Descensus uteri, the dreaded descent of the uterus, is a silent enemy that might be lurking within the depths of your body.
Hailing from an array of causes, from pregnancy to chronic constipation, this condition brings with it a host of unpleasant symptoms.
But fear not, for hope lies on the horizon, with treatments ranging from pelvic floor training to surgical miracles.
Join us on a journey into the realm of descensus uteri, where we unravel its mysteries and discover the path to victory.
descensus uteri
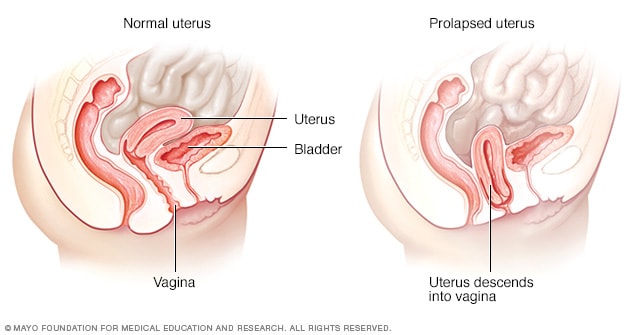
Descensus uteri, also known as uterine prolapse, is a condition characterized by the descent or sagging of the uterus into the vaginal canal.
This occurs due to various factors such as connective tissue weakness, muscle weakness, and ligament weakness.
Other contributing factors include pregnancy, physical exertion, excessive weight, chronic constipation, chronic bronchitis, bladder issues, and digestive difficulties.
Symptoms of descensus uteri can manifest as a pressure sensation, vaginal pain, increased urination, urinary incontinence, increased urge to defecate, and infection.
Ulcers, bladder prolapse, and rectal prolapse can also occur.
Treatment options typically include gynecological examination, ultrasound, pelvic floor training, surgical intervention, postnatal exercises, and prevention measures.
Key Points:
- Descensus uteri is the descent or sagging of the uterus into the vaginal canal.
- Contributing factors include:
- Connective tissue weakness
- Muscle weakness
- Ligament weakness
- Other factors that can contribute to uterine prolapse include:
- Pregnancy
- Physical exertion
- Excessive weight
- Chronic constipation
- Chronic bronchitis
- Bladder issues
- Digestive difficulties
- Symptoms can include:
- Pressure sensation
- Vaginal pain
- Increased urination
- Urinary incontinence
- Increased urge to defecate
- Infection
- Ulcers, bladder prolapse, and rectal prolapse are potential complications.
- Treatment options include:
- Gynecological examination
- Ultrasound
- Pelvic floor training
- Surgical intervention
- Postnatal exercises
- Prevention measures.
descensus uteri – Watch Video
💡
Pro Tips:
1. The descensus uteri refers to the downward displacement of the uterus within the pelvic cavity, a condition that can occur due to factors such as age, childbirth, or chronic straining.
2. The ancient Egyptians believed that the weight of the uterus was responsible for women’s intellectual inferiority.
3. Around the 19th century, a condition called “hysterical suffocation” was often misdiagnosed as a descensus uteri. It was believed that the uterus was moving upwards and causing symptoms such as difficulty breathing and anxiety.
4. The Greek physician Galen proposed a controversial theory that the uterus was a roaming “wandering womb” that could cause various ailments by moving around the body.
5. During the Renaissance, physicians used various methods to treat descensus uteri, including using pessaries made of substances like wood, cork, or silver to support and lift the uterus back into place.
Connective Tissue Weakness
Connective tissue weakness is a significant factor in the development of descensus uteri or uterine prolapse. The connective tissues surrounding the uterus, such as ligaments and pelvic floor muscles, play a crucial role in supporting and maintaining the position of the uterus. However, when these tissues become weakened or damaged, the uterus can descend into the vaginal canal.
Several factors can contribute to connective tissue weakness, including genetics, hormonal changes, and aging. Genetics can predispose individuals to have weaker connective tissues, making them more susceptible to uterine prolapse. Hormonal changes during menopause can also lead to the degradation of connective tissues, further increasing the risk. Additionally, the natural process of aging can gradually weaken these tissues over time.
Muscle Weakness
Muscle weakness in the pelvic floor is a common cause of descensus uteri. The pelvic floor muscles provide support to the uterus, bladder, and bowel. If these muscles are weakened or lax, the uterus may sag or prolapse. This weakening can occur due to various factors, including childbirth, aging, obesity, and repetitive heavy lifting.
