Congenital heart disease – a term that holds within it a world of complexity, mystery, and resilience.
It touches the lives of 1% of newborns, encompassing a myriad of conditions from stenosis to transposition of the great arteries.
With symptoms that range from difficulty breathing to a bluish tint on the skin, its impact is profound.
But fear not, for medical advancements have paved the way for early diagnosis and treatments that offer hope for affected individuals.
Join us as we delve into the world of congenital heart disease, where resilience and innovation converge to create a path towards normal, healthy lives.
Get ready to be captivated by a tale of strength, courage, and triumph over adversity.
congenital heart disease
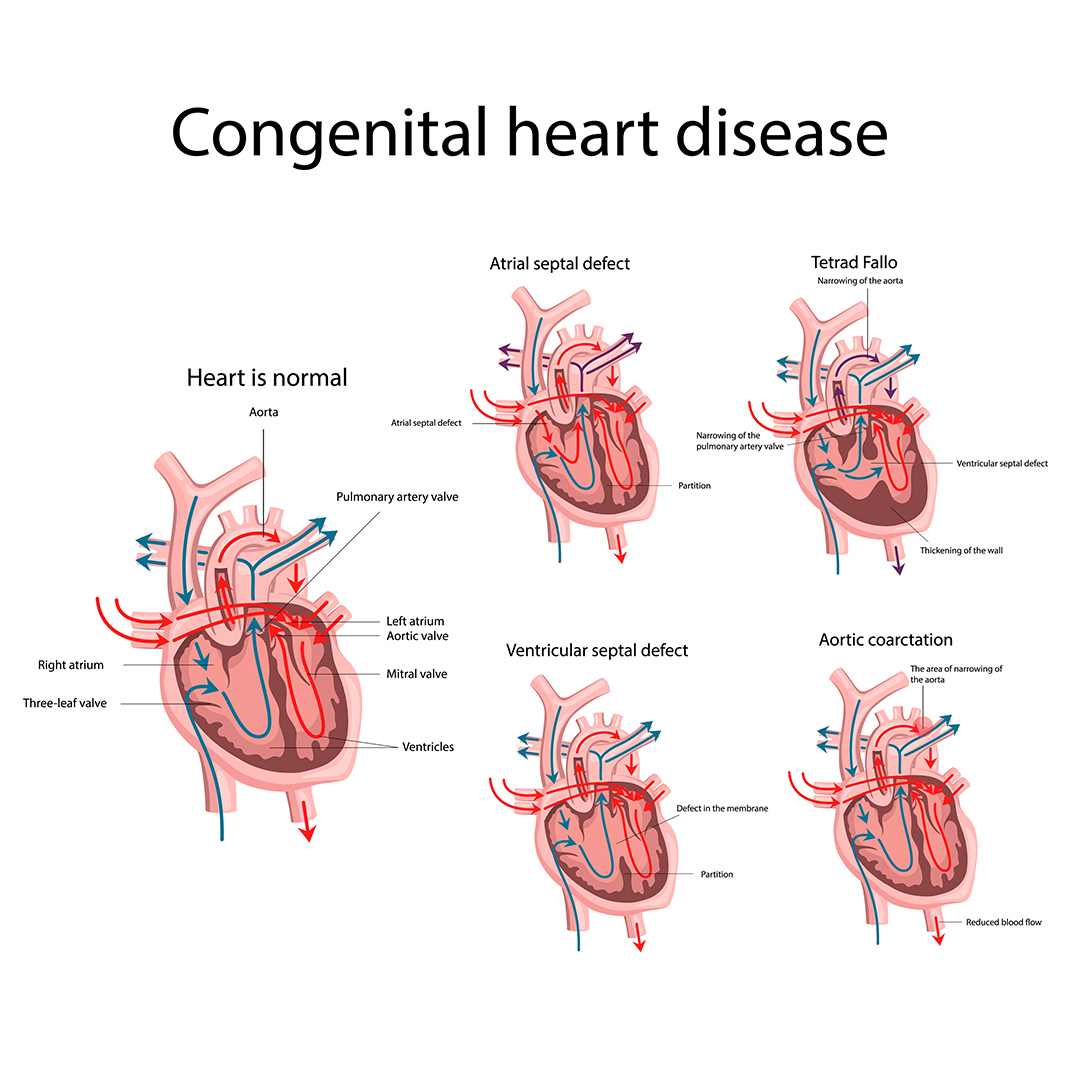
Congenital heart disease refers to a range of heart defects that are present at birth.
