– An oophorectomy is a surgical procedure to remove one or both of the ovaries, which are almond-shaped organs in the female reproductive system.
– It can be done as part of an operation to remove the uterus or independently.
– Reasons for an oophorectomy include tubo-ovarian abscess, ovarian cancer, endometriosis, noncancerous ovarian tumors or cysts, and reducing the risk of ovarian or breast cancer in high-risk individuals.
– Risks of the procedure include bleeding, infection, damage to nearby organs, rupture of a tumor, and retention of ovary cells that cause symptoms.
– If both ovaries are removed, the person will experience menopause, which can lead to signs and symptoms such as hot flashes, vaginal dryness, depression, anxiety, heart disease, memory problems, decreased sex drive, and osteoporosis.
– Undergoing an oophorectomy at a younger age may increase the risks related to early menopause.
– Preparing for an oophorectomy may involve fasting before the surgery, stopping certain medications, and undergoing imaging tests like ultrasound and blood tests.
– Discussing options for infertility preservation with a doctor is recommended for those who want to have children.
– The article provides information about oophorectomy, a surgical procedure to remove the ovaries.
– It discusses two methods of performing the surgery: laparotomy and laparoscopic surgery.
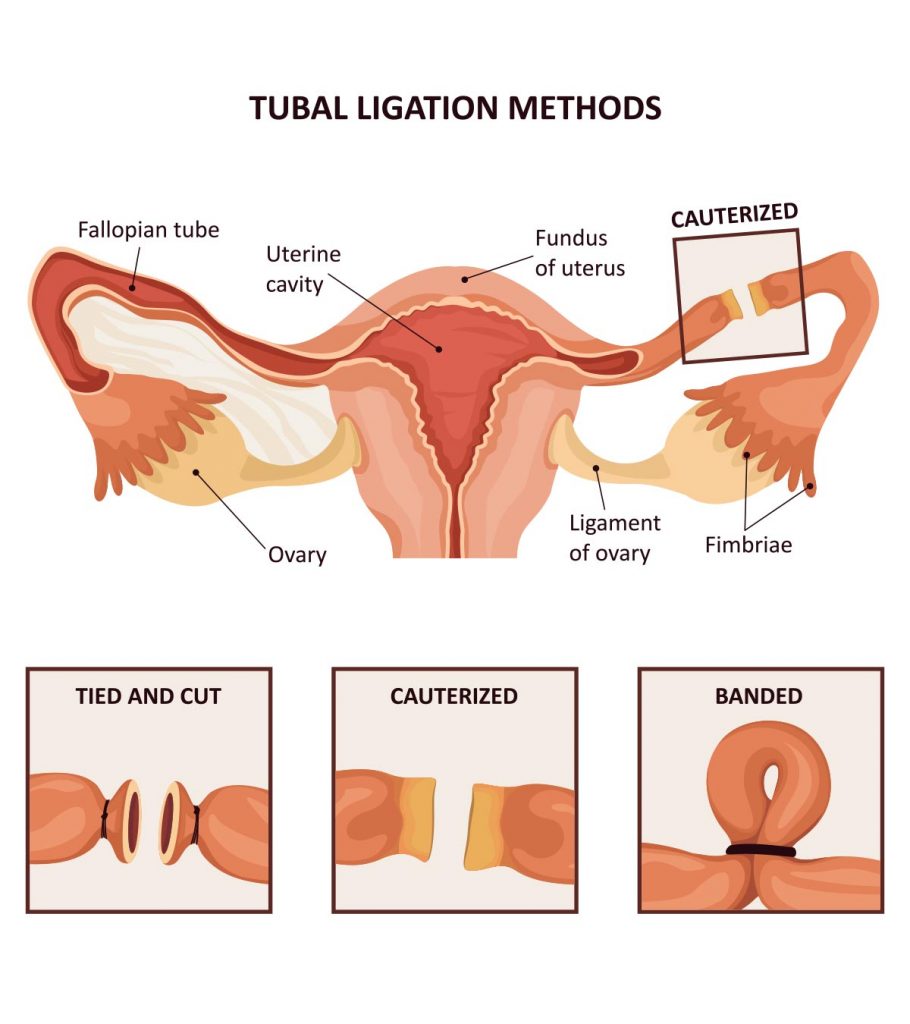
– Both methods involve separating the ovaries from their blood supply and surrounding tissue before removal.
– Laparoscopic or robotic oophorectomy is generally associated with quicker recovery, less pain, and a shorter hospital stay.
– After the surgery, patients can expect to spend time in a recovery room and may need to stay in the hospital for a few hours to a few days.
– Most people can go home after the surgery and can return to normal activities within two to four weeks, depending on individual circumstances.
– Oophorectomy is a surgical procedure to remove one or both ovaries.
– It is commonly done to treat diseases or reduce the risk of certain cancers.
– There are different types of oophorectomies including unilateral (removing one ovary), bilateral (removing both ovaries), salpingo-oophorectomy (removing one ovary and one fallopian tube), bilateral salpingo-oophorectomy (removing both fallopian tubes and ovaries), hysterectomy with salpingo-oophorectomy (removing uterus, one fallopian tube, and one ovary), and total hysterectomy with bilateral salpingo-oophorectomy (removing uterus, cervix, both fallopian tubes, and both ovaries).
– Reasons for oophorectomy include endometriosis, benign cysts, preventative surgery for high-risk individuals for breast and ovarian cancer due to BRCA gene mutations, ovarian cancer, ovarian torsion, and infections.
– If both ovaries and fallopian tubes are removed, natural pregnancy becomes impossible, but options like IVF can still be considered.
– Fertility preservation options such as egg freezing may also be discussed with a healthcare provider.
Continue Reading