Imagine a world where the most basic of human experiences seems impossible.
Where the absence of a vital part of female anatomy poses a unique challenge.
This is the reality for those diagnosed with congenital absence of vagina, a condition known as vaginal agenesis.
But fear not – medical advancements and a holistic approach to care are paving the way for hope and healing.
Dive into the intricacies of this condition and discover the innovative treatments and support systems that are transforming lives at the Center for Young Women’s Health.
congenital absence of vagina
Congenital absence of the vagina, also known as vaginal agenesis, is a condition where a female is born without a vagina.
This condition can be diagnosed through external and internal exams, ultrasounds, MRIs, and karyotyping to identify any genetic causes.
Treatment for vaginal agenesis can be delayed, allowing the patient to choose the timing and readiness for treatment.
The American College of Obstetricians and Gynecologists recommend creating a vagina through the use of vaginal dilators.
Dilators should be used twice a day for 15 to 20 minutes, with the success rate depending on consistent and frequent use.
Vaginal dilatation does not impact orgasmic function or lubrication, but water-based lubricant can be used for intercourse if necessary.
Medical centers specializing in treating vaginal agenesis, such as the Center for Young Women’s Health, provide a multidisciplinary team approach, offering testing, treatment, counseling, and follow-up services to empower young women and address both the physical and emotional effects of this condition.
Key Points:
- Congenital absence of the vagina is a condition where a female is born without a vagina.
- Diagnosis can be done through external and internal exams, ultrasounds, MRIs, and karyotyping.
- Treatment can be delayed, allowing the patient to choose the timing and readiness for treatment.
- The American College of Obstetricians and Gynecologists recommend creating a vagina through the use of vaginal dilators.
- Success rate of vaginal dilatation depends on consistent and frequent use.
- Medical centers specializing in treating vaginal agenesis provide a multidisciplinary team approach, offering testing, treatment, counseling, and follow-up services.
congenital absence of vagina – Watch Video
💡
Pro Tips:
1. Congenital Absence of Vagina Trivia:
1. In medical terms, the congenital absence of a vagina is known as Mayer-Rokitansky-Küster-Hauser syndrome (MRKH syndrome). It affects approximately 1 in every 4,500 women worldwide.
2. MRKH syndrome is typically diagnosed during adolescence when a girl fails to menstruate, despite having all other signs of puberty. However, with modern technology, it can now be diagnosed even before adolescence using ultrasound and MRI scans.
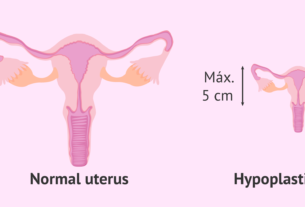
3. People with MRKH syndrome often have normal external genitalia, including a functioning clitoris, labia, and other structures. However, the vagina is either absent or underdeveloped.
4. Although MRKH syndrome affects the reproductive system, it does not affect a person’s ability to have sexual pleasure or experience arousal. It is possible for individuals with MRKH to have a fulfilling sex life through various methods, including surgery or the use of dilation techniques.
5. Treatment options for MRKH syndrome include surgical procedures to create a functional vagina, such as vaginoplasty or dilation therapy. In recent years, there have been significant advancements in reconstructive surgical techniques, enabling individuals with MRKH syndrome to have a fully functional and anatomically correct vagina.
Congenital Absence Of Vagina
Congenital absence of vagina, also known as vaginal agenesis, is a rare condition in which a female is born without a vagina or has an underdeveloped or partial vagina. This condition is often caused by a failure of the Mullerian ducts, which are responsible for the development of the female reproductive system, to fuse properly during embryonic development.
Vaginal agenesis affects approximately 1 in 5,000 females.
Diagnosis And Treatment Options
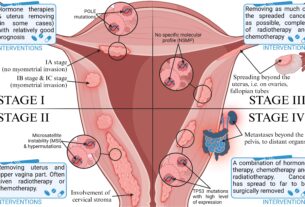
Diagnosing vaginal agenesis typically involves a comprehensive evaluation by a healthcare professional. External and internal physical exams are conducted to assess the absence or underdevelopment of the vagina. Additionally, ultrasounds and MRIs may be used to visualize the reproductive tract and confirm the diagnosis. Karyotyping, a genetic test, may also be performed to identify any underlying genetic causes of vaginal agenesis.
Once diagnosed, treatment options for vaginal agenesis can vary depending on the individual’s preferences, readiness, and overall health. Delayed treatment is an option for some individuals who may choose to delay or forgo treatment until they feel ready. It is important for healthcare providers to respect the patient’s choice in timing and readiness for treatment.
External And Internal Exams
During the external examination for vaginal agenesis, healthcare providers assess the external genitalia to identify any physical abnormalities or absence of the vaginal opening. They may also evaluate the presence or absence of other secondary sexual characteristics, such as pubic hair or breast development.
Internal exams are crucial for a definitive diagnosis of vaginal agenesis. This involves using a speculum to visualize the internal reproductive organs, including the cervix, uterus, fallopian tubes, and ovaries. In cases of vaginal agenesis, the absence or underdevelopment of the vagina is apparent during the internal exam.