These defects can range from simple stenosis to complex conditions such as Tetralogy of Fallot, Transposition of the great arteries, and Hypoplastic left heart syndrome.
It is the most common birth defect, affecting approximately 1% of all newborns.
Possible causes include certain genetic conditions, maternal age over 40, and a family history of heart defects.
Symptoms may include difficulty breathing, poor feeding, and a bluish tint to the skin or lips.
Early diagnosis and treatment are crucial for a better prognosis.
Treatment options include medications, catheter procedures, and surgery.
With proper medical care and long-term follow-up, individuals with congenital heart disease can lead normal, healthy lives, although potential complications may arise.
Key Points:
- Congenital heart disease is a range of heart defects present at birth.
- The defects can range from simple stenosis to complex conditions such as Tetralogy of Fallot, Transposition of the great arteries, and Hypoplastic left heart syndrome.
- It is the most common birth defect, affecting approximately 1% of all newborns.
- Possible causes include certain genetic conditions, maternal age over 40, and a family history of heart defects.
- Symptoms may include difficulty breathing, poor feeding, and a bluish tint to the skin or lips.
- Treatment options include medications, catheter procedures, and surgery.
congenital heart disease – Watch Video
💡
Pro Tips:
1. Congenital heart disease affects approximately 8 in every 1,000 newborns in the United States, making it the most common birth defect.
2. The earliest known case of congenital heart disease was discovered in the remains of a baby buried in Egypt over 3,500 years ago.
3. Contrary to popular belief, congenital heart disease is not solely a pediatric condition, as many individuals live into adulthood with the condition.
4. Famous American actress and singer Marylin Monroe had a congenital heart defect called a patent foramen ovale, which is a small hole in the heart that should have closed after birth.
5. A rare form of congenital heart disease called Tetralogy of Fallot was discovered in 1672 by a French physician named ??tienne-Louis Arthur Fallot, who described the four specific heart abnormalities characteristic of the condition.
Complex Defects
Congenital heart disease (CHD) is a term used to describe a variety of structural abnormalities that impact the heart and its major vessels. Stenosis, the narrowing of blood vessels or valves, is a complex defect frequently observed in CHD. This condition has the potential to restrict blood flow, resulting in a range of complications and symptoms. Important structures that can be affected by stenosis in CHD include valves, arteries, and chambers of the heart.
Tetralogy Of Fallot
Tetralogy of Fallot (TOF) is a specific type of complex congenital heart defect characterized by four distinct abnormalities. These include a ventricular septal defect (VSD), right ventricular hypertrophy, pulmonary stenosis, and an overriding aorta.
These abnormalities disrupt the normal flow of oxygenated and deoxygenated blood in the heart, leading to various symptoms. Some common symptoms of TOF include cyanosis (a bluish tint to the skin), fatigue, and difficulty breathing.
TOF is a condition that requires medical attention, and treatment often involves surgery to correct the abnormalities and improve the overall function of the heart. Early diagnosis and intervention are crucial for managing TOF effectively.
Transposition Of The Great Arteries
Transposition of the great arteries (TGA) is a complex defect characterized by the switching of the positions of the pulmonary artery and the aorta. This abnormality results in the presence of two parallel circulatory systems. In this condition, oxygenated blood flows to the body, while deoxygenated blood returns to the lungs without being properly oxygenated. As a consequence, infants with TGA often experience cyanosis, a bluish discoloration of the skin, shortly after birth. Surgery is required to correct this defect and restore normal blood flow.
