In the vast ecosystem of microorganisms that call the human body their home, there are some that remain relatively unknown, lurking in the shadows of scientific exploration.
One such enigmatic resident is Haemophilus vaginalis, a bacterium shrouded in mystery.
This tiny but captivating microbe captivates researchers who strive to unravel its secrets and uncover its potential impact on human health.
Journey with us as we delve into the realm of Haemophilus vaginalis, uncovering the intriguing world of these elusive microorganisms.
haemophilus vaginalis
Haemophilus vaginalis is a bacterium that has been associated with various infections in the genital area, particularly in women.
It is typically found in the vaginal microbiota, but can also be present in the urethra and cervix.
This bacterium is known to contribute to bacterial vaginosis, a common condition characterized by an imbalance in the vaginal flora.
Haemophilus vaginalis can cause symptoms such as vaginal discharge, itching, and irritation.
Prompt diagnosis and appropriate treatment are important to prevent complications and improve the quality of life for affected individuals.
Key Points:
- Haemophilus vaginalis is a bacterium associated with genital infections in women.
- It is commonly found in the vaginal microbiota but can also be present in the urethra and cervix.
- The bacterium contributes to bacterial vaginosis, a condition characterized by an imbalance in vaginal flora.
- Symptoms caused by Haemophilus vaginalis include vaginal discharge, itching, and irritation.
- Prompt diagnosis and appropriate treatment are crucial to prevent complications.
- Treatment can significantly improve the quality of life for affected individuals.
haemophilus vaginalis – Watch Video
💡
Pro Tips:
1. In spite of its name, Haemophilus vaginalis does not only affect the vaginal area in women. It can also colonize other sites of the body, such as the respiratory tract and the gastrointestinal tract.
2. Haemophilus vaginalis is actually not a true member of the genus Haemophilus. It was later reclassified as Gardnerella vaginalis due to its distinct characteristics and its role in causing bacterial vaginosis.
3. Haemophilus vaginalis is an anaerobic bacterium, meaning it thrives in environments devoid of oxygen. This is why it can be found naturally in the vaginal microbiota, which is an anaerobic ecosystem.
4. Haemophilus vaginalis was discovered by Albert Döderlein in 1892. However, it was initially classified as a normal inhabitant of the female genital tract, suggesting a symbiotic rather than pathogenic relationship with its host.
5. Research has shown that the presence of Haemophilus vaginalis in the vaginal microbiota can influence the susceptibility to sexually transmitted infections. This has led scientists to investigate potential links between this bacterium and the development of certain diseases.
Introduction To Haemophilus Vaginalis
Haemophilus vaginalis is a bacterium commonly found in the urogenital tract of both men and women. While it is a normal inhabitant of the vaginal flora, it can also be associated with various health issues, particularly in women. This article aims to provide information on the causes, symptoms, diagnosis, treatment, prevention, complications, and current research surrounding Haemophilus vaginalis.
Causes:
- Haemophilus vaginalis belongs to the Haemophilus genus, which includes other pathogenic species like Haemophilus influenzae.
- It can colonize parts of the urogenital tract, such as the urethra and cervix, in addition to the vaginal area.
- Transmission primarily occurs through sexual contact, but other means of transmission are also possible.
Symptoms:
- In many cases, Haemophilus vaginalis does not cause any symptoms and may go unnoticed.
- However, it can lead to various health issues, such as vaginal discharge, itching, and discomfort.
- Some individuals may also experience urinary symptoms, such as pain or burning during urination.
Diagnosis:
- The diagnosis of Haemophilus vaginalis infection is typically made by collecting a sample from the affected area.
- The sample is then examined under a microscope or sent to a laboratory for further testing, including culture and identification of the bacterium.
Treatment:
- Treatment for Haemophilus vaginalis infection usually involves the use of antibiotics that are effective against this bacterium.
- The specific antibiotic prescribed may vary depending on the severity of the infection and the individual’s medical history.
- It is important to complete the full course of antibiotics as prescribed by a healthcare professional.
Prevention:
- Practicing safe sex, such as using condoms, can reduce the risk of acquiring Haemophilus vaginalis through sexual contact.
- Maintaining good hygiene and avoiding douching can also help prevent infections.
- Regular medical check-ups and screenings can aid in the early detection and timely treatment of any urogenital infections.
Complications:
- If left untreated, Haemophilus vaginalis infections can lead to complications, such as pelvic inflammatory disease (PID) in women.
- PID can cause long-term complications, including infertility and chronic pelvic pain.
- Prompt diagnosis and appropriate treatment are crucial in preventing such complications.
“Haemophilus vaginalis is a bacterium commonly found in the urogenital tract. It can lead to various health issues in women. Transmission primarily occurs through sexual contact, but other means of transmission are also possible.”
- Causes:
- Haemophilus vaginalis belongs to the Haemophilus genus, which includes other pathogenic species.
