In a world where the battle against cancer rages on, there is one type that silently dominates the shadows: the endometrioid tumor.
Nestled within the depths of the uterus, this formidable adversary wears many faces and carries countless mysteries.
Embark on a journey with us as we unveil the enigmatic nature of endometrioid cancer and explore the unknown territories that lie behind its insidious veil.
endometrioid tumour
An endometrioid tumor is a type of cancer that originates in the inner lining of the uterus, known as the endometrium.
It is the most common type of cancer in the uterus and is characterized by the growth of gland cells that resemble the normal uterine lining.
Some endometrioid cancers may also contain squamous cells.
The grade of an endometrial cancer is determined by the organization of the cancer cells into gland-like structures, with Grade 1 tumors having over 95% gland formation, Grade 2 tumors having between 50% and 94% gland formation, and Grade 3 tumors having less than half gland formation and being more aggressive.
Endometrioid cancers are generally classified into two types – Type 1, which is typically not aggressive and caused by excess estrogen, and Type 2, which is more likely to spread outside the uterus and is not caused by estrogen excess.
Risk factors for endometrial cancer include changes in hormone balance, certain diseases or conditions, menstruation and pregnancy history, age, obesity, hormone therapy for breast cancer, and Lynch syndrome, a genetic syndrome associated with an increased risk of various cancers.
Early detection of endometrial cancer is crucial for successful treatment, usually involving surgical removal of the uterus.
Key Points:
- Endometrioid tumors originate in the inner lining of the uterus called the endometrium.
- It is the most common type of cancer in the uterus and is characterized by the growth of gland cells resembling the normal uterine lining.
- Some endometrioid cancers may also contain squamous cells.
- The grade of the cancer is determined by the organization of the cancer cells into gland-like structures, with Grade 1 and Grade 2 tumors having a higher percentage of gland formation than Grade 3 tumors.
- Endometrioid cancers are classified into Type 1 and Type 2, with Type 1 being less aggressive and caused by excess estrogen, while Type 2 is more likely to spread outside the uterus and not caused by estrogen excess.
- Risk factors for endometrial cancer include hormone imbalances, certain diseases or conditions, menstruation and pregnancy history, age, obesity, hormone therapy for breast cancer, and Lynch syndrome.
- Early detection is crucial for successful treatment, typically involving surgical removal of the uterus.
endometrioid tumour – Watch Video
💡
Pro Tips:
1. The term “endometrioid” in endometrioid tumour refers to the resemblance of the tumour cells to the endometrium, the inner lining of the uterus.
2. Endometrioid tumours are most commonly found in the ovaries and endometrium, but can also occur in other organs such as the testes, colon, and kidneys.
3. The presence of endometrioid tumours can lead to symptoms such as pelvic pain, abnormal menstrual bleeding, and infertility in some cases.
4. Endometrioid tumours are often associated with endometriosis, a condition where the endometrial tissue grows outside the uterus.
5. Research has shown that endometrioid tumours, particularly those found in the ovaries, have a higher chance of being malignant compared to other subtypes of ovarian tumours.