Childbirth can significantly impact the strength of the pelvic floor muscles. The stretching and tearing of these muscles during delivery can lead to their weakening. Moreover, repeated pregnancies can further exacerbate muscle weakness. Aging and hormonal changes also contribute to muscle degradation, making the uterus more susceptible to prolapse. Additionally, obesity and repetitive heavy lifting put excessive strain on the pelvic floor muscles, leading to their dysfunction.
Ligament Weakness
Ligament weakness is a crucial factor linked to the development of descensus uteri, where the uterus descends into the vaginal canal. It is primarily the uterosacral and cardinal ligaments that provide support and maintain the uterus in its proper position. However, pregnancy and childbirth play a significant role in weakening these ligaments.
During pregnancy, the ligaments that support the uterus naturally become lax to accommodate the growth of the fetus. This stretching can cause long-lasting damage and weaken the ligaments. Furthermore, multiple pregnancies further increase the chances of experiencing ligament weakness.
Pregnancy
Pregnancy is a well-known factor in the development of descensus uteri. The weight of the growing fetus puts pressure on the pelvic organs, including the uterus. This increased pressure, combined with the hormonal changes and stretching of ligaments, can weaken the supporting structures and contribute to uterine prolapse.
Furthermore, vaginal childbirth can result in pelvic floor muscle and connective tissue damage. The strain and stretching caused during delivery can lead to weakened pelvic floor muscles and ligaments, further increasing the risk of uterine prolapse.
- Pregnancy contributes to descensus uteri
- Growing fetus weight puts pressure on pelvic organs
- Hormonal changes and ligament stretching weaken supporting structures
- Vaginal childbirth can damage pelvic floor muscles and connective tissue
- Weakened muscles and ligaments increase the risk of uterine prolapse.
Physical Exertion
Engaging in excessive physical exertion, particularly activities that involve repetitive heavy lifting or straining, can increase the risk of descensus uteri. Constantly subjecting the pelvic area to intense physical strain can weaken the pelvic floor muscles, ligaments, and other supporting structures, making the uterus more prone to prolapse.
Jobs or activities that require heavy lifting, such as those in the construction or agriculture industries, can significantly contribute to the development of uterine prolapse. Additionally, individuals who regularly participate in high-impact activities, such as weightlifting or gymnastics, may also experience weakened pelvic floor muscles, increasing the risk of prolapse.
- Excessive physical exertion can increase the risk of descensus uteri
- Heavy lifting and straining put strain on the pelvic area
- Weakens pelvic floor muscles, ligaments, and supporting structures
- Jobs in construction or agriculture industries increase risk of uterine prolapse
- Regular participation in high-impact activities can also contribute to prolapse.
Excessive Weight
Carrying excess weight puts additional strain on the pelvic floor muscles and supporting ligaments, increasing the risk of descensus uteri. Obesity can weaken these structures and make them less able to support the uterus properly. Moreover, excess abdominal fat can push down on the pelvic organs, contributing to the prolapse of the uterus.
Additionally, obesity is often associated with other risk factors for uterine prolapse, such as chronic constipation and chronic bronchitis. Addressing weight-related issues through weight loss and appropriate lifestyle changes can help reduce the risk of uterine prolapse.
- Excess weight strains the pelvic floor muscles and supporting ligaments
- Obesity weakens the structures that support the uterus
- Excess abdominal fat contributes to uterine prolapse
- Obesity is linked to chronic constipation and bronchitis
- Weight loss and lifestyle changes can decrease the risk of uterine prolapse.
Chronic Constipation
Chronic constipation can have negative effects on the pelvic floor muscles and contribute to uterine prolapse. Increased intra-abdominal pressure caused by constipation weakens these muscles over time. Straining during bowel movements can also put stress on the uterus and contribute to prolapse.
Moreover, chronic constipation leads to repeated straining, which weakens the supporting ligaments and connective tissues. To reduce the risk of uterine prolapse, it’s important to address digestive issues promptly. This can be done through maintaining a healthy diet, ensuring adequate fluid intake, and regularly engaging in exercise.
Chronic Bronchitis
Chronic bronchitis is a respiratory condition that involves persistent coughing and inflammation of the bronchial tubes. This condition can indirectly contribute to uterine prolapse. The chronic cough associated with bronchitis can increase intra-abdominal pressure, which in turn weakens the pelvic floor muscles and ligaments.
