In the intricate world of human reproduction, the hypothalamic-pituitary-ovarian axis holds a powerful sway.
Disruption within this delicate system can lead to a myriad of ovulatory disorders, a leading cause of infertility.
From delayed puberty to signs of hypothyroidism, the symptoms are as varied as the causes.
Join us as we delve into the fascinating realm of the HPO axis and explore the potential solutions for these challenging conditions.
hypothalamic-pituitary-ovarian axis
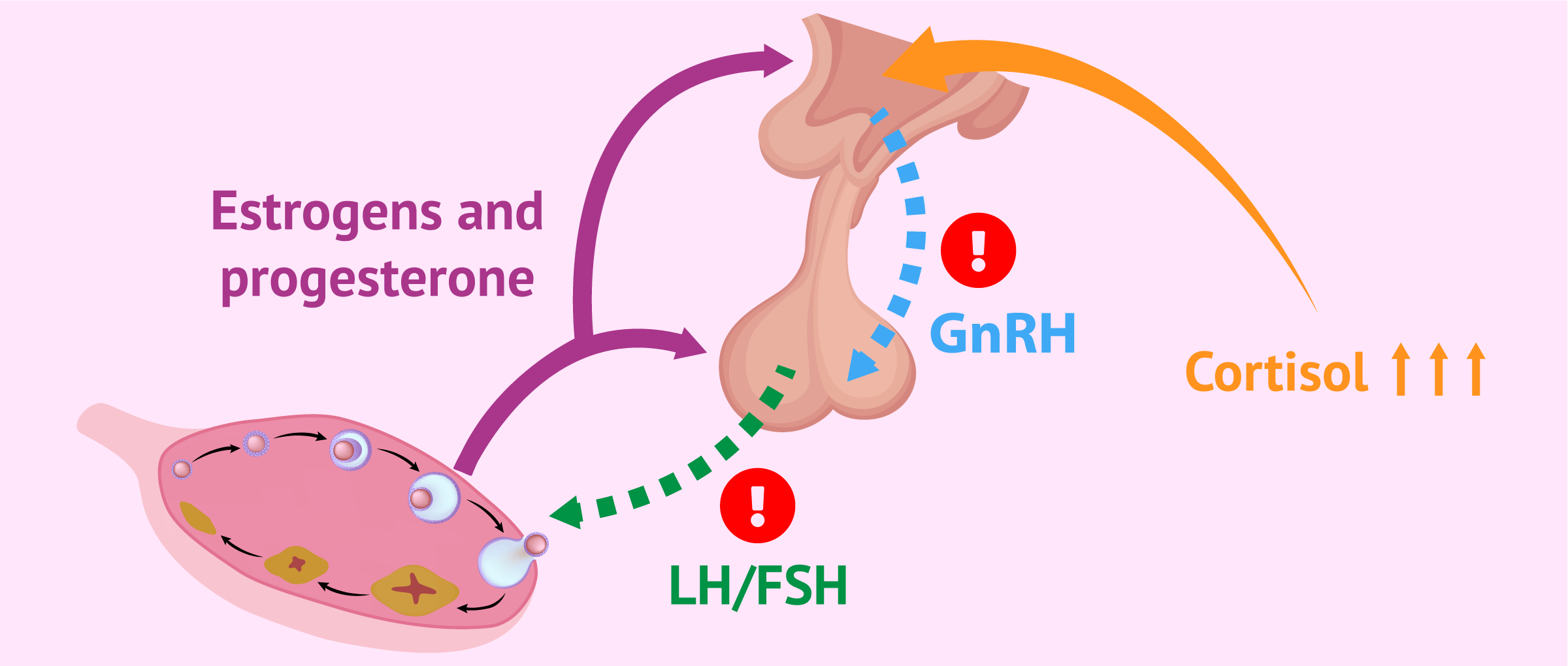
The hypothalamic-pituitary-ovarian (HPO) axis is a coordinated system of communication between the hypothalamus, pituitary gland, and ovaries that regulates reproductive processes.
Ovulatory disorders resulting from HPO axis dysfunction are a common cause of infertility, accounting for 25% of diagnoses.
Three groups of ovulatory disorders resulting from HPO dysfunction have been identified: hypothalamic pituitary failure, eugonadal ovulatory dysfunction, and hypergonadotropic ovulatory dysfunction.