- It can colonize the urethra, cervix, and vaginal area.
- Symptoms:
- Vaginal discharge, itching, and discomfort.
- Urinary symptoms like pain or burning during urination.
- Diagnosis:
- Sample collection and laboratory testing.
- Treatment:
- Antibiotics prescribed based on severity and medical history.
- Complete the full course of antibiotics.
- Prevention:
- Practicing safe sex (using condoms) and maintaining good hygiene.
- Regular medical check-ups and screenings.
- Complications:
- Untreated infections can lead to pelvic inflammatory disease (PID).
- PID can cause long-term complications like infertility and chronic pelvic pain.
Causes And Risk Factors
The primary cause of Haemophilus vaginalis infection is intimate contact with an infected individual. This can include sexual intercourse, but it can also be spread through other sexual activities that involve exchange of bodily fluids. Certain risk factors may increase the likelihood of acquiring an infection, including:
- Multiple sexual partners
- Unprotected sex
- History of sexually transmitted infections (STIs)
Additionally, factors such as the use of certain contraceptives like diaphragms and spermicides, hormonal changes during pregnancy, and a weakened immune system can contribute to the development of Haemophilus vaginalis infection.
It is important to note that not all individuals who engage in these risk factors will develop an infection, as the presence of Haemophilus vaginalis alone may not always lead to symptoms or complications.
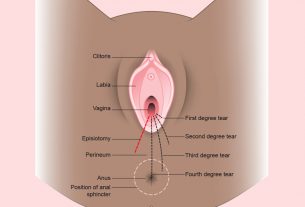
Symptoms And Diagnosis
Haemophilus vaginalis infection can present differently in each individual. Some individuals may not experience any symptoms, while others may have symptoms such as:
- Vaginal discharge
- Itching
- Burning sensation
- Pain during urination
- Discomfort during sexual intercourse
It is crucial to distinguish these symptoms from other vaginal infections or conditions, as the appropriate treatment may vary.
To diagnose Haemophilus vaginalis infection, healthcare providers often:
1. Perform a physical examination
2. Inquire about symptoms and medical history
3. Conduct laboratory tests
During the examination, a vaginal swab is usually taken to collect a sample for microscopic examination and laboratory culture. This allows for the identification of Haemophilus vaginalis and the exclusion of other possible pathogens. Accurate diagnosis is essential to ensure proper management of the infection.
Treatment Options
The treatment of Haemophilus vaginalis infection usually requires antibiotics. The selection and duration of antibiotic treatment will be determined by various factors, including the severity of symptoms, presence of co-infections, and results from antibiotic susceptibility testing.
Commonly used antibiotics for Haemophilus vaginalis include metronidazole, azithromycin, and doxycycline.
Both sexual partners should receive treatment simultaneously to prevent reinfection. During treatment, it is important to abstain from sexual activity and avoid contact with bodily fluids to minimize transmission. Completing the full course of antibiotics is crucial, even if symptoms improve. Regular follow-up visits with healthcare professionals are necessary to ensure successful treatment of the infection.
Prevention Of Haemophilus Vaginalis Infection
Preventing Haemophilus vaginalis infection involves practicing safe sex and adopting healthy sexual behaviors. This includes using barrier methods of contraception, such as condoms, and engaging in open and honest communication about sexual history with partners. Regular screening for STIs and seeking prompt treatment for any suspected infections is also crucial in preventing the spread of Haemophilus vaginalis and other pathogens.
Maintaining good genital hygiene and avoiding the use of irritating substances, such as douches or scented products, can also reduce the risk of developing an infection. It is important to remember that even individuals who do not experience any symptoms can still transmit Haemophilus vaginalis to sexual partners. Education about safe sex practices and open dialogue with healthcare providers are key components of prevention.
Complications And Long-Term Effects
While Haemophilus vaginalis infection is generally considered a mild condition, it can lead to complications if left untreated. If the infection spreads to other parts of the reproductive system, it can cause pelvic inflammatory disease (PID), which can result in chronic pain, infertility, and ectopic pregnancy. Furthermore, individuals with Haemophilus vaginalis infection may have an increased risk of acquiring other STIs, such as gonorrhea and chlamydia.
In some cases, the long-term effects of Haemophilus vaginalis infection may not manifest immediately. Therefore, it is crucial to receive timely and appropriate treatment to prevent potential complications. Regular check-ups with healthcare providers should be prioritized, even if symptoms have resolved, to monitor for any ongoing issues or secondary infections.
Haemophilus Vaginalis In Women
Haemophilus vaginalis is a bacterium that is particularly concerning for women, as it is associated with potential gynecological complications. One notable complication is the development of PID (Pelvic Inflammatory Disease), which can have significant long-term consequences.
