In the mysterious realm of the womb, where life takes shape in a world unseen, a remarkable phenomenon unfolds: fetal breath movement.
Like a delicate dance of invisible whispers, these tiny movements of the unborn strengthen the very muscles that will sustain life outside the womb.
Join us as we unravel the enigma of fetal breath movement and discover the awe-inspiring journey of a baby’s first breath.
fetal breath movement
Fetal breath movement refers to the breathing-like movements that babies practice in the womb.
These movements play a role in strengthening the breathing muscles and supporting the development of air sacs in the lungs.
While fetal breath movement starts around week 10 of pregnancy, it becomes more frequent after week 20.
It is important to note that these movements are not necessary for the baby’s survival and may not occur constantly.
Oxygen and carbon dioxide exchange in the womb happens through the umbilical cord and placenta.
The baby takes their first breath after birth when they respond to the change in environment.
The lungs of babies are fully developed by week 28 of pregnancy, allowing premature babies to breathe on their own.
However, lung and circulatory system maturation continues until at least 8 years of age.
Key Points:
- Fetal breath movement helps babies develop their breathing muscles and air sacs in the lungs.
- These movements become more frequent after week 20 of pregnancy.
- Fetal breath movement is not necessary for the baby’s survival and may not occur constantly.
- Oxygen and carbon dioxide exchange in the womb occurs through the umbilical cord and placenta.
- Babies take their first breath after birth in response to the change in environment.
- Lungs are fully developed by week 28 of pregnancy, allowing premature babies to breathe on their own. However, lung and circulatory system maturation continues until at least 8 years of age.
fetal breath movement – Watch Video
💡
Pro Tips:
1. Fetal breath movement, also known as “practice breathing,” is a reflex action that prepares the baby’s lungs for breathing after birth.
2. Fetal breath movement can be observed on ultrasounds as early as 16 to 18 weeks gestation, indicating the development of the respiratory system.
3. The purpose of fetal breath movement is not to obtain oxygen, but to exercise the respiratory muscles and enhance lung development.
4. Fetal breath movement is considered a positive sign of a healthy developing fetus, as its absence can be a potential indicator of certain health complications.
5. The frequency of fetal breath movement usually decreases in the later stages of pregnancy, as the baby’s lungs become more mature and capable of functioning independently at birth.
Understanding Fetal Breath Movement: What You Need To Know
During pregnancy, it is a common misconception that babies breathe in the same way as adults. However, the truth is that babies don’t breathe in the womb in the traditional sense, as they don’t have access to air. Instead, they engage in a series of practice breathing movements called fetal breath movements. These movements serve a crucial purpose in developing the baby’s respiratory system.
The Development Of Fetal Breathing Movements
Fetal breathing movements, also known as respiratory movements, begin around week 10 of pregnancy. The baby starts to perform gentle inhaling and exhaling motions with their diaphragm and chest muscles. These movements help exercise and strengthen the muscles involved in breathing, such as the diaphragm and intercostal muscles. They also play a significant role in the development of air sacs in the lungs, known as alveoli.
- Fetal breathing movements start around week 10 of pregnancy.
- The baby inhales and exhales using their diaphragm and chest muscles.
- These movements exercise and strengthen breathing muscles.
- They contribute to the development of air sacs in the lungs.
“Fetal breathing movements aid in the development of breathing muscles and air sacs in the lungs.”
Importance Of Fetal Breathing Movements For Lung Development
Fetal breathing movements serve an essential developmental purpose, preparing the baby’s respiratory muscles for the transition from the womb to the outside world where breathing is required. These movements also contribute to the development of the baby’s lungs by stretching and strengthening the alveoli – tiny air sacs responsible for oxygen and carbon dioxide exchange. Strengthening these air sacs through fetal breathing movements supports their ability to function properly after birth.
Timing Of Fetal Breathing Movements In Pregnancy
Fetal breathing movements usually start around week 10 of pregnancy, but they become more frequent and noticeable after week 20. As the baby grows and develops, these movements become a regular occurrence. However, the frequency and intensity of fetal breathing movements can vary throughout the pregnancy.
It is important to note that the baby does not need constant practice of fetal breathing movements for healthy lung development. The primary source of oxygen during pregnancy is the mother’s blood, which is delivered to the baby through the placenta and umbilical cord.
