Hidden beneath our daily activities lies a complex web of muscles that holds everything together, quite literally.
One crucial player in this intricate system is the pelvic floor muscles.
Picture a funnel-shaped pelvis, a silent hero that supports and stabilizes our pelvic organs.
However, when these muscles falter, a cascade of problems can ensue, from embarrassing moments of incontinence to the unnerving fear of organ prolapse.
Today, we journey into the realm of pelvic floor dysfunction and explore the various factors that can lead to this hidden menace.
Brace yourself for an eye-opening adventure!
funnel shaped pelvis
A funnel-shaped pelvis refers to a pelvic structure that is wider at the top and gradually narrows towards the bottom.
This anatomical variation can have implications for the function of the pelvic floor muscles.
The pelvic floor is a group of muscles that support the abdominal and pelvic organs, including the bladder, uterus, and rectum.
The levator ani muscles, specifically the pubococcygeus, iliococcygeus, and coccygeus muscles, play a crucial role in maintaining continence of the bowels and providing support to the pelvic viscera.
These muscles are innervated by the nerve to levator ani and branches of the pudendal nerve, and they receive blood supply from the inferior vesical, inferior gluteal, and pudendal arteries.
Pelvic floor dysfunction can occur due to various factors such as obstetric trauma, increasing age, obesity, and chronic straining.
This dysfunction can manifest as urinary and fecal incontinence, genitourinary prolapse, pelvic pain, and sexual dysfunction.
Key Points:
- Funnel-shaped pelvis narrows gradually from top to bottom.
- Implications for pelvic floor muscle function.
- Pelvic floor muscles support abdominal and pelvic organs.
- Levator ani muscles crucial for maintaining bowel continence and providing pelvic support.
- Innervated by nerve to levator ani and branches of pudendal nerve.
- Pelvic floor dysfunction can lead to urinary/fecal incontinence, prolapse, pain, and sexual dysfunction.
funnel shaped pelvis – Watch Video
💡
Pro Tips:
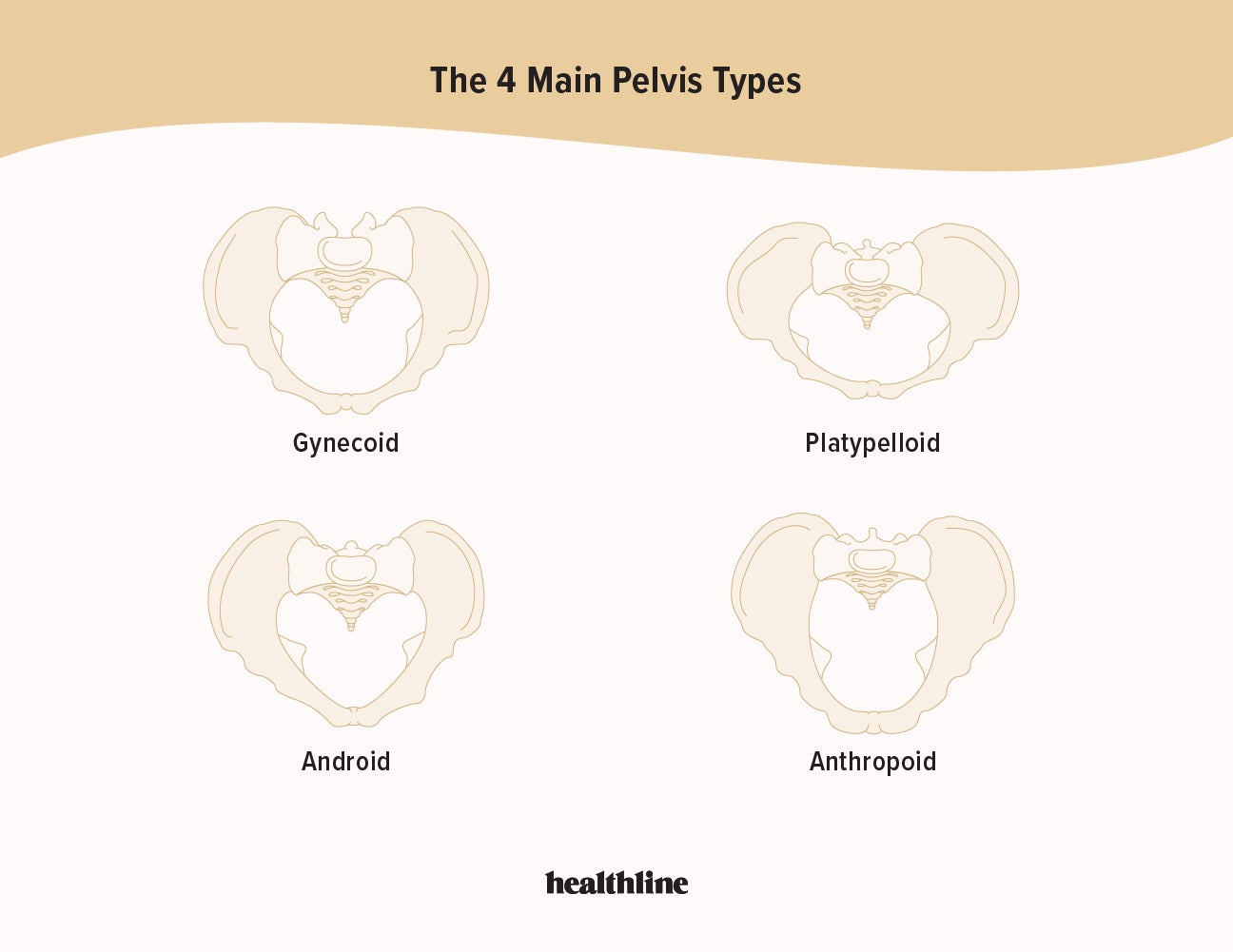
1. The funnel-shaped pelvis, also known as a gynecoid pelvis, is considered the most favorable pelvic shape for childbirth.
