The climacteric period: a time of change, a chapter in life shrouded with uncertainty and transformation.
As men and women venture into this mysterious realm, their bodies go through a series of alterations that can leave them grappling with a range of symptoms.
From the waning ability to reproduce to the enigmatic hormonal shifts, this is a stage like no other.
Join us as we delve into the intricacies of the climacteric period, unraveling its secrets and exploring the various treatment options that can ease the path to a harmonious transition.
climacteric period
The climacteric period refers to the midlife transition when fertility declines.
In men, this can result in a reduction in their ability to reproduce.
Women, on the other hand, lose their ability to reproduce once they reach menopause.
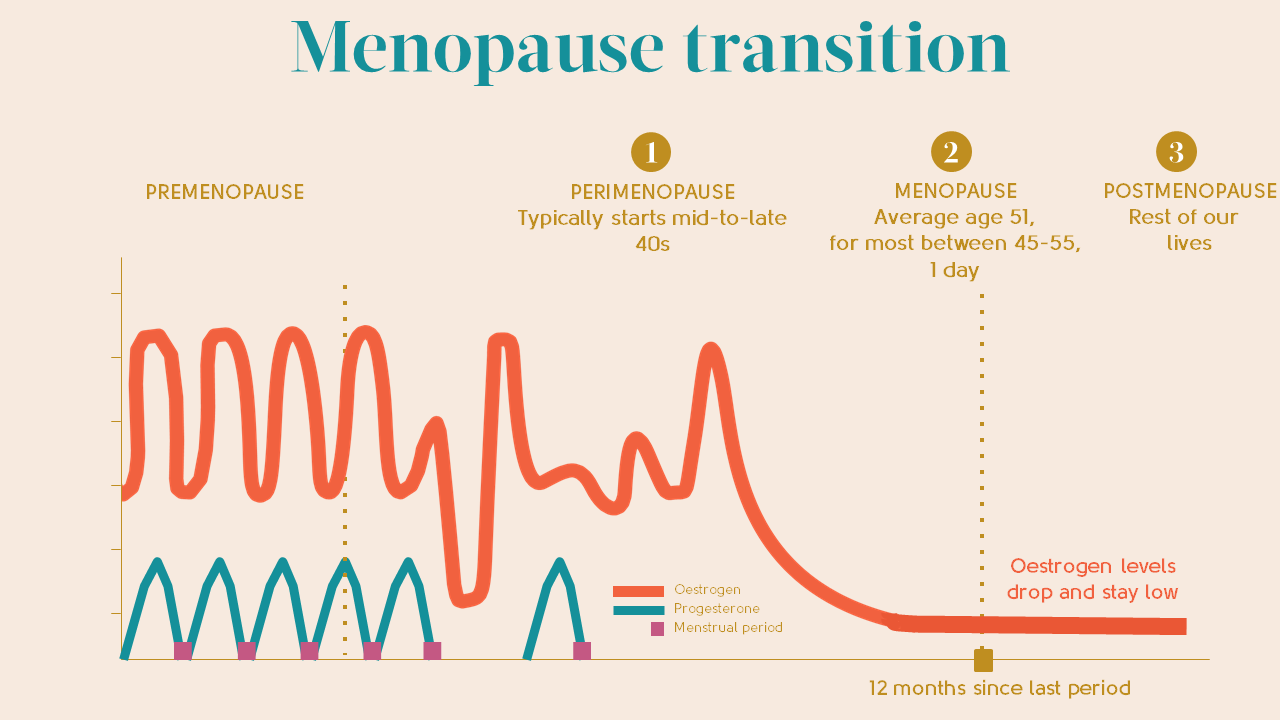
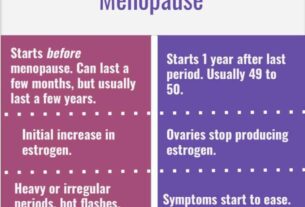
Perimenopause is a period of transition in which a woman’s ovaries stop releasing eggs and the production of estrogen and progesterone decreases.
Menopause is defined as 12 months without menstruation, typically occurring around the age of 51.
Symptoms of perimenopause and menopause, caused by decreased production of estrogen and progesterone, include difficulty sleeping, hot flashes, vaginal dryness, thinning of the vaginal wall, decreased bone mass leading to osteoporosis, depression, irritability, and weight gain.
While hormone replacement therapy was once common, concerns about its potential risks have led to a decrease in its prescription for menopausal women.
Other treatment options include lower doses of estrogen, frequent exams, lifestyle adjustments, and alternative therapies.
Men in middle adulthood may experience erectile dysfunction (ED), with intermittent ED affecting up to 50% of men between 40 and 70 years old.
Chronic ED affects approximately 30 million men in the United States.
Causes of ED include medical conditions and psychological factors, with diseases accounting for the majority of cases.
Low testosterone levels can also contribute to symptoms such as low sex drive, ED, fatigue, loss of muscle, and breast enlargement.
Supplemental testosterone effectiveness is varied, and long-term replacement therapy can increase the risk of certain health issues.