The Role Of Oxygen And Carbon Dioxide Exchange In The Womb
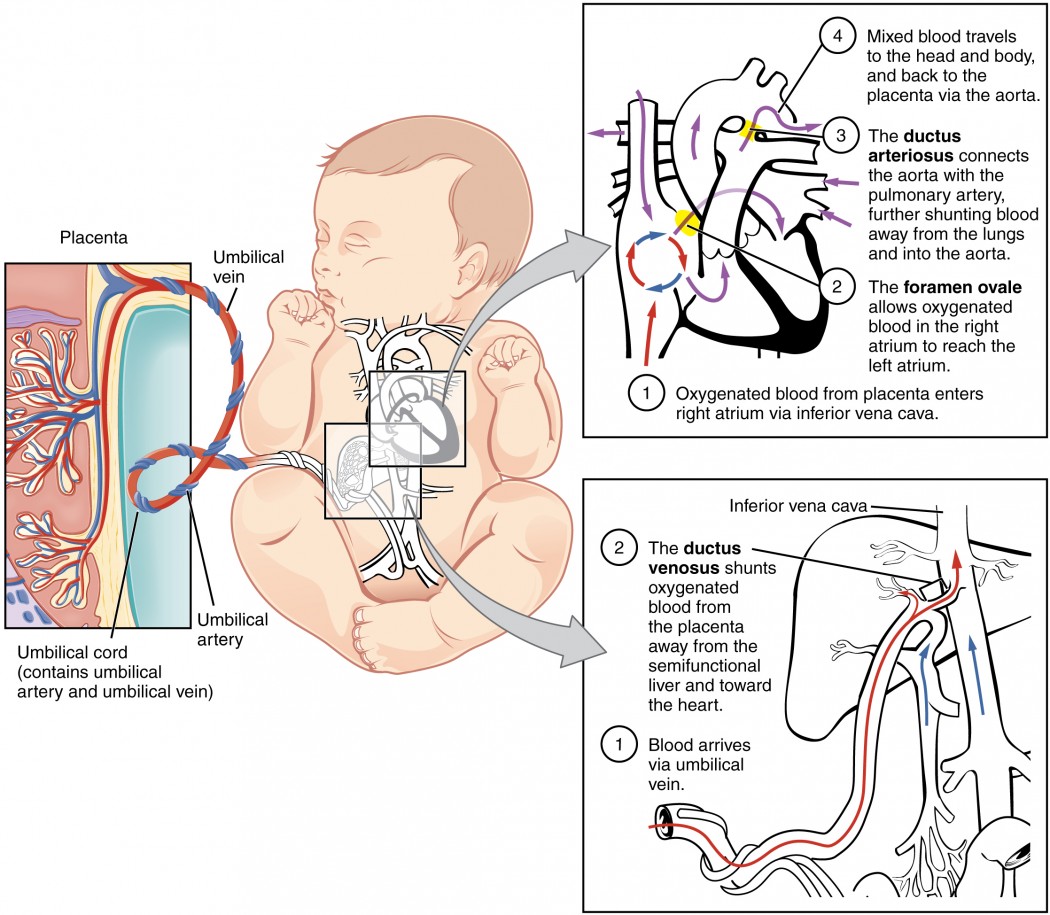
While in the womb, the baby’s oxygen and carbon dioxide exchange occurs through the umbilical cord and placenta. The mother’s blood carries oxygen and nutrients through the placenta, which are then transferred to the baby’s blood. In return, the baby’s blood releases carbon dioxide, which is carried back to the mother’s blood for elimination.
This unique process eliminates the need for the baby to independently breathe air while in the womb. The fetal breathing movements serve as important exercises for future breathing functions rather than serving an immediate respiratory purpose within the womb.
- The baby’s oxygen and carbon dioxide exchange occurs through the umbilical cord and placenta
- The mother’s blood carries oxygen and nutrients through the placenta
- The baby’s blood releases carbon dioxide, which is carried back to the mother’s blood for elimination
“The fetal breathing movements serve as important exercises for future breathing functions rather than serving an immediate respiratory purpose within the womb.”
First Breath: Transition From Womb To World
After birth, the baby undergoes a significant transition from the protected environment of the womb to the outside world. Within approximately 10 seconds of delivery, the baby takes its first breath in response to the change in environment. This moment signifies the initiation of fully independent respiratory function as the baby’s lungs begin to expand and inhale air into their respiratory system for the first time.
The first breath marks the baby’s transition from relying on the umbilical cord and placenta for oxygen supply to breathing air directly into their lungs. This transition is facilitated by several factors:
- Expansion of the chest cavity: As the baby takes its first breath, the chest cavity expands, allowing for increased lung capacity.
- Increased lung capacity: The baby’s lungs develop throughout pregnancy but only fully expand when they inhale air at birth.
- Other factors: Various physiological changes enable the transition to independent breathing, such as the closure of the ductus arteriosus and foramen ovale.
In conclusion, the baby’s first breath is a momentous occasion that signifies the beginning of independent respiratory function. As the baby inhales air into their lungs, they no longer rely on the umbilical cord and placenta for oxygen supply, and instead, they initiate the lifelong process of breathing.
“Remember, the first breath is the start of their journey towards self-sustained life.“
Lung Development Milestones: From Preterm To Full Maturation
By week 28 of pregnancy, premature babies are able to breathe on their own as their lungs have developed enough. However, it is important to remember that the circulatory system and lung maturation continue to progress until full-term birth and beyond.
By week 37 of pregnancy, the baby’s lungs have developed more fully and they continue to grow and fine-tune until at least 8 years of age. An important milestone occurs around month 6 of pregnancy when the lungs start producing a substance called surfactant. Surfactant is crucial because it enables the air sacs in the lungs to inflate and deflate properly.