1. Introduction To Endometrioid Cancer
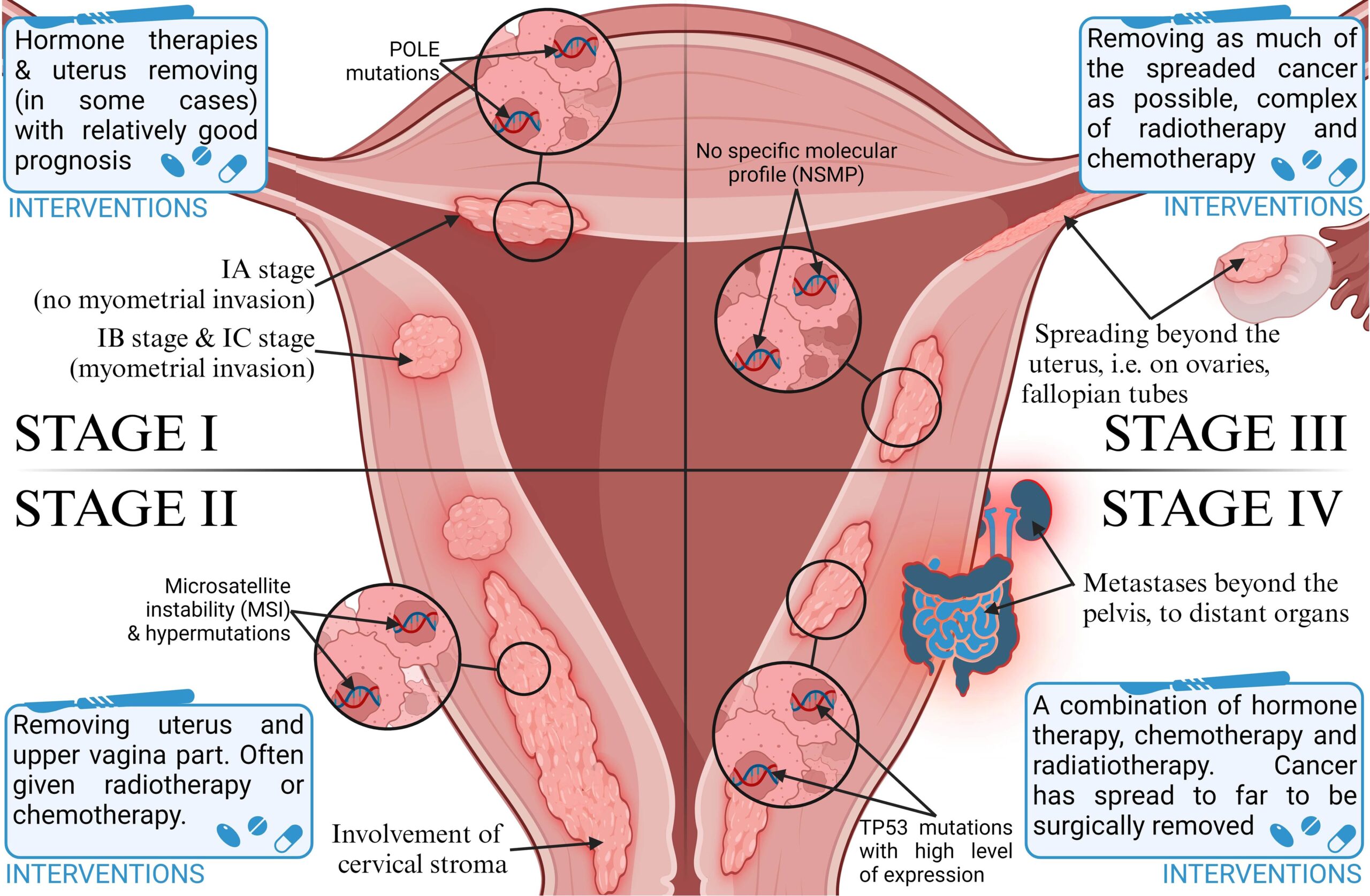
Endometrioid cancer is the most common type of cancer in the uterus, originating in the inner lining, called the endometrium. This type of cancer develops from gland cells within the endometrium and closely resembles the normal uterine lining. It’s important to note that there are several subtypes and types of endometrial cancers, including adenocarcinoma (the most prevalent), uterine carcinosarcoma, squamous cell carcinoma, small cell carcinoma, transitional carcinoma, serous carcinoma, clear-cell carcinoma, mucinous adenocarcinoma, undifferentiated carcinoma, dedifferentiated carcinoma, and serous adenocarcinoma.
2. Types Of Endometrial Cancers
Endometrial cancers can be categorized into two primary types: type 1 and type 2.
Type 1 endometrial cancers are usually less aggressive and are associated with an excess of estrogen. These cancers commonly develop from atypical hyperplasia, a condition characterized by the overgrowth of cells in the endometrium.