Hypoplastic Left Heart Syndrome
Hypoplastic left heart syndrome (HLHS) is a complex defect characterized by underdevelopment of the left side of the heart, including the left ventricle, mitral valve, and aortic valve.
As a result, the right side of the heart has to pump blood to both the lungs and the body, leading to a strain on the heart.
Symptoms of HLHS can include poor feeding, rapid breathing, and cyanosis.
Treatment usually involves a series of surgeries to reroute blood flow and restore function to the heart.
Most Common Birth Defect
Congenital heart disease (CHD) is the most common birth defect worldwide, affecting approximately 1% of all newborns. This high prevalence makes CHD a significant health concern that requires attention in terms of diagnosis, treatment, and prevention strategies. Raising awareness about CHD is crucial to ensure early diagnosis and intervention for affected individuals.
1% Of All Newborns Affected
Out of all newborns, approximately 1% are affected by congenital heart disease (CHD). This statistic emphasizes the significant impact of CHD on the pediatric population. Efforts must be made to educate healthcare providers and parents about the signs and symptoms of CHD to ensure early detection and intervention for affected infants.
Possible Causes
The causes of congenital heart defects, including stenosis, are not fully understood. However, research suggests that a combination of genetic and environmental factors may contribute to their development. Genetic mutations, chromosomal abnormalities, and maternal health conditions such as diabetes are believed to play a role in the occurrence of CHD. Furthermore, specific medications taken during pregnancy and exposure to environmental toxins have been associated with an increased risk of CHD.
Risk Factors
While the precise causes of congenital heart disease (CHD) are not fully understood, several risk factors have been identified:
- Maternal age over 40 is associated with an increased risk of having a child with CHD.
- Certain genetic conditions, such as Down syndrome and Turner syndrome, are also known to be linked to heart defects.
- Having a family history of heart defects increases the likelihood of having a child with CHD.
These risk factors emphasize the need for early detection and intervention to ensure the best possible outcomes for infants with CHD.
Maternal Age Over 40
Maternal age over 40 is a noteworthy risk factor for the development of congenital heart disease (CHD) in babies. This advanced maternal age is linked to a higher likelihood of chromosomal abnormalities, which can impact the heart. Therefore, pregnant women in this age group should undergo comprehensive prenatal screening and genetic testing to evaluate the risk of CHD.
In summary:
- Maternal age over 40 is considered a risk factor for CHD in babies.
- Advanced maternal age increases the chance of chromosomal abnormalities affecting the heart.
- Pregnant women aged 40 and above should undergo comprehensive prenatal screening and genetic testing.
Quote: “Maternal age over 40 is an important factor in assessing the risk of congenital heart disease in babies.”
(Note: The bullet points and blockquote have been added to improve the readability and organization of the information.)
Certain Genetic Conditions
Several genetic conditions have been associated with an increased risk of congenital heart defects. Some examples include:
- Down syndrome
- Turner syndrome
- Marfan syndrome
- Holt-Oram syndrome
These genetic conditions can disrupt normal heart development, potentially resulting in structural abnormalities like stenosis.
Genetic counseling and testing are essential for families with a history of these disorders to assess the risk of CHD.
Family History Of Heart Defects
A family history of heart defects, particularly in first-degree relatives (parents, siblings), increases the risk of congenital heart disease (CHD) in offspring. Studies have found that individuals with an affected sibling or parent have an elevated risk of CHD compared to the general population.
To identify and manage the risk of CHD in their children, genetic counseling and prenatal screening are crucial for families with a history of heart defects.
- Key point: Family history of heart defects increases risk of CHD in offspring.
- Individuals with affected siblings or parents have elevated risk compared to general population.
- Genetic counseling and prenatal screening are important for managing risk.
Symptoms
Children with congenital heart disease, including stenosis, may exhibit various symptoms depending on the type and severity of the defect. Common symptoms include:
- Difficulty breathing
- Poor feeding
- Bluish tint to the skin or lips
These symptoms indicate inadequate oxygenation or blood flow, highlighting the need for prompt medical attention and evaluation.