Ultrasounds And MRIs For Diagnosis
Ultrasounds and MRIs: Diagnostic Imaging Techniques for Vaginal Agenesis
Ultrasounds and MRIs play a crucial role in diagnosing vaginal agenesis, a condition characterized by the underdevelopment or absence of the vagina. These advanced imaging techniques provide detailed insights into the internal reproductive structures, aiding healthcare providers in making accurate diagnoses and determining the most suitable treatment strategy for each patient.
Ultrasound:
- Utilizes sound waves to create images
- Particularly effective in visualizing reproductive organs
- Helps confirm the absence or underdevelopment of the vagina
MRI:
- Relies on a magnetic field and radio waves to produce detailed images
- Provides in-depth visualization of internal structures
By employing ultrasound and MRI, healthcare professionals can obtain a comprehensive view of the reproductive system, enabling them to identify the root cause of the condition and devise an optimal treatment plan.
“Accurate diagnosis is the cornerstone of effective treatment.” – Unknown
In conclusion, ultrasounds and MRIs are invaluable tools in the diagnosis of vaginal agenesis. These imaging techniques empower healthcare providers to evaluate the internal reproductive structures and determine the most appropriate course of action, ultimately improving the overall care and well-being of patients.
Karyotyping For Genetic Causes
Karyotyping, a genetic test, is often recommended to identify any underlying genetic causes of vaginal agenesis. This test involves analyzing the chromosomes to detect any abnormalities or genetic variations that may contribute to the condition.
In some cases, vaginal agenesis may be associated with certain genetic syndromes or chromosomal abnormalities. Identifying these genetic causes can help healthcare providers tailor treatment plans and provide appropriate counseling and support to affected individuals and their families.
Delayed Treatment Considerations
For individuals with vaginal agenesis, delaying or forgoing treatment until they feel ready can be a viable option. This approach allows them to have sufficient time and space to make informed decisions about their healthcare.
It is of utmost importance for healthcare providers to respect and support the individual’s choice regarding the timing and readiness for treatment. By fostering open and honest communication, healthcare providers can ensure that the individual’s needs, concerns, and preferences are thoroughly considered throughout the treatment process.
- Delaying or forgoing treatment can allow individuals with vaginal agenesis to have more control over their own healthcare decisions.
- Taking the time to make informed decisions can lead to better overall satisfaction with the chosen treatment approach.
- Healthcare providers should actively listen and provide support during discussions about treatment options.
- Respecting the individual’s autonomy and agency is crucial for a successful treatment experience.
“The individual’s autonomy and agency in deciding the timing and readiness for treatment should be highly regarded and supported.”
Patient’s Choice In Timing And Readiness
Empowering individuals to make decisions regarding their own healthcare is a central tenet in the management of vaginal agenesis. Each person’s journey is unique, and their readiness for treatment may vary.
Proper counseling and education about available treatment options and their potential outcomes are vital. By providing individuals with comprehensive information about the benefits, risks, and alternatives of various treatments, healthcare providers support patients in making well-informed decisions that are right for them.
- Key points to consider:
- Each person’s journey is unique
- Readiness for treatment may vary
- Proper counseling and education are vital
- Comprehensive information on treatment options
- Benefits, risks, and alternatives should be discussed
- Support patients in making well-informed decisions
“Empowering individuals to make decisions regarding their own healthcare is crucial in managing vaginal agenesis.”
Creating A Vagina With Dilators
A widely accepted and highly successful treatment for vaginal agenesis is the use of vaginal dilators to create a functional vagina. The American College of Obstetricians and Gynecologists (ACOG) recommends the use of vaginal dilators as the first-choice treatment for vaginal agenesis.
The process involves inserting a series of progressively larger dilators into the vagina over time to gradually stretch and expand the vaginal tissues. This allows for the development of a functional vagina. Dilators are typically used twice a day for 15 to 20 minutes, and consistent and frequent use is key to the success of dilation.
- Vaginal dilators are a widely accepted and successful treatment for vaginal agenesis.
- Recommended by the American College of Obstetricians and Gynecologists (ACOG).
- Insert progressively larger dilators to stretch and expand vaginal tissues.
- Consistent and frequent use is essential for successful dilation.
“The use of vaginal dilators is the recommended first-choice treatment for vaginal agenesis.”
ACOG’s Recommendation On Dilators
The American College of Obstetricians and Gynecologists (ACOG) strongly supports the use of vaginal dilators as a safe and effective treatment for vaginal agenesis. Dilators provide a non-surgical and non-hormonal alternative for creating a neovagina and restoring normal sexual function, including the potential for orgasm.
To ensure the maximum effectiveness of dilators, it is crucial to adhere to a prescribed schedule and technique. Healthcare providers may suggest using a water-based lubricant to facilitate the insertion and removal of dilators whenever necessary.
Frequency And Consistency Of Dilation Success
The success of vaginal dilatation for treating vaginal agenesis is highly dependent on the frequency and consistency of use. Regular and diligent use of dilators is essential in achieving successful dilation and maintaining a functional vagina.