In situations where a baby is born extremely premature, they may receive artificial surfactant in addition to breathing assistance from a ventilator, CPAP machine, or small breathing tubes. Babies born before week 36 and most born before week 32 may require breathing support due to their lung immaturity.
Supporting Baby’s Lung Development: Factors To Consider
Maintaining a healthy pregnancy is essential for the proper development of a baby’s lungs. Factors such as quitting smoking, following a nutritious diet, avoiding smoke after birth, and encouraging regular exercise can significantly support a baby’s lung development.
Quitting smoking is particularly crucial, as exposure to tobacco smoke during pregnancy can impair lung development and increase the risk of respiratory problems in the baby. Additionally, providing a smoke-free environment after birth further protects the baby’s developing lungs.
A well-balanced diet rich in essential nutrients, vitamins, and minerals supports overall fetal development, including the lungs. Regular exercise during pregnancy also contributes to a healthy circulation, ensuring that the baby receives an adequate oxygen supply throughout gestation.
- Quit smoking
- Follow a nutritious diet
- Avoid smoke after birth
- Encourage regular exercise
“Maintaining a healthy pregnancy is essential for the proper development of a baby’s lungs.”
Delivery And The Impact On Baby’s Breathing
During delivery, the baby’s breathing is impacted by the contractions that squeeze the baby and force the amniotic fluid out of the lungs. This process is essential as it helps clear the airways and prepares the lungs for the first breaths. The strong squeezing action during delivery assists in expelling any residual fluid or mucus in the respiratory system, making it easier for the baby to breathe independently.
It is worth noting that as long as the baby is attached to the mother through the placenta and umbilical cord, it is not necessary for them to breathe. The baby’s oxygen and nutrient supply are maintained through the umbilical cord until it is clamped and cut after birth.
- Delivery impacts baby’s breathing
- Process clears airways and prepares lungs
- Strong squeezing action helps expel fluid and mucus
- Baby doesn’t need to breathe as long as attached to mother
- Oxygen and nutrient supply maintained through umbilical cord
Postnatal Lung Development: Growing And Fine-Tuning
After birth, the baby’s respiratory system continues to grow and mature. One crucial aspect of this development is the expansion of alveoli, the small air sacs in the lungs responsible for facilitating oxygen exchange. Most newborns are born with approximately 20 to 50 million alveoli, which gradually increase to around 300 million by the age of eight.
As the baby grows, the ribs that surround the critical organs become tougher, helping to protect the lungs and ensure their proper function. The continuous growth and fine-tuning of the lungs contribute to the baby’s overall respiratory health during childhood and beyond.
It is essential to monitor the baby’s respiratory function during the early years and consult with a medical professional if any concerns arise. Accidental ingestion of meconium, the baby’s first bowel movement, during birth can also pose risks to the baby’s lungs and respiratory health. Prompt removal of the meconium is vital to prevent any contamination or potential harm to the developing respiratory system.
💡
You may need to know these questions about fetal breath movement
Can you see fetal breathing movements?
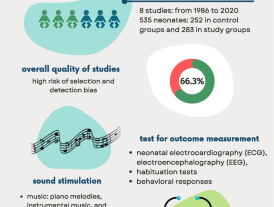
During the later stages of pregnancy, fetal breathing movements become more frequent. Around weeks 24 to 28, the practice of breathing occurs for about 10 to 20 percent of the time, which later increases to 30 to 40 percent by week 30. While observing an ultrasound in the third trimester, it is possible to witness these breathing movements, providing reassurance that everything is progressing as expected. It’s a remarkable sight that signifies the healthy development of the baby.
What are fetal breathing like movements?
Fetal breathing movements (FBMs) are fascinating rhythmic contractions of the diaphragm and other skeletal muscles that occur in healthy mammalian fetuses. These breathing-like movements are similar to postnatal breathing and are centrally organized. In addition to the diaphragm, FBMs may also engage muscles in the chest wall and upper respiratory tract. These periodic FBMs provide a glimpse into the complex development of the respiratory system in the womb.
Is it normal to feel baby breathing in the womb?
It is not normal to feel the baby breathing in the womb as they do not actually breathe in the traditional sense. Instead, babies rely on their mothers’ breathing to receive oxygen needed for their development. So, while you may feel movements from the baby in the womb when placing your palm on your tummy, these movements are not connected to the baby breathing.
What are fetal breathing movements on ultrasound?
Fetal breathing movements on ultrasound are observed as the expansion and relaxation of the diaphragm and chest wall. These movements can vary in depth and regularity. In the early stages of development, these motions can appear sporadic, but as the pregnancy progresses, they tend to adopt a more consistent pattern.
Reference source
https://www.whattoexpect.com/pregnancy/fetal-health/how-babies-breathe-womb
https://www.sciencedirect.com/topics/medicine-and-dentistry/fetus-breathing
https://adatewithbaby.com/how-to-babies-breathe-in-the-womb/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2097958/