In contrast, type 2 endometrial cancers are more likely to grow and spread beyond the uterus, displaying a poorer prognosis. Unlike type 1 cancers, type 2 endometrial cancers are not caused by elevated estrogen levels. They encompass various subtypes such as papillary serous carcinoma, clear-cell carcinoma, undifferentiated carcinoma, and grade 3 endometrioid carcinoma.
3. Characteristics Of Endometrioid Cancer
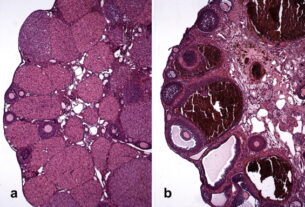
Endometrioid tumors are composed mainly of glandular cells and can also contain squamous cells. The grade of an endometrial cancer is determined by the organization of the cancer cells into gland-like structures.
- Grade 1 tumors have 95% or more of the cancer tissue forming glands.
- Grade 2 tumors have between 50% and 94% glandular formation.
- Grade 3 tumors exhibit less than half of the cancer tissue forming glands.
Grade 3 tumors are typically more aggressive and have a poorer prognosis.
“The grade of endometrial cancers is based on the amount of glandular formation, with grade 1 having the highest glandular component and grade 3 having the least.”
4. Sub-Types Of Endometrioid Cancers
There are various subtypes of endometrial cancer that further define the disease. These subtypes include:
- Adenocarcinoma (with squamous differentiation)
- Adenoacanthoma
- Adenosquamous (or mixed cell)
- Secretory carcinoma
- Ciliated carcinoma
- Villoglandular adenocarcinoma
Each subtype has its own unique characteristics, but they all fall under the umbrella of endometrial cancer.
5. Grading System For Endometrial Cancer
The grade of an endometrial cancer is a crucial factor in determining its aggressiveness and prognosis. The classification system for endometrial cancer is based on the percentage of glandular formation within the cancer tissue. Grade 1 tumors, which have a high proportion of glands, generally have a more favorable outlook. Conversely, grade 3 tumors, where less than half of the cancer tissue forms glands, tend to exhibit aggressive behavior and have poorer outcomes.
6. Differences Between Type 1 And Type 2 Endometrial Cancers
Type 1 and type 2 endometrial cancers differ in behavior and underlying causes:
- Type 1 cancers are predominantly associated with excessive estrogen exposure and commonly arise from atypical hyperplasia.
- Type 2 cancers are not influenced by estrogen levels and are more likely to exhibit aggressive growth and metastasis.
- Type 2 cancers include subtypes such as papillary serous carcinoma, clear-cell carcinoma, undifferentiated carcinoma, and grade 3 endometrioid carcinoma.
7. Uterine Carcinosarcoma And Its Relation To Endometrioid Cancer
Uterine Carcinosarcoma (CS): A Brief Overview
Uterine carcinosarcoma (CS), also referred to as malignant mixed mullerian tumor, is a distinctive form of cancer that incorporates elements of both endometrial carcinoma and sarcoma. Considered as a type 2 endometrial carcinoma, this malignancy arises in the endometrium, requiring specialized diagnostic and treatment strategies owing to its complex nature.
Key points:
- Uterine carcinosarcoma combines features of endometrial carcinoma and sarcoma.
- It is classified as a type 2 endometrial carcinoma and originates in the endometrium.
- Due to its complexity, specialized diagnostic and treatment approaches are essential.
“Uterine carcinosarcoma presents a unique challenge due to its mixed nature and requires careful attention during diagnosis and treatment.”
8. Uterine Sarcomas And Their Connection To Endometrial Cancer
In addition to endometrial carcinomas, there are also uterine sarcomas, which arise in the muscle layer or supporting connective tissue of the uterus. Uterine sarcomas are distinct from endometrial carcinomas and represent a separate group of malignancies. Unlike endometrial cancers, uterine sarcomas are rare and often present unique challenges in diagnosis and treatment.
- Uterine sarcomas arise in the muscle layer or supporting connective tissue of the uterus.
- They are distinct from endometrial carcinomas.
- Uterine sarcomas are a separate group of malignancies.