The constant strain from coughing puts excessive pressure on the pelvic organs, potentially resulting in descensus uteri. It is crucial for individuals with chronic bronchitis to effectively manage their condition in order to reduce the risk of uterine prolapse.
- Chronic bronchitis is a respiratory condition characterized by persistent coughing and inflammation of the bronchial tubes.
- The chronic cough associated with bronchitis can lead to increased intra-abdominal pressure.
- This increased pressure weakens the pelvic floor muscles and ligaments.
- The strain from coughing can put excessive pressure on the pelvic organs, potentially leading to uterine prolapse.
It is essential for individuals with chronic bronchitis to manage their condition effectively to minimize the risk of uterine prolapse.
Bladder Issues
Bladder issues, including frequent urinary tract infections (UTIs) and bladder prolapse, are closely linked to descensus uteri.
UTIs can cause discomfort and urgency, leading to increased urination and straining. This, in turn, weakens the pelvic floor muscles and supporting ligaments.
Bladder prolapse, also known as cystocele, occurs when the bladder drops into the vagina due to weakened pelvic floor muscles. This condition often coexists with uterine prolapse and shares similar risk factors, such as connective tissue weakness, muscle weakness, physical exertion, and pregnancy.
Digestive Difficulties
Digestive difficulties, including chronic constipation, can contribute to descensus uteri. Chronic digestive issues can cause excessive straining during bowel movements, which weakens the pelvic floor muscles and supporting ligaments. Similarly, chronic digestive conditions like ulcers can lead to increased intra-abdominal pressure, weakening the pelvic structures.
Furthermore, rectal prolapse, a condition where the rectum protrudes from the anus, is often associated with uterine prolapse. Chronic constipation and continual straining during bowel movements can increase the risk of both rectal and uterine prolapse.
Descensus uteri or uterine prolapse is a condition characterized by the descent of the uterus into the vaginal canal. Connective tissue weakness, muscle weakness, and ligament weakness are major contributors to this condition. Factors such as pregnancy, physical exertion, excessive weight, chronic constipation, chronic bronchitis, bladder issues, and digestive difficulties can increase the risk of uterine prolapse. It is crucial to identify and address these risk factors promptly.
Gynecological examinations, ultrasounds, pelvic floor training, and surgical treatments are available for managing uterine prolapse. Additionally, postnatal exercises and preventive measures, such as maintaining a healthy weight and addressing constipation, can help minimize the likelihood of uterine prolapse.
💡
You may need to know these questions about descensus uteri
What is Descensus uteri?
Descensus uteri, also known as a uterine prolapse, is a condition characterized by the descent of the uterus towards the vagina. In severe cases, the uterus may become visible at the vaginal opening. This condition can lead to the weakening of the bladder and result in urinary incontinence. The prolapse of the uterus poses significant discomfort and may require medical intervention to alleviate the symptoms and improve the quality of life for affected individuals.
What is a uterine displacement?
Uterine displacement, also known as a prolapsed uterus, refers to the condition where the uterus descends from its normal position and protrudes out of the vagina. This occurs when the pelvic floor muscles and ligaments become weak, losing their ability to adequately support the uterus. Consequently, the uterus slips downward, resulting in its displacement and causing various discomfort and complications.
What are the grades of Descensus Uteri?
Descending Uterus (Descensus Uteri) is classified into four grades based on the extent of prolapse. Grade 0 indicates no prolapse, while grade 1 represents a prolapse that is halfway to the hymen. Advancing to grade 2, the prolapse reaches the hymen, and with grade 3, it extends halfway past the hymen. Lastly, grade 4 signifies the maximum extent of descent.
What are the four types of uteri?
In the realm of mammalian reproductive anatomy, there exist four distinct types of uteri: duplex, bipartite, bicornuate, and simplex. The duplex uterus, characterized by having two entirely separate uteri, each equipped with its own fallopian tube, presents a unique structure. Meanwhile, the bipartite uterus also features two separate compartments, though they share a common cervix. Another variant, the bicornuate uterus, is characterized by its Y-shaped structure, with two partially fused uterine horns. Lastly, the simplex uterus stands as a singular structure, lacking any division or fusion, offering a more straightforward design. These various uterine forms present fascinating adaptations throughout the mammalian world.
Reference source
https://www.hirslanden.com/en/international/disease-patterns/descensus-uteri.html
https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/symptoms-causes/syc-20353458
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prolapsed-uterus
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056425/