Imagine the anticipation and excitement of welcoming a new life into the world.
But what happens when the journey is far from smooth sailing?
Enter hypertonic uterine inertia, a perplexing condition that plunges expectant mothers into a whirlwind of weak contractions and unanswered questions.
With its obscure origins and potential complications, this obstetric enigma can turn an eagerly awaited arrival into a harrowing ordeal.
Fasten your seatbelts, as we embark on a journey filled with unexpected twists and turns in the realm of hypertonic uterine inertia and its sinister accomplice, cervical dystocia.
hypertonic uterine inertia
Hypertonic uterine inertia refers to infrequent, weak, and short-duration uterine contractions that occur during labor.
The causes of hypertonic uterine inertia are unknown, but factors such as primigravida (particularly elderly), anemia, nervousness, hormonal deficiencies, and uterine abnormalities may be involved.
There are two categories of hypertonic uterine inertia: primary and secondary.
Primary inertia occurs when weak contractions are present from the start of labor, while secondary inertia occurs when initially strong contractions become weak and inadequate.
Clinical symptoms include prolonged labor, slow cervical dilatation, and intact membranes.
Complications can include retained placenta and postpartum hemorrhage.
Diagnosis is done through tocography and examination, and management may involve proper labor management, medications, and operative delivery if necessary.
Key Points:
- Hypertonic uterine inertia is characterized by infrequent, weak, and short-duration uterine contractions during labor.
- Potential causes include factors such as primigravida, anemia, nervousness, hormonal deficiencies, and uterine abnormalities.
- Hypertonic uterine inertia can be categorized as primary or secondary, depending on the timing and strength of contractions.
- Clinical symptoms include prolonged labor, slow cervical dilatation, and intact membranes.
- Possible complications include retained placenta and postpartum hemorrhage.
- Diagnosis involves tocography and examination, and management may include proper labor management, medications, and operative delivery if necessary.
hypertonic uterine inertia – Watch Video
💡
Pro Tips:
1. Hypertonic uterine inertia, also known as secondary uterine inertia, is a condition characterized by excessive contractions of the uterus during labor, which can lead to prolonged or difficult delivery.
2. While rare, hypertonic uterine inertia can be caused by a variety of factors, including anxiety, stress, dehydration, caffeine consumption, or the use of certain medications.
3. In some cases, hypertonic uterine inertia can be influenced by the position of the baby during labor. Certain positions may cause the uterus to contract more forcefully, leading to the condition.
4. Hypertonic uterine inertia can significantly increase the risk of fetal distress or complications during delivery, making it important for medical professionals to closely monitor and manage the condition.
5. To treat hypertonic uterine inertia, medical interventions such as intravenous fluids, pain management, or uterine relaxant medications may be used to help regulate contractions and ensure safer delivery for both the mother and baby.
Definition And Characteristics
Hypertonic uterine inertia is a condition characterized by infrequent, weak, and short-duration uterine contractions. These contractions are not strong enough to effectively progress labor, resulting in prolonged labor. The condition is marked by slow cervical dilatation and intact membranes. However, it generally has little impact on the mother and fetus apart from causing maternal anxiety.
To summarize:
- Hypertonic uterine inertia involves infrequent, weak, and short-duration uterine contractions.
- These contractions are not sufficient for labor progression, leading to prolonged labor.
- The condition is identified by slow cervical dilatation and intact membranes.
- Fortunately, it typically does not pose significant risks to the mother or fetus, except for causing maternal anxiety.
Unknown Causes
The causes of hypertonic uterine inertia are still unknown. Multiple factors may contribute to the development of this condition. Some possible factors include:
- primigravida (particularly elderly)
- anemia
- nervousness
- hormonal deficiencies
- improper use of analgesics
- uterine overdistension
- developmental anomalies
- myomas
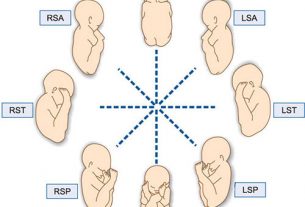
- malpresentations
- malpositions
- cephalopelvic disproportion
- a full bladder or rectum
However, more research is needed to determine the exact mechanisms behind the occurrence of hypertonic uterine inertia.
Factors Involved In Hypertonic Uterine Inertia
Several factors have been identified in association with hypertonic uterine inertia.
- Primigravida individuals, especially those who are older, are more prone to developing this condition.
- Anemia, nervousness, and hormonal deficiencies can also contribute to the occurrence of hypertonic uterine inertia.
- Improper use of analgesics, uterine overdistension, developmental anomalies, myomas, malpresentations, malpositions, cephalopelvic disproportion, and a full bladder or rectum can further exacerbate the problem.
Note: It is important to address these factors and consider appropriate management strategies to prevent or treat hypertonic uterine inertia.
Categorization: Primary And Secondary Inertia
Hypertonic uterine inertia can be categorized into two types: primary and secondary inertia. Primary inertia occurs when weak contractions are present from the start of labor. In contrast, secondary inertia involves initially strong contractions that later become weak and inadequate to overcome an obstruction. The distinction between primary and secondary inertia helps in determining the appropriate management approach for each case.