- They are rare compared to endometrial carcinomas.
- Diagnosis and treatment of uterine sarcomas pose unique challenges.
“Unlike endometrial cancers, uterine sarcomas are rare and often present unique challenges in diagnosis and treatment.”
9. Symptoms And Causes Of Endometrial Cancer
Recognizing the signs and symptoms of endometrial cancer is vital for early detection and successful treatment. Symptoms of this disease may include vaginal bleeding after menopause, bleeding between periods, and pelvic pain. The exact cause of endometrial cancer remains unknown, but changes in the DNA of cells in the endometrium are believed to lead to the growth of cancer cells.
10. Risk Factors For Endometrial Cancer
Identifying risk factors for endometrial cancer can help individuals take steps towards preventive measures and early detection. Risk factors include alterations in hormone balance, certain diseases or conditions, menstruation history, pregnancy history, age, obesity, hormone therapy for breast cancer, and Lynch syndrome. Notably, obesity and hormone therapy are prominent risk factors for endometrial cancer. Lynch syndrome, a genetic syndrome associated with an increased risk of several types of cancer, also elevates the risk of endometrial cancer. Individuals with Lynch syndrome are encouraged to seek appropriate cancer screenings and genetic counseling for a thorough understanding of their personal risk profile.
Understanding the types, characteristics, grading systems, and unique subtypes of endometrial cancers is crucial for appropriate diagnosis and treatment strategies. Additionally, recognizing the symptoms, causes, and risk factors associated with endometrial cancer facilitates early detection and improves patient outcomes. By shedding light on the complexities and nuances of endometrioid tumor progression, this article aims to contribute to the advancement of healthcare practices and heightened awareness surrounding this prevalent cancer.
💡
You may need to know these questions about endometrioid tumour
What is an endometrioid tumor?
An endometrioid tumor is a type of tumor that typically develops in the endometrium, the inner lining of the uterus. It is the most frequently observed form of endometrial carcinoma. This tumor’s microscopic characteristics resemble the proliferative endometrium, displaying varying levels of glandular complexity and cellular pleomorphism. Due to its resemblance to normal endometrial tissue, proper diagnosis and classification of this tumor are important for appropriate treatment and management strategies.
Is endometrioid cancer the same as endometrial cancer?
Endometrioid cancer is a type of endometrial cancer, but not all endometrial cancers are endometrioid. While the majority of endometrial cancers are adenocarcinomas, which originate from gland cells, endometrioid cancer specifically resembles the normal uterine lining. This distinction highlights that endometrioid cancer is a subtype within the broader category of endometrial cancer, reflecting its close resemblance to the endometrium.
Is endometrioid cancer curable?
Yes, endometrioid cancer can be curable in many cases. Early diagnosis plays a crucial role in the successful treatment of endometrioid cancer. With timely detection, treatment options such as surgery, radiation therapy, and chemotherapy can be highly effective in eliminating or controlling cancerous cells. Therefore, patients diagnosed with endometrioid cancer in its early stages have a high chance of being cured and returning to normal health. However, it is essential for individuals to be aware of the signs and symptoms and promptly consult a healthcare professional to ensure early detection and increase the likelihood of a positive outcome.
Is endometrioid carcinoma aggressive?
Endometrioid carcinoma, specifically type 1, is generally considered less aggressive compared to type 2 endometrial cancers. Type 1 endometrioid carcinomas tend to have a slower rate of spreading to other tissues. As a result, they often do not require as aggressive treatment as their type 2 counterparts. However, it is important to note that each case should be evaluated individually, and treatment decisions should be made in consultation with healthcare professionals based on specific characteristics of the tumor and the patient’s overall health.
Reference source
https://pubmed.ncbi.nlm.nih.gov/21309258/
https://www.cancer.org/cancer/types/endometrial-cancer/about/what-is-endometrial-cancer.html
https://www.cancer.gov/types/uterine/patient/endometrial-treatment-pdq
https://my.clevelandclinic.org/health/diseases/16409-uterine-cancer