However, it is important to note that most men with low testosterone do not experience related problems.
Key Points:
- Climacteric period is the midlife transition when fertility declines
- Men experience a reduction in their ability to reproduce during this period
- Women lose their ability to reproduce once they reach menopause
- Perimenopause is a transition period when a woman’s ovaries stop releasing eggs and hormone production decreases
- Menopause is defined as 12 months without menstruation and typically occurs around age 51
- Symptoms of perimenopause and menopause include:
- Difficulty sleeping
- Hot flashes
- Vaginal dryness
- Depression
- Weight gain
climacteric period – Watch Video
💡
Pro Tips:
1. The climacteric period, also known as menopause, occurs in women typically between the ages of 45 and 55. However, in rare cases, it can start as early as the late 30s or early 40s, which is known as early or premature menopause.
2. Contrary to popular belief, the term “climacteric” doesn’t only refer to menopause in women. In men, it is referred to as “andropause” or “late-onset hypogonadism.” Andropause usually occurs later in life, generally between the ages of 40 and 60, and is characterized by a gradual decline in testosterone production.
3. The climacteric period is not exclusive to humans; other primates and mammals also experience a similar transition. For example, female chimpanzees also undergo what can be considered a form of menopause, where they cease to have reproductive potential but still live for many years after.
4. The climacteric period can vary across cultures and societies. While some cultures perceive menopause as a challenging and negative stage in a woman’s life, others view it as a time of liberation and newfound wisdom. Societal beliefs and cultural attitudes regarding aging and menopause shape women’s experiences during this period.
5. The climacteric period is not only associated with physical changes but also emotional and psychological ones. Some women may experience mood swings, irritability, depression, anxiety, and decreased libido, among other symptoms. However, it is important to note that every person’s experience during this time can be vastly different, and not all women will exhibit the same symptoms or intensity.
Definition of Climacteric Period and Fertility Decline
The climacteric period, also known as the midlife transition, is the phase in a person’s life when fertility declines. It is a natural process that both men and women go through as they age.
During this period, individuals may notice changes in their reproductive abilities, which can have significant physical and emotional effects.
- Some key points to remember about the climacteric period:
- It is a phase when fertility declines.
- It affects both men and women.
- It is a natural process associated with aging.
- Changes in reproductive abilities can occur.
“As we age, the climacteric period marks a significant transition in our reproductive abilities.”
Male Experience of Reduced Reproductive Ability during Climacteric Period
Men also experience a decline in their ability to reproduce as they enter the climacteric period. This reduction in fertility is primarily caused by a decrease in testosterone levels. Testosterone is the hormone responsible for sperm production and overall sexual function in men. As levels decline, men may notice a decrease in their sex drive, and they may also experience difficulties in achieving and maintaining an erection. These changes can be distressing and significantly impact their quality of life.
Women’s Loss of Reproductive Ability at Menopause
The climacteric period for women is marked by menopause, which signifies the end of their reproductive ability. Menopause is officially defined as the absence of menstruation for 12 consecutive months and typically occurs around the age of 51.
During menopause, women’s ovaries cease the release of eggs, and there is a notable decline in the production of estrogen and progesterone, the vital reproductive hormones. Consequently, women no longer undergo menstrual cycles or ovulation.
-Bullet points:
- Menopause is the conclusion of the climacteric period for women and signifies the cessation of their reproductive capability.
- Menopause is defined as the absence of menstruation for 12 consecutive months and typically occurs around the age of 51.
- During menopause, women’s ovaries stop releasing eggs.
- The production of estrogen and progesterone, the primary reproductive hormones, decreases significantly.
- Consequently, women no longer experience menstrual cycles or ovulation.
Perimenopause: Transition Period and Hormonal Changes
Before reaching menopause, women go through a transitional phase called perimenopause. This period can last for several years and is characterized by erratic menstrual cycles and hormonal fluctuations. As the ovaries gradually cease to function, estrogen and progesterone levels fluctuate, leading to various physical and emotional symptoms. The irregularity of menstrual cycles and the changing hormone levels can cause discomfort and uncertainty for many women during perimenopause.
Menopause and its Definition and Average Age
Menopause is officially diagnosed after 12 consecutive months without menstruation. The average age at which women experience menopause is around 51. However, it is important to note that the timing can vary significantly from person to person. Some women may enter menopause earlier, while others may undergo the transition later in life.
- Key points:
- Menopause is diagnosed after 12 consecutive months without menstruation.
- Average age of menopause is around 51.
- Timing can vary significantly from person to person.
“The timing of menopause can vary greatly between individuals.”
Symptoms of Perimenopause and Menopause
The symptoms experienced during perimenopause and menopause are primarily attributed to the decreased production of estrogen and progesterone. These symptoms can vary widely among individuals but commonly include:
- Difficulty falling asleep
- Hot flashes
- Night sweats
- Vaginal dryness
- Pain during intercourse
- Thinning of the vaginal walls
- Decreased bone mass leading to osteoporosis
- Depression
- Irritability
- Weight gain
These symptoms can significantly impact a woman’s daily life and overall well-being.