2. It is estimated that only about 50% of females have a naturally funnel-shaped pelvis. The remaining population has varying pelvic shapes, such as android, anthropoid, and platypelloid.
3. Some studies suggest that women with a funnel-shaped pelvis may have a higher risk of experiencing obstructed labor and requiring a cesarean section.
4. The funnel shape of the pelvis not only contributes to childbirth but also plays a crucial role in maintaining stability and balance during everyday activities.
5. The concept of the funnel-shaped pelvis has been extensively studied and depicted in ancient art and sculptures, dating back to ancient civilizations like Egypt and Greece.
The Pelvic Floor Muscles and Their Function
The pelvic floor muscles are essential for supporting the pelvic organs, maintaining continence, and providing stability in the abdominal and pelvic regions. These muscles form a muscular hammock that extends from the pubic bone to the coccyx. They comprise various muscle groups, such as the levator ani, pubococcygeus, iliococcygeus, and coccygeus muscles.
Working together, these muscles control bladder and bowel movements, support the pelvic organs, contribute to sexual function, and stabilize the pelvic region during movement.
Anatomy of the Pelvic Floor
The pelvic floor is composed of a network of muscles, ligaments, and connective tissues that form a firm support structure for the pelvic organs, including the bladder, uterus, and rectum. The levator ani muscles are the primary muscles of the pelvic floor, consisting of three parts: puborectalis, pubococcygeus, and iliococcygeus. The coccygeus muscle, also known as the ischiococcygeus, is situated posteriorly and provides additional support to the pelvic viscera. These muscles are interconnected and provide the necessary strength and flexibility to maintain pelvic organ function.
- The pelvic floor is crucial for supporting the organs in the pelvic region.
- The levator ani muscles include the puborectalis, pubococcygeus, and iliococcygeus.
- The coccygeus muscle, or ischiococcygeus, provides extra support.
- These muscles work together to ensure proper pelvic organ function.
Note: The pelvic floor is essential for maintaining pelvic organ function.