These conditions can be caused by a variety of factors, including genetic mutations, tumors, radiation therapy, and hormonal imbalances.
Symptoms of HPO axis dysfunction include delayed puberty, amenorrhea, infertility, and various other signs related to specific underlying conditions.
Laboratory tests such as the Dutch Cycling Mapping Test and the Sex Hormones panel can be used to evaluate HPO axis dysfunction, along with testing for specific hormones and thyroid function.
Treatment for HPO axis dysfunction focuses on addressing the underlying cause and may include nutritional changes, herbal supplements, lifestyle modifications, and genetic testing in certain cases.
Key Points:
- HPO axis is a system that regulates reproductive processes
- HPO axis dysfunction is a common cause of infertility
- There are three groups of ovulatory disorders resulting from HPO dysfunction
- These conditions can be caused by various factors
- Symptoms include delayed puberty, amenorrhea, infertility, and other signs
- Testing and treatment options are available for HPO axis dysfunction
hypothalamic-pituitary-ovarian axis – Watch Video
💡
Pro Tips:
1. The hypothalamic-pituitary-ovarian axis is a hormonal communication system that plays a crucial role in the regulation of female reproductive functions.
2. The hypothalamus, a small region of the brain, releases gonadotropin-releasing hormone (GnRH) which stimulates the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH) into the bloodstream.
3. FSH stimulates the growth and maturation of the ovarian follicles, which contain the eggs, while LH triggers ovulation and promotes the formation of the corpus luteum.
4. The corpus luteum, a temporary structure that forms in the ovary after the release of an egg, secretes progesterone which prepares the uterus for possible implantation of a fertilized egg.
5. The hypothalamic-pituitary-ovarian axis is tightly regulated, but disruptions such as stress, excessive exercise, or certain medical conditions can lead to irregularities in the menstrual cycle and fertility issues in women.
1. Introduction: Hypothalamic-Pituitary-Ovarian Axis And Its Role In Infertility
Infertility is a deeply challenging and emotionally taxing condition that affects millions of couples worldwide. Among the numerous causes of infertility, ovulatory disorders resulting from hypothalamic-pituitary-ovarian (HPO) axis dysfunction account for a significant proportion. In fact, this dysfunction is the cause of around 25% of infertility diagnoses.
The HPO axis is a precise and synchronized network of communications between the hypothalamus, the pituitary gland, and the ovaries. It plays a vital role in regulating reproductive processes, including ovulation, and any disruption in this delicate balance can lead to ovulatory disorders and subsequent infertility.
2. Understanding HPO Axis: Communication Between Hypothalamus, Pituitary Gland, And Ovaries
The HPO axis functions as a complex feedback system, where the hypothalamus releases gonadotropin-releasing hormone (GnRH) to stimulate the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland. These hormones, in turn, stimulate the ovaries to produce estrogen and progesterone, facilitating follicular development, ovulation, and subsequent preparation of the uterine lining for implantation.
This intricate communication pathway ensures the timely and coordinated release of hormones necessary for successful ovulation and fertility. However, any disruptions or imbalances at any point along this axis can lead to ovulatory disorders and interfere with a woman’s ability to conceive.
3. Ovulatory Disorders: Causes And Impact On Fertility
Ovulatory disorders are characterized by abnormal, irregular, or absent ovulation, which often causes difficulties in fertility. They are a major cause of infertility, highlighting the significance of the HPO axis (hypothalamic-pituitary-ovarian axis) in reproductive health. The causes of ovulatory disorders are multifactorial, encompassing genetic factors and various medical conditions.
Additionally, stress, excessive exercise, and inadequate nutrition can contribute to ovulatory dysfunction. These disruptors can interfere with the release of GnRH (gonadotropin-releasing hormone) from the hypothalamus, hinder the secretion of FSH (follicle-stimulating hormone) and LH (luteinizing hormone) from the pituitary gland, or disrupt the normal development and maturation of ovarian follicles. Ultimately, these disruptions lead to ovulatory disorders.
4. WHO Classification: Categorizing Ovulatory Disorders Resulting From HPO Dysfunction
To better understand and categorize ovulatory disorders resulting from HPO dysfunction, the World Health Organization (WHO) has classified them into three distinct groups:
Group 1, Hypothalamic Pituitary Failure, encompasses conditions such as idiopathic hypogonadotropic hypogonadism (IHH) and various disruptions affecting the hypothalamus or pituitary gland, including gene mutations, acquired panhypopituitarism, intracranial tumors, brain radiation therapy, Langerhans cell histiocytosis, and De Morsier syndrome.
