In the realm of medical mysteries, there exists a peculiar condition known as a hydatidiform mole.
With its abnormal growth of the placenta and potential to transform into cancer, it stands as a rare enigma that demands our attention.
Join us as we delve into this intriguing world, where vigilance and support are paramount.
hydatidiform mole
A hydatidiform mole, also known as a molar pregnancy, is a rare condition where there is abnormal and rapid growth of part or all of the placenta, resulting in a larger than normal size and the presence of fluid-filled cysts.
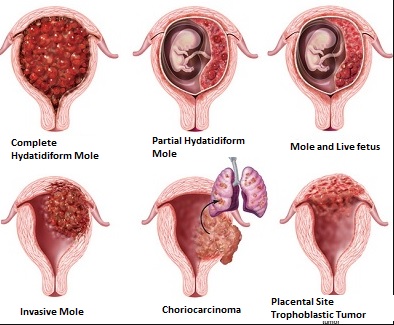
There are two types of molar pregnancies: complete molar pregnancy, where a fetus does not develop, and partial molar pregnancy, where a fetus develops but is abnormal and cannot survive beyond three months.
Typical symptoms of pregnancy may still be experienced, such as morning sickness or sore breasts.
However, there is a risk that the placenta can develop into choriocarcinoma, a rare form of cancer.
Regular monitoring of hCG levels is necessary to detect any remaining molar cells, and treatment may be required if hCG levels do not decrease.
Emotional healing after a molar pregnancy can take time, and seeking support is recommended.
Key Points:
- Hydatidiform mole is a rare condition where there is abnormal and rapid growth of part or all of the placenta
- There are two types: complete molar pregnancy (no fetus development) and partial molar pregnancy (abnormal fetus)
- Symptoms of pregnancy can still be experienced, such as morning sickness or sore breasts
- There is a risk of the placenta developing into choriocarcinoma, a rare form of cancer
- Regular monitoring of hCG levels is necessary to detect remaining molar cells
- Emotional healing after a molar pregnancy can take time, seeking support is recommended
hydatidiform mole – Watch Video
💡
Pro Tips:
1. Despite being called a “mole,” a hydatidiform mole is not an actual mole or a mammal. It is a rare benign tumor that forms in the uterus during pregnancy.
2. Hydatidiform moles are characterized by the abnormal growth of placental tissue, leading to the formation of grape-like clusters instead of a fetus. This results in a molar pregnancy, which can be potentially dangerous and require medical intervention.
3. Hydatidiform moles are often associated with abnormal chromosome patterns. Instead of the usual chromosomal arrangement in humans (46 chromosomes), hydatidiform moles can have either a complete paternal chromosome set or multiple sets of paternal chromosomes.
4. In some cases, the development of a hydatidiform mole can be preceded by a complete or partial loss of paternal chromosomes, leaving only the maternal chromosomes to contribute to the growth of the placenta. This can lead to an abnormal pregnancy with no fetal development.
5. Though usually benign, hydatidiform moles have a small risk of progressing into a malignant form called “choriocarcinoma.” This rare occurrence can spread to other parts of the body, requiring prompt medical intervention and treatment.
Rare Condition Affecting Pregnancies: Hydatidiform Mole
Hydatidiform mole, also known as a molar pregnancy, is a rare condition that affects approximately 1 in 1,200 pregnancies. This abnormal pregnancy occurs when there is abnormal and rapid growth of part or all of the placenta. As a result, the placenta becomes larger than normal, and fluid-filled cysts may be present. The fetus in a molar pregnancy may not develop at all or may be abnormal and unable to survive beyond three months.
Detecting a molar pregnancy is crucial for proper management and care. It is typically identified in early pregnancy through ultrasound or by examining tissue after a miscarriage. Women who experience symptoms such as morning sickness or sore breasts, which are typically associated with a normal pregnancy, may still have a molar pregnancy. This is because the placenta in a molar pregnancy continues to produce the pregnancy hormone hCG, despite the abnormality.
Detection Of Hydatidiform Mole Through Ultrasound Or Tissue Examination
Early detection of a hydatidiform mole is essential for appropriate medical intervention. Ultrasound imaging is commonly used to diagnose a molar pregnancy. During an ultrasound, the abnormal growth of the placenta and the presence of cysts can be visualized. This imaging technique provides valuable information regarding the size and characteristics of the molar pregnancy.
In some cases, a molar pregnancy may result in a miscarriage. Following a miscarriage, the tissue is often examined to confirm the diagnosis. Microscopic examination of the tissue can reveal the presence of characteristic changes, such as the absence of embryonic structures or the presence of abnormal placental tissue.
Abnormal Growth And Cysts In Molar Pregnancy
The hallmark of a molar pregnancy is the abnormal and rapid growth of part or all of the placenta. The placenta usually plays the crucial role of providing nutrients and oxygen to the developing fetus. However, in a molar pregnancy, the placenta becomes enlarged and may develop fluid-filled cysts.