Role of the Levator Ani Muscles in Fecal Continence
The levator ani muscles are crucial for maintaining fecal continence. Specifically, the puborectalis muscle forms a muscular sling around the rectum, forming the anorectal angle. This angle acts as a barrier to prevent involuntary loss of stool and provides support to the rectum, enabling voluntary control over defecation. The contraction of the levator ani muscles during bowel movements is essential for maintaining this angle, ensuring controlled bowel emptying and preventing fecal incontinence.
Stability and Support Provided by the Pubococcygeus Muscle
The pubococcygeus muscle, the largest part of the levator ani, plays a significant role in providing stability and support to the abdominal and pelvic organs. It forms a sling-like structure that extends from the pubic bone to the coccyx, encompassing the urethra, vagina, and rectum. This muscle helps maintain pelvic organ position and contributes to the tight closure of the urethra, preventing urine leakage during physical exertion or coughing.
Additionally, the pubococcygeus muscle is involved in sexual function, contributing to orgasmic contractions.
Elevation of the Pelvic Floor by the Iliococcygeus Muscle
The iliococcygeus muscle is located above the pubococcygeus muscle and has a significant role in the elevation of the pelvic floor and the anorectal canal. It is essential in maintaining continence for both feces and gas.
By contracting and lifting the pelvic floor, the iliococcygeus muscle assists in controlling the passage of fecal matter and prevents involuntary leakage. Additionally, it plays a crucial role in supporting the pelvic organs and aids in preventing pelvic organ prolapse.
- Assists in maintaining continence
- Controls the passage of fecal matter
- Prevents involuntary leakage
- Supports pelvic organs
- Prevents pelvic organ prolapse
“The iliococcygeus muscle is important in elevating the pelvic floor and the anorectal canal, aiding in continence and preventing pelvic organ prolapse.”
Support to Pelvic Viscera by the Coccygeus Muscle
The coccygeus muscle, also known as the ischiococcygeus, is responsible for providing support to the pelvic viscera. Located at the posterior aspect of the pelvic floor, it connects the coccyx to the ischial spine. The coccygeus muscle, along with other pelvic floor muscles, plays a vital role in maintaining the position and stability of the bladder, uterus, and rectum. It acts as a firm base for the pelvic organs, preventing prolapse and ensuring their proper anatomical alignment.
- The coccygeus muscle, also known as the ischiococcygeus, provides support to the pelvic viscera.
- Situated at the posterior aspect of the pelvic floor, it connects the coccyx to the ischial spine.
- Together with other pelvic floor muscles, the coccygeus muscle helps to maintain the position and stability of the bladder, uterus, and rectum.
- It acts as a firm base for the pelvic organs, preventing prolapse and maintaining their proper anatomical alignment.
Innervation of Pelvic Floor Muscles
The pelvic floor muscles receive innervation from the nerve to levator ani and branches of the pudendal nerve. The nerve to levator ani arises from the sacral plexus and provides motor innervation to the levator ani muscles. The pudendal nerve, which originates from the sacral nerves S2-S4, supplies sensory innervation to the pelvic floor.
This innervation allows for voluntary control over the pelvic floor muscles and the coordination necessary for appropriate bladder and bowel function.
Blood Supply to the Pelvic Floor Area
The blood supply to the pelvic floor area is provided by several arteries:
- The inferior vesical arteries supply blood to the bladder and prostate in males.
- The inferior gluteal arteries contribute to the blood supply of the gluteal muscles and pelvic region.
- The pudendal arteries, along with their branches, provide blood to the external genitalia and perineum.
This extensive blood supply ensures adequate oxygenation and nutrition to the pelvic floor muscles and surrounding tissues.