Concerns around Hormone Replacement Therapy
In the past, hormone replacement therapy (HRT) was commonly prescribed to alleviate the symptoms of menopause. However, concerns about its long-term health risks have led to a decrease in its usage. HRT has been associated with an increased risk of breast cancer, stroke, and the development of other conditions. As a result, many healthcare professionals now carefully evaluate the necessity and suitability of HRT for each individual, considering their specific risk factors and symptoms.
- HRT was commonly prescribed to alleviate menopause symptoms
- Concerns about long-term health risks reduced its usage
- Increased risk of breast cancer and stroke associated with HRT
- Healthcare professionals evaluate necessity and suitability considering risk factors and symptoms.
Treatment Options for Menopausal Symptoms
Although most women do not experience severe enough symptoms to require estrogen or hormone replacement therapy, there are various treatment options available to manage menopausal symptoms. These options include:
- Lower doses of estrogen
- Frequent medical check-ups
- Lifestyle adjustments such as avoiding caffeine and alcohol
- Incorporating soy into the diet
- Remaining sexually active
- Practicing relaxation techniques
- Using water-based lubricants
It is essential for women to consult with their healthcare providers to discuss the best approach for managing their specific symptoms.
Cultural Influences on Menopausal Experience
Studies have consistently shown that menopausal symptoms vary across countries, regions, and ethnic groups. Cultural influences play a significant role in how menopause is experienced and perceived.
For example, some cultures do not have specific words for menopausal symptoms, and women in these cultures may not experience certain symptoms commonly associated with menopause.
Furthermore, different cultures have different perspectives on menopause, with some viewing it as a loss and others as a liberating experience.
For instance, in India, 94% of women welcomed menopause as it signified a gain in status and freedom from menstrual restrictions.
Erectile Dysfunction in Middle Adulthood and its Causes
In middle adulthood, erectile dysfunction (ED) becomes more common among men. Studies show that intermittent ED affects as many as 50% of men between the ages of 40 and 70. Approximately 30 million men in the United States experience chronic ED. The causes for ED can be both medical and psychological. Medical conditions such as diabetes, kidney disease, alcoholism, and atherosclerosis can contribute to ED. Atherosclerosis, in particular, occurs when plaque builds up in the arteries, restricting blood flow to the penis, thus causing difficulties in achieving or maintaining an erection. Psychological factors, including stress, anxiety, and depression, can also play a significant role in the development of ED.
To conclude, the climacteric period is a significant life transition that both men and women experience as they age. Understanding the physical and emotional changes that occur during this period is essential for individuals to navigate this phase of their lives successfully. By being aware of the symptoms and treatment options available, individuals can make informed choices and seek appropriate support to manage any challenges that may arise during the climacteric period.
💡
You may need to know these questions about climacteric period
What is the difference between climacteric and menopause?
The climacteric and menopause are both related to the end of reproductive function in women, but they differ in terms of the overall timeline and specific events. The climacteric refers to the period starting from normal ovarian function and gradually leading to the afollicular nadir, or the lowest point, of ovarian activity. During this time, women may experience a variety of physical and hormonal changes. On the other hand, menopause specifically refers to a woman’s final menstrual period, marking the cessation of fertility. It is considered the endpoint of the climacteric phase and is characterized by a significant decrease in ovarian function and the absence of future menstruation.
What changes occur during the climacteric?
The climacteric, also known as perimenopause, marks the transitional period leading up to menopause. During this stage, women may experience a range of changes in their menstrual cycles. Some may notice that their cycles become shorter or longer than usual, with irregularity becoming more common. Additionally, the amount of menstrual bleeding may vary, leading to lighter or heavier periods. These changes serve as early indications that menopause is approaching, as women may start experiencing the first symptoms associated with this natural transition.
What is the climacteric in middle adulthood?
The climacteric in middle adulthood refers to the transitional period characterized by a decline and eventual cessation of ovarian activity and function, known as peri-menopause and post-menopause. This is accompanied by hormonal changes, including a decrease in estrogen levels, resulting in noticeable shifts in menstrual cycles. During peri-menopause, women may experience irregular periods, while post-menopause denotes the complete end of menstruation. These physiological changes mark an important stage in a woman’s life, with potential implications for physical and psychological well-being.
Can a woman have an Orgasim after menopause?
Yes, a woman can have an orgasm after menopause. Although menopause may bring changes to a woman’s body, it does not mean the end of sexual enjoyment. In fact, many women find that their sex life improves after menopause. By exploring new techniques, communicating with their partner(s), and prioritizing pleasure, women can continue to experience fulfilling orgasms and maintain a satisfying sex life well into their menopausal years. Embracing the changes and being open to new possibilities can lead to a fulfilling and pleasurable sexual experience for women post-menopause.
Reference source
https://pubmed.ncbi.nlm.nih.gov/12188398/
https://agsjournals.onlinelibrary.wiley.com/doi/full/10.1111/j.1532-5415.1982.tb05661.x
https://bocahindonesia.com/en/klimakterium/
https://www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397