These cysts are small, sac-like structures filled with fluid. They can vary in size and number. The presence of these cysts is one of the key features that distinguish a molar pregnancy from a normal one. The abnormal growth and cysts can be visualized through ultrasound imaging, providing medical professionals with important diagnostic information.
- Abnormal and rapid growth of the placenta
- Enlargement of the placenta and development of fluid-filled cysts
“The hallmark of a molar pregnancy is the abnormal and rapid growth of part or all of the placenta.”
Types Of Molar Pregnancy: Complete And Partial
Molar pregnancies can be classified into two main types: complete molar pregnancy and partial molar pregnancy.
In a complete molar pregnancy, a fetus does not develop at all. Instead, there is only abnormal placental tissue. The absence of a fetus is due to an error during fertilization, where the egg is fertilized by an empty sperm or two sperm.
On the other hand, a partial molar pregnancy is characterized by the presence of an abnormal fetus. However, the fetus is not viable and cannot survive beyond three months. In a partial molar pregnancy, both normal and abnormal placental tissue are present. The abnormal development of the fetus in a partial molar pregnancy is usually the result of an extra set of chromosomes.
It is essential to accurately diagnose the type of molar pregnancy to guide appropriate management and follow-up care.
Key points:
- Complete molar pregnancies have no fetus and only abnormal placental tissue.
- Partial molar pregnancies have an abnormal fetus that cannot survive beyond three months.
- Both normal and abnormal placental tissue are present in partial molar pregnancies.
- Accurate diagnosis is crucial for proper management and follow-up care.
“It is essential to accurately diagnose the type of molar pregnancy to guide appropriate management and follow-up care.”
Symptoms And Hormone Production In Molar Pregnancy
While molar pregnancies are abnormal and cannot lead to a healthy pregnancy, women may still experience typical symptoms associated with pregnancy. This is because the placenta in a molar pregnancy continues to produce the pregnancy hormone hCG, even though the pregnancy is abnormal.
Symptoms such as morning sickness, nausea, vomiting, and sore breasts are common in molar pregnancies, similar to a normal pregnancy. These symptoms occur due to the presence of hCG, which stimulates changes in the body to support a developing fetus.
It is important to note that experiencing these symptoms does not necessarily indicate a healthy pregnancy. If a molar pregnancy is suspected, further diagnostic tests, such as ultrasound or tissue examination, should be conducted to confirm the diagnosis.
- Molar pregnancies are abnormal and cannot lead to a healthy pregnancy.
- Symptoms of molar pregnancies are similar to a normal pregnancy due to the production of hCG by the placenta.
- Experiencing typical pregnancy symptoms does not guarantee a healthy pregnancy.
- Diagnostic tests like ultrasound or tissue examination are necessary to confirm a molar pregnancy.
Malignant Potential: Hydatidiform Mole Leading To Choriocarcinoma
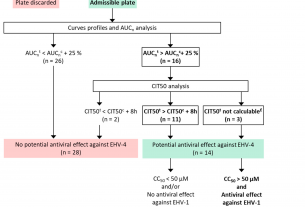
While most molar pregnancies are benign and do not pose a significant health risk, there is a small chance that the abnormal placenta can become malignant. In rare cases, a molar pregnancy can lead to the development of choriocarcinoma, a type of gestational trophoblastic disease that is a form of cancer.
Choriocarcinoma occurs when the abnormal placental tissue becomes cancerous and starts invading the uterine wall. From there, it has the potential to spread to other organs, such as the lungs, liver, and brain, through the bloodstream.
Fortunately, choriocarcinoma is highly responsive to chemotherapy. Timely detection and treatment can lead to successful management and cure of this rare form of cancer associated with molar pregnancies. Regular monitoring of hCG levels is crucial to identify any persistent molar cells that could potentially develop into choriocarcinoma.
Risk Factors For Molar Pregnancy
Several risk factors have been identified for molar pregnancy. Age is an important factor, with women under 18 or over 35 being at a higher risk. Additionally, women of Asian or Mexican background have a slightly increased risk compared to other ethnic groups.
Certain dietary factors may also play a role. A diet low in carotene, a plant pigment that is converted to vitamin A in the body, has been associated with an increased risk of molar pregnancy. Therefore, maintaining a well-balanced diet that includes a variety of fruits and vegetables is important during pregnancy.
Women who have previously had a molar pregnancy or another type of gestational trophoblastic tumor are also at a higher risk of experiencing a future molar pregnancy.
GTD Registry For Monitoring And Follow-Up Care
To ensure proper monitoring and follow-up care for women who have experienced a molar pregnancy, specialized registries have been established. One notable registry is the Gestational Trophoblastic Disease (GTD) Registry at the Royal Women’s Hospital.