Difficulty Breathing
Difficulty breathing is a common symptom of congenital heart disease, specifically stenosis. This condition is characterized by narrowed blood vessels or valves, which can obstruct blood flow and limit oxygen delivery to the body. As a result, children with congenital heart disease often experience struggles with breathing. It is important to note that rapid or labored breathing, especially during exertion, may indicate a potential heart problem. Therefore, it is crucial for parents or caregivers to seek evaluation from a healthcare professional if these symptoms are observed.
To summarize, the key points are:
- Difficulty breathing is a common symptom of congenital heart disease, particularly stenosis.
- Narrowed blood vessels or valves can impede blood flow and oxygen delivery.
- Children with congenital heart disease may experience rapid or labored breathing, especially during exertion.
- Seek evaluation from a healthcare professional if these symptoms are observed.
“Rapid or labored breathing, especially during exertion, may indicate a potential heart problem and should be evaluated by a healthcare professional.”
Poor Feeding
Infants with congenital heart defects, like stenosis, may experience difficulties with feeding. Insufficient blood flow and oxygenation can lead to fatigue and inadequate energy for feeding. Affected babies may have a weak suck, tire easily during feeds, or show signs of distress while feeding. Monitoring feeding patterns and consulting a pediatrician is critical to address these concerns promptly.
– Insufficient blood flow and oxygenation
– Fatigue and inadequate energy for feeding
– Weak suck
– Tiring easily during feeds
– Signs of distress while feeding
“Monitoring feeding patterns and consulting a pediatrician is critical to address these concerns promptly.”
Bluish Tint To Skin Or Lips
A bluish tint to the skin or lips, referred to medically as cyanosis, is a telltale sign of inadequate oxygenation. In children with congenital heart disease, cyanosis indicates compromised blood flow and oxygen supply to tissues. The tint may become more prominent during crying, feeding, or physical activity. It is important to seek medical attention if cyanosis is observed, as timely intervention can be life-saving.
Early Diagnosis And Treatment
Early diagnosis and treatment are vital for improving outcomes in children with congenital heart disease, including stenosis.
Prenatal screening, such as ultrasounds and fetal echocardiograms, can detect abnormalities before birth.
Postnatal assessments, including physical examinations and diagnostic tests, help identify specific defects and develop appropriate treatment plans.
Starting treatment early allows for better management of symptoms and prevents complications.
-
Prenatal screening methods:
- Ultrasounds
- Fetal echocardiograms
-
Postnatal assessments:
- Physical examinations
- Diagnostic tests
Early diagnosis and treatment play a crucial role in improving outcomes for children with congenital heart disease.
Treatment Options
The treatment of congenital heart disease, including stenosis, depends on the specific defect and its severity. Various treatment options are available to optimize heart function and improve outcomes in affected individuals. These include:
- Medication management
- Catheter-based procedures
- Surgeries.
It is crucial to tailor the treatment approach to the individual’s condition and needs, ensuring the best possible outcome.
Medications
Medications are often prescribed to manage symptoms and improve heart function in individuals with congenital heart disease. Depending on the specific defect, these medications can help regulate blood pressure, control heart rhythm abnormalities, and enhance cardiac output. It is important to note that close monitoring and regular follow-up visits are necessary to adjust dosages and ensure effectiveness of the prescribed medications.
Catheter Procedures
Catheter-based procedures, also known as interventional cardiology, are minimally invasive techniques used to treat certain congenital heart defects.
One common procedure for treating stenosis is balloon valvuloplasty. During this procedure, a catheter with a deflated balloon is guided to the narrowed valve. Once in place, the balloon is then inflated, effectively widening the valve and improving blood flow.
Compared to open-heart surgery, balloon valvuloplasty offers several advantages:
- Fewer risks: The minimally invasive nature of the procedure reduces the chances of complications.
- Shorter recovery time: As the procedure does not involve major incisions, patients typically experience a faster recovery.
In conclusion, catheter-based procedures, particularly balloon valvuloplasty, present a beneficial alternative to open-heart surgery for treating stenosis in congenital heart defects.