Symptoms And Impact On Mother And Fetus
Clinical symptoms of hypertonic uterine inertia include prolonged labor, infrequent and weak contractions, slow cervical dilatation, intact membranes, and little impact on the mother and fetus apart from maternal anxiety. While the condition itself may not pose significant risks to the mother and baby, it can lead to complications such as retained placenta and postpartum hemorrhage if not properly managed.
Potential Complications
Complications that can arise from hypertonic uterine inertia include retained placenta and postpartum hemorrhage. If the contractions are unable to effectively expel the placenta, it may become lodged in the uterus, leading to the need for medical intervention. Postpartum hemorrhage can occur when the uterus fails to contract adequately after delivery, resulting in excessive bleeding.
These complications highlight the importance of timely and appropriate management of hypertonic uterine inertia.
- Retained placenta
- Postpartum hemorrhage
Diagnosis Methods
The diagnosis of hypertonic uterine inertia is typically done through tocography, which measures uterine contractions. Additionally, a thorough examination is conducted to detect any abnormalities that may be contributing to the condition. These diagnostic methods help healthcare professionals assess the severity of the condition and determine the most suitable treatment options.
- Tocography is used to measure uterine contractions
- Thorough examination to detect abnormalities
- Help professionals assess severity and determine treatment options
“The diagnosis of hypertonic uterine inertia is typically done through tocography, which measures uterine contractions. Additionally, a thorough examination is conducted to detect any abnormalities that may be contributing to the condition.”
Management Strategies
The management of hypertonic uterine inertia may involve various strategies depending on the individual case. Proper management of the first stage of labor is crucial, and prophylactic antibiotics may be administered if the labor is prolonged. Amniotomy, the artificial rupture of membranes, can be performed to stimulate contractions. Additionally, the use of oxytocin, a hormone that stimulates contractions, may be considered to help progress labor. General measures such as analgesics and antispasmodics can provide relief from discomfort and uterine spasms.
Operative Delivery As A Last Resort
In cases where other methods fail or complications arise, operative delivery may be necessary. This can include vaginal delivery using forceps or vacuum extraction, or in more severe cases, a cesarean section. Operative delivery is considered a last resort when all other interventions have been exhausted or when there is a risk to the mother or baby’s health.
More Common In Primigravidae
Hypertonic uterine inertia is a more commonly observed condition in primigravidae, particularly in older individuals. The lack of previous labor experience and the physiological changes associated with first-time pregnancies may contribute to the occurrence of this condition. Therefore, healthcare professionals should be aware of the increased risk in primigravidae and provide appropriate monitoring and management during labor.
Hypertonic uterine inertia is a condition characterized by infrequent, weak, and short-duration uterine contractions that hinder the progress of labor. While the exact causes are still unknown, multiple factors may contribute to its development. Timely diagnosis and appropriate management are essential to prevent complications and ensure a safe delivery for both the mother and baby.
💡
You may need to know these questions about hypertonic uterine inertia
What is hypertonic inertia of the uterus?
Hypertonic inertia of the uterus refers to a condition characterized by abnormally frequent contractions, accompanied by a heightened resting tone in the uterus, leading to extremely painful contractions. This condition can have detrimental effects on both the mother and the fetus. The excessive frequency and intensity of contractions may cause maternal exhaustion, while the resulting high resting tone and increased pain can potentially lead to fetal hypoxia, a condition characterized by inadequate oxygen supply to the fetus. Early recognition and appropriate management of hypertonic inertia are essential to prevent potential complications for both the mother and the unborn child.
What causes hypertonic uterine contraction?
Hypertonic uterine contractions can be triggered by an excessive amount of oxytocin in the body. When oxytocin levels are inappropriately high, the uterus experiences hypertonus, meaning it remains contracted without relaxing between contractions. This condition can lead to fetal distress. As labor advances and the woman’s natural induction mechanisms activate, it may be necessary to lower the concentration of oxytocin to mitigate the risk of hypertonic contractions.
What are the symptoms of a hypertonic uterus?
A hypertonic uterus refers to a condition where the uterine muscles are in a constant state of contraction. This can lead to symptoms such as excessive pain during menstrual cycles, difficulty with fertility, and discomfort during sexual intercourse. It may also cause urinary and bowel issues, including increased frequency and urgency, as well as constipation. Seeking medical attention is vital, as physical therapy has proven to be an effective treatment approach for relieving the symptoms associated with a hypertonic uterus.
How do you treat a hypertonic uterus?
Treating a hypertonic uterus can be challenging, but various approaches can offer relief. Repositioning the patient, using short-acting tocolytics like terbutaline 0.25 mg IV once, and discontinuing the use of oxytocin, if applicable, are initial steps to consider. Additionally, the administration of analgesics can help alleviate discomfort associated with hypertonic uterine dysfunction. However, due to the complexity of the condition, individualized care and close monitoring by healthcare professionals are crucial for effective management.
Reference source
https://jogi.co.in/storage/articles/files/filebase/Archives/1966/dec/1966_691_698_Dec.pdf
https://gpnotebook.com/simplepage.cfm?ID=-200933368
https://www.sciencedirect.com/topics/medicine-and-dentistry/uterine-hypertonia
https://my.clevelandclinic.org/health/diseases/22870-hypertonic-pelvic-floor