In addition, women who are pregnant and contract a Haemophilus vaginalis infection may experience complications such as preterm labor and delivery.
Therefore, it is crucial for women to be aware of the symptoms associated with Haemophilus vaginalis infection and to seek medical attention if necessary. Prompt diagnosis and treatment are key in preventing potential reproductive health complications.
To protect themselves, women should practice safe sex, use barrier methods of contraception, and attend regular gynecological check-ups.
Haemophilus Vaginalis In Men
Although Haemophilus vaginalis is commonly associated with women’s health, it can also affect men. Men who engage in sexual activities with individuals infected with Haemophilus vaginalis are at risk of acquiring the bacterium and developing symptoms such as discharge from the urethra, discomfort during urination, and irritation of the genital area.
Similar to women, men should engage in safe sex practices, including the consistent use of condoms, to reduce the risk of contracting and spreading Haemophilus vaginalis. Individuals who experience any unusual symptoms should seek medical advice for proper diagnosis and treatment. It is important to remember that Haemophilus vaginalis can affect people of any gender and sexual orientation.
Current Research And Advances In Treatment
Ongoing research primarily focuses on understanding the biology and pathogenesis of Haemophilus vaginalis in order to develop more effective treatments and preventive strategies. Scientists are investigating the mechanisms by which Haemophilus vaginalis colonizes and persists in the urogenital tract, as well as exploring its interactions with the host immune system.
Advances in diagnostic techniques, particularly the use of molecular methods, are being explored to improve the accuracy and speed of Haemophilus vaginalis detection. These advancements will aid in early identification of the infection, enabling timely treatment.
Furthermore, researchers are working on the development of novel antibiotics that specifically target Haemophilus vaginalis while minimizing potential side effects. This approach aims to provide healthcare providers with a wider range of treatment options and potentially reduce the risk of antibiotic resistance.
Conclusion And Takeaways
Haemophilus vaginalis is a bacterium that colonizes the urogenital tract and poses significant health risks, particularly in women. It is primarily transmitted through intimate contact, leading to symptoms such as vaginal discharge and discomfort during urination. Prompt diagnosis and treatment with appropriate antibiotics are crucial in preventing complications, including pelvic inflammatory disease and infertility.
To prevent Haemophilus vaginalis infection, practicing safe sex, undergoing regular check-ups with healthcare providers, and maintaining good genital hygiene play a vital role. Ongoing research is dedicated to enhancing our understanding of Haemophilus vaginalis and developing more effective treatments and preventive measures. By staying informed, practicing safe behaviors, and seeking medical attention whenever necessary, individuals can safeguard their reproductive health and minimize the impact of Haemophilus vaginalis infection.
💡
You may need to know these questions about haemophilus vaginalis
Can a man pass gardnerella to a woman?
While gardnerella vaginallis is not classified as a sexually transmitted infection, it can still be transmitted from a woman to a man during unprotected sexual intercourse. However, there is no clear evidence suggesting that an infected man can pass the condition to a woman. Gardnerella vaginallis primarily affects women and is characterized by an imbalance of bacteria in the vagina. It is important for both partners to practice safe sexual habits and maintain proper hygiene to minimize the risk of transmission and maintain overall vaginal health.
Is Megasphaera a STD?
While Megasphaera species have been associated with a heightened risk of HIV transmission, it is important to note that Megasphaera itself is not considered a sexually transmitted disease (STD). However, its presence in the urogenital tracts of adolescent males and heterosexual couples suggests that these bacteria may potentially be transmitted through sexual activity. Further research is needed to fully understand the transmission dynamics of Megasphaera and its role in sexual health.
Is gardnerella bacteria a STD?
No, gardnerella bacteria is not classified as a sexually transmitted bacteria. Unlike the bacterial strains responsible for STDs such as gonorrhea, syphilis, or chlamydia, having gardnerella bacteria in the vagina does not necessarily indicate an infection. In fact, gardnerella is naturally found in healthy vaginas. Therefore, while it is important to be mindful of maintaining vaginal health, the presence of gardnerella alone should not be a cause for concern regarding STD transmission.
What does it mean if you test positive for gardnerella?
If you test positive for Gardnerella, it indicates that you have been infected by this bacteria which can lead to bacterial vaginosis (BV). BV is a condition characterized by an imbalance in the vaginal microbiota. This means that the naturally occurring bacteria in the genital tract are disrupted, leading to discomfort and abnormal vaginal discharge. It is important to seek proper treatment to restore the bacterial balance and prevent further complications. Additionally, it is crucial to inform your sexual partner as Gardnerella can be passed on during sexual intercourse.
Reference source
https://yoursexualhealth.co.uk/blog/gardnerella-vaginallis-in-men/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8767330/
https://my.clevelandclinic.org/health/body/22001-gardnerella-vaginalis
https://pubmed.ncbi.nlm.nih.gov/6153721/