Contraceptive agents: Their Types, Usage, and Effectiveness
– Etonogestrel: long-acting synthetic progestin contraceptive used in rings and implants
– Desogestrel: synthetic progestin used in contraception with ethinyl estradiol
– Megestrol acetate: progestin used orally for anorexia, weight loss, and as anticancer agent
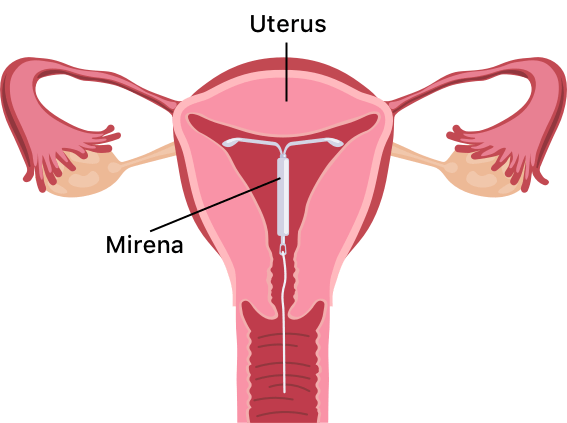
– Levonorgestrel: progestin found in oral and IUD contraceptives, emergency contraceptives
– Medroxyprogesterone acetate: progestin used in contraception, amenorrhea, endometriosis, cancer treatment
– Norethisterone: synthetic progestin used for contraception, hormone replacement therapy, endometriosis
– Ethynodiol diacetate: oral contraceptive to prevent pregnancy
– Mifepristone: cortisol receptor blocker used for Cushing’s syndrome and pregnancy termination
– Norgestimate: progesterone used as contraceptive and acne treatment
– Dienogest: oral progestin used for endometriosis treatment and contraception
– Norgestrienone: not annotated
– Estradiol cypionate: estradiol prodrug used for vasomotor symptoms and hypoestrogenisms
– Ormeloxifene: selective estrogen receptor modulator used as non-hormonal contraceptive
– Diethylstilbestrol: used in prostate cancer treatment and prevention of miscarriage
– Cyproterone acetate: used with ethinyl estradiol for severe acne and androgenization symptoms
– Drospirenone: progestin used in oral contraceptive pills
– Hydroxyprogesterone caproate: synthetic progestin to prevent preterm births in women with previous history
– Nomegestrol acetate: used in oral contraceptives, menopausal hormone therapy, treatment of gynecological disorders
– Quingestanol: no annotations or information provided
– Ethinylestradiol: used as a contraceptive
– Ulipristal: selective progesterone receptor modulator used for emergency contraception
– Estradiol valerate: prodrug used for menopause symptoms, hypoestrogenism, prostate cancer treatment, endometriosis, contraception
– Mestranol: synthetic estradiol used in oral contraceptive pills
– Demegestone: progesterone receptor agonist previously used for luteal insufficiency
– Segesterone acetate: hormonal contraceptive to prevent pregnancy
– Norethindrone enanthate: synthetic progestogen used for contraceptive therapy
– Algestone acetophenide: progestin used as an injectable contraceptive in combination with an estrogen
– Chlormadinone acetate: progestin used in combination with an estrogen for birth control
– Ifidancitinib: under investigation for the treatment of atopic dermatitis