Healthcare providers will typically provide guidance on the appropriate frequency, duration, and pressure of dilation. It may take several months to years of consistent and frequent use of dilators to achieve the desired results. However, with dedication and adherence to the recommended regimen, the vast majority of individuals with vaginal agenesis can successfully develop a functional vagina.
In conclusion, vaginal agenesis is a rare condition that can have significant physical and emotional implications for affected individuals. However, with appropriate diagnosis, treatment, and support, individuals with vaginal agenesis can lead healthy and fulfilling lives. The combination of medical expertise, counseling, and support services provided by specialized medical centers such as the Center for Young Women’s Health (CYWH) ensures accurate diagnoses, exceptional care, and empowering resources for those navigating the challenges of vaginal agenesis.
- Vaginal dilatation is crucial for treating vaginal agenesis
- Regular and diligent use of dilators is essential
- Healthcare providers provide guidance on frequency, duration, and pressure
- Achieving desired results may take several months to years
- Adherence to the recommended regimen is key
- Appropriate diagnosis, treatment, and support are important for individuals with vaginal agenesis
- Specialized medical centers like the Center for Young Women’s Health (CYWH) provide accurate diagnoses, exceptional care, and resources for those with vaginal agenesis.
💡
You may need to know these questions about congenital absence of vagina
What is a congenital absence in a female?
Congenital absence in a female refers to a condition known as Rokitansky syndrome, Mayer-Rokitansky-Kuster-Hauser syndrome, vaginal agenesis, or vaginal aplasia. This rare condition is characterized by the absence or underdevelopment of the vagina since birth. While there are several recent reviews available regarding this condition, its impact on a woman’s reproductive and sexual health can vary, making it an important area of study for medical professionals.
1. How does the congenital absence of vagina impact a person’s overall reproductive health and fertility?
Congenital absence of the vagina, also known as Mayer-Rokitansky-Kuster-Hauser syndrome, affects a person’s overall reproductive health and fertility in various ways. The condition is characterized by the absence or underdevelopment of the vagina, often accompanied by underdeveloped or absent uterus. While individuals with this condition have normally functioning ovaries, their inability to conceive and carry a pregnancy to term is a challenge.
Without a functional vagina, sexual intercourse and natural reproduction become impossible. However, this does not necessarily affect a person’s fertility if they desire to have biological children. Assisted reproductive technologies (ART), such as in vitro fertilization (IVF) or uterine transplantation, can offer solutions. If the individual has a functioning uterus, they may be able to receive an embryo created from their own eggs and a partner’s sperm, or they can choose to use a gestational carrier. Thus, while the congenital absence of the vagina impacts reproductive health, it does not necessarily mean a person is infertile, as alternative options can be pursued to overcome the challenge.
2. What are the available treatment options for individuals with congenital absence of vagina, and what are the potential outcomes and long-term effects of these treatments?
There are several treatment options available for individuals with congenital absence of vagina. One option is surgical creation of a neo-vagina, where a canal is constructed using a variety of techniques, such as using a section of the sigmoid colon or peritoneum. Another option is the use of dilation therapy, where a dilator is inserted regularly to gradually enlarge the vaginal opening.
The potential outcomes of these treatments vary depending on individual factors and specific techniques used. Surgical creation of a neo-vagina can result in the formation of a functional and anatomically similar vaginal canal. However, there may be risks associated with surgery, such as infection or complications from the use of a graft. Dilation therapy can also be a successful option in creating a functional neo-vagina, but it requires regular and consistent adherence to the therapy.
In terms of long-term effects, the vast majority of individuals can achieve satisfactory sexual function and have the ability to conceive and carry a pregnancy to term after successful treatment. However, it is important to note that every case is unique and outcomes can vary. Some individuals may experience psychological or emotional challenges related to body image or intimacy. It is crucial for individuals to receive comprehensive care, including counseling and support, to address any potential long-term effects and ensure overall well-being.
3. How does the psychological well-being of individuals with congenital absence of vagina typically differ from those without this condition, and what support systems or interventions are available to address any associated emotional challenges?
Individuals with congenital absence of vagina may face unique psychological challenges compared to those without this condition. The absence of a vagina can cause feelings of embarrassment, shame, and low self-esteem. It may also affect intimate relationships and sexual experiences. This difference in physical anatomy can lead to psychological distress and a sense of isolation.
Support systems and interventions are available to address the emotional challenges associated with this condition. Psychological counseling can be beneficial in helping individuals cope with their emotions, improve self-esteem, and develop healthy coping mechanisms. Support groups can provide a sense of community and allow individuals to connect with others who have similar experiences. In some cases, medical interventions such as surgical reconstruction or the use of medical devices may also be available to help individuals with this condition. Overall, a comprehensive approach involving emotional support, counseling, and potential medical interventions can help individuals with congenital absence of vagina navigate the associated emotional challenges and improve their psychological well-being.
Reference source
https://www.childrenshospital.org/conditions/vaginal-agenesis
https://link.springer.com/chapter/10.1007/978-1-4613-9086-2_19
https://www.mayoclinic.org/diseases-conditions/vaginal-agenesis/symptoms-causes/syc-20355737
https://pubmed.ncbi.nlm.nih.gov/782313/