Group 2, Eugonadal Ovulatory Dysfunction, includes ovulatory disorders caused by conditions such as polycystic ovary syndrome (PCOS), obesity, hyperprolactinemia, and primary hypothyroidism.
Group 3, Primary Ovarian Insufficiency or Failure, involves ovulatory disorders resulting from conditions such as Turner Syndrome, FMR1 gene mutation, autoimmune thyroiditis, autoimmune polyglandular syndromes, exposure to environmental toxins, cancer treatments, and menopause.
Understanding these categories helps medical professionals identify the underlying causes of the ovulatory disorders and develop appropriate treatment strategies.
5. Group 1: Hypothalamic Pituitary Failure – Causes And Implications
Within the WHO classification, Group 1 ovulatory disorders arise due to hypothalamic pituitary failure. This group includes idiopathic hypogonadotropic hypogonadism (IHH) and conditions affecting the hypothalamus or pituitary gland.
IHH is characterized by the inadequate production or release of GnRH, which results in insufficient FSH and LH secretion, impairing ovulation.
Various factors can contribute to hypothalamic pituitary failure, including:
- Gene mutations
- Acquired panhypopituitarism
- Intracranial tumors
- Brain radiation therapy
- Langerhans cell histiocytosis
- De Morsier syndrome
Diagnosing and addressing these underlying causes are crucial for effective management and treatment of this group of ovulatory disorders.
6. Group 2: Eugonadal Ovulatory Dysfunction – Factors Contributing To The Disorder
Group 2 ovulatory disorders, known as Eugonadal Ovulatory Dysfunction, encompass various conditions such as polycystic ovary syndrome (PCOS), obesity, hyperprolactinemia, and primary hypothyroidism. These factors have the potential to disturb the hormonal balance within the HPO axis, leading to issues with ovulation.
Polycystic ovary syndrome (PCOS), a common cause of ovulatory dysfunction, is characterized by hormonal imbalances, enlarged ovaries with multiple small cysts, and insulin resistance. It often coexists with obesity and insulin resistance, further exacerbating the disruption of hormone regulation.
Hyperprolactinemia, which involves the excessive production of the prolactin hormone, and primary hypothyroidism, characterized by a deficiency in thyroid hormones, can also disrupt ovulation and fertility by affecting the HPO axis. Recognizing and effectively treating these underlying conditions is crucial for restoring normal ovulatory function.
7. Group 3: Primary Ovarian Insufficiency Or Failure – Conditions And Risk Factors
Group 3 ovulatory disorders, classified as Primary Ovarian Insufficiency or Failure, encompass a range of conditions with varying causes. These conditions include Turner Syndrome, FMR1 gene mutation, autoimmune thyroiditis, autoimmune polyglandular syndromes, exposure to environmental toxins, cancer treatments, and menopause.
Turner Syndrome, a genetic disorder characterized by the absence or partial absence of the X chromosome, often leads to ovarian dysfunction and early menopause. The FMR1 gene mutation, associated with Fragile X syndrome, can also impact ovarian function.
Autoimmune thyroiditis, autoimmune polyglandular syndromes, exposure to environmental toxins, cancer treatments like chemotherapy and radiation therapy, and natural menopause can all contribute to ovulatory disorders by affecting the health and function of the ovaries. Identifying these risk factors and implementing appropriate interventions can help manage and mitigate the impact of these conditions on fertility.
8. Symptoms: Indications Of HPO Axis Dysfunction
Recognizing symptoms of HPO axis dysfunction is crucial for early detection and prompt treatment. Some common symptoms include:
- Delayed puberty
- Amenorrhea (absence of menstruation)
- Signs of hypothyroidism (such as fatigue, weight gain, and cold intolerance)
- PCOS symptoms (including irregular menstrual cycles, excessive hair growth, and acne)
- Insulin resistance
- Central obesity
- Hyperprolactinemia symptoms (such as galactorrhea and irregular menstruation)
- Symptoms associated with Turner Syndrome (such as short stature, webbed neck, and infertility)
It is important to note that these symptoms can vary and may not be present in all cases, making accurate diagnosis and evaluation crucial for effective treatment and management.
