Contraceptive Methods: Empowering Women with Safe and Effective Protection
List:
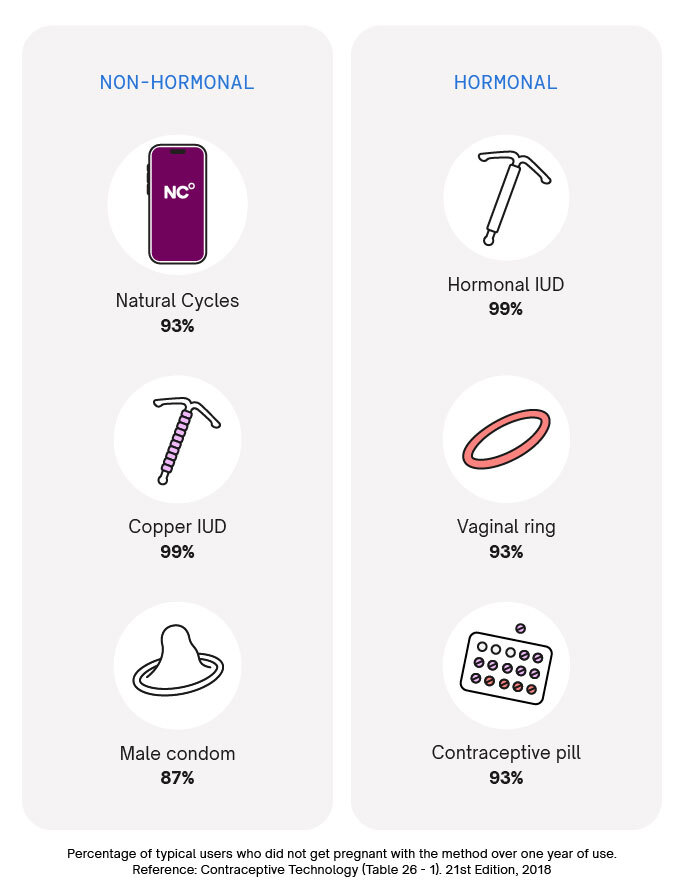
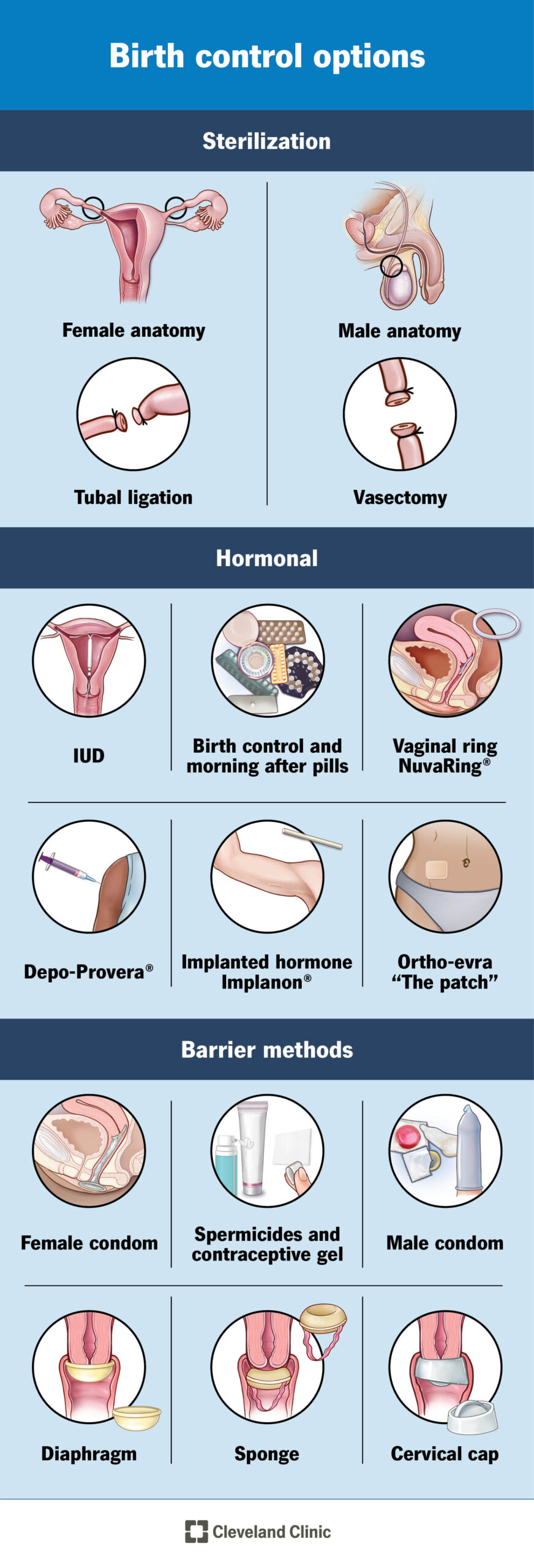
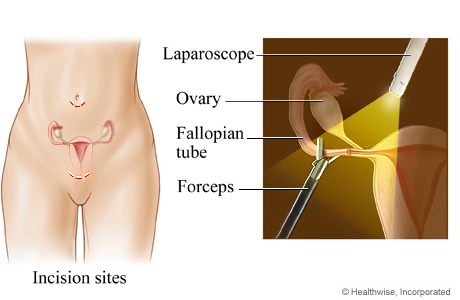
1. The article discusses two intrauterine devices (IUDs) used as contraceptive methods: the Levonorgestrel intrauterine system (LNG IUD) and the Copper T intrauterine device.
2. The LNG IUD is a small T-shaped device inserted into the uterus by a doctor.
3. It releases a small amount of progestin daily to prevent pregnancy.
4. The device can stay in the uterus for 3 to 8 years, depending on the specific device.
5. The typical use failure rate of the LNG IUD is between 0.1% and 0.4%.
6. The Copper T IUD is also shaped like a “T” and is placed inside the uterus by a doctor to prevent pregnancy.
7. It can be left in the uterus for up to 10 years.
8. The typical use failure rate of the Copper T IUD is 0.8%.