Signs and Symptoms of Pelvic Floor Dysfunction
Pelvic floor dysfunction refers to a broad range of disorders that can affect the normal functioning of the pelvic floor muscles. This dysfunction can manifest with various signs and symptoms, including:
- Urinary incontinence
- Fecal incontinence
- Genitourinary prolapse (such as bladder or uterine prolapse)
- Pelvic pain
- Sexual dysfunction
Patients may experience difficulty controlling their bowel or bladder movements, pelvic pressure or heaviness, pain during intercourse, or even bulging or protrusion in the vaginal or rectal area. These symptoms can significantly impact a person’s quality of life and may require medical intervention for proper management.
Causes of Pelvic Floor Dysfunction
Numerous factors can contribute to the development of pelvic floor dysfunction.
- Obstetric trauma, such as vaginal childbirth, is a common cause, as it may lead to muscle or nerve damage.
- Increasing age can also weaken the pelvic floor muscles and contribute to dysfunction.
- Other risk factors include obesity, chronic straining during bowel movements, chronic coughing, and certain medical conditions like chronic constipation or pelvic inflammatory disease.
Understanding the underlying causes is essential in the prevention and treatment of pelvic floor dysfunction.
In conclusion, the funnel-shaped pelvis has a significant impact on childbirth. Understanding the functions of the pelvic floor muscles and their anatomy provides valuable insights into the stability, support, and control of the pelvic region.
Recognizing signs and symptoms of pelvic floor dysfunction and understanding its causes can help individuals seek appropriate medical attention and interventions for effective management. By promoting awareness and knowledge, we can empower individuals to prioritize their pelvic health and improve their overall well-being.
- It is important to consider obstetric trauma, age, obesity, chronic straining during bowel movements, chronic coughing, and certain medical conditions such as chronic constipation or pelvic inflammatory disease as potential risk factors for pelvic floor dysfunction.
💡
You may need to know these questions about funnel shaped pelvis
Is the male or female pelvis funnel shaped?
The pelvis of a female is characterized by its more spacious and less funnel-shaped structure compared to the male. This distinction arises from the wider sacrum and flatter iliac bone found in the female pelvis. Unlike the male pelvis, which exhibits a more funnel-like shape, the female pelvis accommodates for a greater amount of space within the pelvic basin. This anatomical variation is a key feature that distinguishes the male and female pelvises.
What is the funnel shaped pelvis seen in?
The funnel-shaped pelvis can be observed in a variety of anatomical structures. One notable example is the gallbladder, where the funnel-shaped pelvis functions in collecting bile before it is released into the small intestine. Another instance is the female reproductive system, where the funnel-shaped pelvis is found in the fallopian tubes, aiding in the transportation of eggs from the ovaries to the uterus. Therefore, the funnel-shaped pelvis is not limited to the renal pelvis but can be found in various essential organs and structures throughout the human body.
What is the rarest pelvic shape?
The rarest pelvic shape among different individuals is the platypelloid pelvis, also known as the flat pelvis. With its distinct characteristics, it stands out as the least common type. Resembling an egg or an oval lying on its side, the platypelloid pelvis is wide but shallow, making it a unique and uncommon variation in pelvic anatomy.
What are the 4 types of pelvis shapes?
The human pelvis can be categorized into four different shapes: gynoid, android, anthropoid, and platypelloid. The gynoid pelvis, found in 41.4% of the population, is typically characterized by a round shape with a wide pelvic inlet, allowing for an easier childbirth. The android pelvis, seen in 32.5% of individuals, is more heart-shaped and has a narrower pelvic inlet, which may pose challenges during childbirth. The anthropoid pelvis, observed in 23.5% of people, is characterized by an oval shape, resembling that of a primate, and may have varying childbirth outcomes. Lastly, the least common is the platypelloid pelvis, present in only 2.6% of individuals, which has a wide transverse and narrow anteroposterior diameter, potentially complicating childbirth.
Reference source
https://www.osmosis.org/learn/Anatomy_of_the_pelvic_cavity
https://www.rxlist.com/female_pelvis/definition.htm
https://www.toppr.com/ask/question/inner-to-the-helium-there-is-a-broad-funnel-shaped-space-called/
https://www.healthline.com/health/types-of-pelvis