed data, it can be inferred that the development of CIN1 can occur relatively rapidly after the onset of persistent high-risk HPV infection. More than 50% of women in each age group were estimated to have developed CIN within 24 months, with at least 30% of women likely experiencing this progression within 12 months. This suggests a relatively quick timeline for the transformation of HPV into CIN1, emphasizing the importance of early detection and monitoring.
Reference source
https://www.macmillan.org.uk/cancer-information-and-support/worried-about-cancer/pre-cancerous-and-genetic-conditions/cin
https://my.clevelandclinic.org/health/diseases/15678-cervical-intraepithelial-neoplasia-cin
https://www.uptodate.com/contents/cervical-intraepithelial-neoplasia-management/print
https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2019.00976