9. Family planning allows people to achieve their desired number of children and space out their pregnancies.
10. It involves the use of contraceptive methods and infertility treatment.
11. Access to contraceptive information and services is essential for the health and human rights of individuals.
12. Preventing unintended pregnancies helps lower maternal ill-health and pregnancy-related deaths.
13. Family planning benefits young girls by delaying pregnancies and reducing health risks associated with early childbearing.
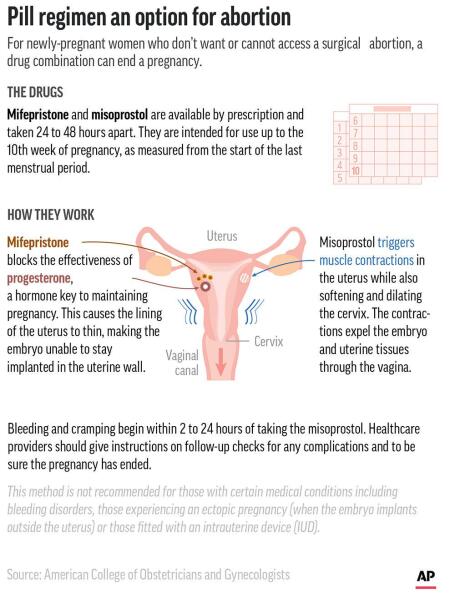
14. It also benefits older women by preventing pregnancies and reducing their increased health risks.
15. Contraception helps reduce the need for unsafe abortions and HIV transmission from mothers to newborns.
16. It can improve education for girls and create more opportunities for women in society.
17. In developing regions, an estimated 214 million women of reproductive age have an unmet need for contraception.