Surgery
More severe cases of congenital heart disease, including stenosis, may require surgical intervention. Open-heart surgery aims to correct the structural abnormality and restore normal blood flow. This may involve valve repair or replacement, reconstruction of the heart structures, or rerouting of blood vessels. Advancements in surgical techniques have significantly improved the success rates of these complex procedures.
Prognosis Improvement
Advancements in medical and surgical interventions have led to significant improvements in the prognosis of children with congenital heart disease, including stenosis. Early diagnosis, appropriate treatment, and a multidisciplinary approach involving pediatric cardiologists, surgeons, and other specialists have been instrumental in enhancing outcomes. With timely intervention, children with CHD can lead normal, healthy lives.
Normal, Healthy Lives
Children with congenital heart disease, including those with stenosis, can live normal and healthy lives with appropriate management. Regular follow-up care, medication adherence, and lifestyle modifications are essential components of long-term care. With proper attention to their heart health, these individuals can achieve developmental milestones, participate in physical activities, and thrive overall.
Long-Term Follow-Up Care
Congenital heart disease requires long-term follow-up care to monitor heart function, assess growth, and screen for potential complications. Regular visits to a pediatric cardiologist are crucial to ensure the ongoing health and well-being of individuals with CHD. Specific protocols and screenings may vary depending on the type and severity of the defect, but close medical supervision is pivotal to detect and address any emerging issues.
Potential Complications
Although advancements in diagnosis and treatment have significantly improved outcomes, individuals with congenital heart disease, including stenosis, may still face potential complications. These can include arrhythmias, heart failure, infective endocarditis, and developmental delays. Close monitoring, adherence to treatment plans, and ongoing medical support are essential to mitigate these risks and optimize quality of life.
💡
You may need to know these questions about congenital heart disease
What are 4 common congenital heart diseases?
Four common congenital heart diseases include atrial septal defect, ventricular septal defect, patent ductus arteriosus, and pulmonary stenosis. Atrial septal defect refers to a hole in the wall that separates the two upper chambers of the heart, while ventricular septal defect is a hole in the wall between the two lower chambers. Patent ductus arteriosus occurs when a blood vessel, called the ductus arteriosus, fails to close after birth, and pulmonary stenosis involves a narrowing of the pulmonary valve, which restricts blood flow from the heart to the lungs. These conditions can lead to various symptoms and complications, highlighting the importance of timely diagnosis and treatment.
What is the life expectancy of a congenital heart defect?
The life expectancy of individuals with a congenital heart defect (CHD) varies depending on its severity. For babies born with a non-critical CHD, approximately 95% are expected to survive to at least 18 years of age. On the other hand, babies born with critical CHDs have a lower survival rate, with approximately 69% expected to reach 18 years of age. However, it is important to note that these statistics provide a general understanding and individual outcomes may differ significantly based on various factors such as the specific type of CHD, access to medical care, and lifestyle choices.
What is the most common congenital heart disease?
The most common congenital heart disease is ventricular septal defect (VSD). This condition occurs when there is a hole in the wall separating the two lower chambers of the heart. The symptoms and impact of VSD vary depending on the size of the defect and the age of the patient. Small VSDs are often asymptomatic and can close on their own in early childhood, allowing individuals to have a normal life.
What is the main cause of congenital heart disease?
Congenital heart disease, a condition where abnormalities in the heart’s structure are present from birth, is primarily caused by genetic alterations or mutations. Researchers have found that changes in the baby’s genes, which can be inherited from the parents or occur during pregnancy, play a crucial role in the development of these heart defects. However, the exact cause of these gene changes is often unknown, leaving researchers with limited knowledge about the underlying factors causing the defects. Further studies are necessary to gain a comprehensive understanding of the specific genetic mechanisms involved in congenital heart disease development.
Reference source
https://www.cdc.gov/ncbddd/heartdefects/facts.html
https://www.nhlbi.nih.gov/health/congenital-heart-defects/types
https://www.cdc.gov/ncbddd/heartdefects/data.html
https://www.ncbi.nlm.nih.gov/books/NBK2212/