These registries serve as an important resource for healthcare providers to track the health of women who have had a molar pregnancy. The GTD Registry provides ongoing monitoring and follow-up care, including:
- Regular assessment of hCG levels
- Imaging studies
- Consultations with specialists
By participating in these registries, women can receive comprehensive care and support tailored to their specific needs. Regular monitoring helps to detect any potential complications or reoccurrence of molar pregnancy, enabling timely intervention and management.
Bullet points:
- Regular assessment of hCG levels
- Imaging studies
- Consultations with specialists
Importance Of Monitoring hCG Levels And Potential Treatment
One of the key aspects of managing a molar pregnancy is monitoring the levels of the pregnancy hormone hCG. Following the removal of the molar tissue or after a miscarriage associated with a molar pregnancy, serial hCG tests are performed.
The hCG levels should decrease steadily over time. Persistently high or rising hCG levels may indicate the presence of abnormal molar cells that could potentially grow or spread to other organs. In such cases, further treatment may be necessary to remove the remaining molar tissue and prevent complications.
Monitoring hCG levels typically involves both urine and blood collection. Results from these tests provide valuable information to healthcare providers and help guide appropriate treatment decisions.
Emotional Healing And Support After A Molar Pregnancy
Dealing with a molar pregnancy can be emotionally challenging. Women may experience feelings of grief, loss, and confusion. It is important to acknowledge these emotions and seek support from family, friends, and healthcare professionals.
The GTD Registry team at the Royal Women’s Hospital and other similar organizations provide valuable emotional support and counseling. These teams understand the unique challenges associated with molar pregnancies and are equipped to offer guidance and assistance throughout the healing process.
In addition to seeking professional support, connecting with others who have experienced molar pregnancies and sharing experiences can also be beneficial. Support groups, online forums, and social media communities can provide a sense of belonging and understanding during the emotional healing journey.
Hydatidiform mole, or molar pregnancy, is a rare condition that affects a small percentage of pregnancies. Timely detection through ultrasound or tissue examination is crucial for accurate diagnosis and appropriate management. Women with a molar pregnancy may experience symptoms similar to a normal pregnancy due to the production of hCG by the abnormal placenta. Although most molar pregnancies are benign, there is a small risk of the placenta becoming malignant and developing into choriocarcinoma. Various risk factors have been identified, and specialized registries are available to provide monitoring and follow-up care. Regular monitoring of hCG levels is essential, and emotional healing and support play an important role in the recovery process. With proper medical care and emotional support, women can navigate the enigmatic world of gestational trophoblastic diseases and move forward towards a healthy future.
💡
You may need to know these questions about hydatidiform mole
Is a hydatidiform mole a miscarriage?
A hydatidiform mole is not technically considered a miscarriage, but rather a rare abnormality in pregnancy. It occurs when an abnormal fertilized egg implants in the uterus, leading to the growth of a mass of tissue instead of a developing fetus. In a complete hydatidiform mole, no fetus develops at all, while in a partial mole, a fetus may develop but will be abnormal and cannot survive for more than a few months. Thus, while a hydatidiform mole does result in the loss of a potential pregnancy, it is distinct from a traditional miscarriage in terms of its underlying mechanism and prognosis.
What is the symptoms of hydatidiform mole?
Hydatidiform mole, also known as a molar pregnancy, presents unique symptoms that differ from a normal pregnancy. One prominent sign is the rapid enlargement of the uterus, far exceeding the typical growth rate. Additionally, most women experience severe nausea, vomiting, and vaginal bleeding, while some may also exhibit elevated blood pressure. These symptoms provide crucial information for medical professionals to evaluate and diagnose a hydatidiform mole in affected women.
What is hydatidiform mole pregnancy with a fetus?
A hydatidiform mole pregnancy with a fetus refers to a unique and uncommon form of gestational trophoblastic disease. It involves the presence of twin pregnancies, where one embryo develops into a hydatidiform mole and the other continues to grow as a live fetus. This condition carries an elevated risk of obstetric complications and has a poor perinatal outcome. Accurate prenatal diagnosis is crucial in order to provide appropriate counseling to couples and ensure close monitoring in specialized medical centers.
Is hydatidiform mole curable?
Hydatidiform mole, a condition characterized by abnormal growth of placental tissue, has seen a drastic reduction in mortality rates due to early diagnosis and proper treatment. With the current advancements in medical science, the mortality rate for this condition is essentially zero. However, it is important to note that around 20% of women with a complete mole may develop a trophoblastic malignancy. Fortunately, gestational trophoblastic neoplasia, the type of cancer that may arise from this condition, holds an excellent prognosis with nearly 100% curability. Therefore, with timely detection and appropriate therapy, hydatidiform mole and its potential complications can be effectively treated and managed.
Reference source
https://www.ncbi.nlm.nih.gov/books/NBK459155/
https://www.thewomens.org.au/health-information/pregnancy-and-birth/pregnancy-problems/early-pregnancy-problems/hydatidiform-mole
https://www.msdmanuals.com/home/women-s-health-issues/cancers-of-the-female-reproductive-system/molar-pregnancy
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5769672/