9. Laboratory Tests: Assessment Methods For HPO Axis Dysfunction
Accurate diagnosis of HPO axis dysfunction involves a comprehensive evaluation, including laboratory tests. Several tests can aid healthcare professionals in assessing the functioning of the HPO axis and identifying ovulatory disorders.
The Dutch Cycling Mapping Test, a dry urine test, provides valuable insights into hormone metabolite levels throughout the menstrual cycle. Vibrant America’s Sex Hormones panel, a blood test, examines various sex hormones, including FSH, LH, estrogen, and progesterone. The Anti-Mullerian Hormone (AMH) test, also a blood test, assesses ovarian reserve and helps determine the quantity of viable eggs remaining. Additionally, complete thyroid panels can provide information on thyroid function and its impact on the HPO axis.
These tests, when utilized in conjunction with a thorough medical history and physical examination, contribute to a comprehensive evaluation and aid in personalized treatment planning.
10. Treatment Options: Addressing The Root Cause And Management Strategies
Effective treatment and management of HPO axis dysfunction and ovulatory disorders necessitate addressing the underlying causes. Identifying and managing the root cause can optimize ovulatory function and increase the chances of conception.
- Nutrition plays a crucial role in optimizing fertility.
- Following a fertility-based diet and ensuring an adequate calorie intake are essential steps in addressing ovulatory disorders.
- Additionally, specific herbs and supplements, such as Vitex and Tribulus, have shown promising results in supporting hormonal balance and ovulation.
Lifestyle changes, including prioritizing quality sleep and incorporating stress reduction techniques such as acupuncture, can also contribute to restoring the functionality of the HPO axis.
Conventional medicine may employ the GnRH stimulation test to assess the functioning of the HPO axis in certain cases, and genetic testing is indicated in specific instances to identify underlying genetic causes.
In conclusion, understanding the significance of the hypothalamic-pituitary-ovarian (HPO) axis in ovulation and fertility is vital for comprehending ovulatory disorders that contribute to infertility. Categorizing these disorders and identifying their underlying causes through laboratory tests and clinical evaluations can pave the way for personalized treatment strategies focused on addressing the root cause. By optimizing hormonal balance and restoring the functionality of the HPO axis, individuals with ovulatory disorders can increase their chances of conceiving and navigating their reproductive health successfully.
- Nutrition is crucial for optimizing fertility.
- Fertility-based diet and adequate calorie intake are essential for addressing ovulatory disorders.
- Herbs and supplements like Vitex and Tribulus have shown promise in supporting hormonal balance and ovulation.
- Lifestyle changes such as quality sleep and stress reduction techniques, like acupuncture, contribute to restoring HPO axis functionality.
- Conventional medicine may employ the GnRH stimulation test to assess HPO axis functioning in certain cases.
- Genetic testing can identify underlying genetic causes in specific instances.
💡
You may need to know these questions about hypothalamic-pituitary-ovarian axis
What is the ovarian hypothalamic-pituitary axis?
The ovarian hypothalamic-pituitary axis is a vital system in the female reproductive system, encompassing the interaction between the hypothalamus, pituitary gland, and ovaries. It plays a critical role in regulating female fertility and the menstrual cycle. Dysfunction of this axis can lead to ovulation disorders, which the World Health Organization (WHO) classifies into three categories. These categories help to categorize and understand the various ways in which the HPO axis can become imbalanced, providing valuable insight for diagnosis and treatment options for women with reproductive issues.
What does the hypothalamic-pituitary axis do?
The hypothalamic-pituitary axis plays a crucial role in maintaining hormonal balance in the body. By integrating information from various sources such as the upper cortex, autonomic functions, environmental cues, and endocrine feedback, the axis effectively regulates the release of hormones from the pituitary gland. This ensures that the hormonal signals sent out by the pituitary gland have a widespread impact on various endocrine systems, thereby influencing physiological processes throughout the body. Ultimately, the hypothalamic-pituitary axis acts as a master regulator, orchestrating the complex interplay of hormones that are essential for overall bodily function.
What happens when the HPA axis is activated?
When the HPA axis is activated, a cascade of events is triggered to help the body cope with stress. The secretion of glucocorticoids, such as cortisol, helps redirect energy resources to meet the body’s immediate needs. These hormones affect multiple organ systems, including the cardiovascular, immune, and metabolic systems. For instance, they increase heart rate and blood pressure, suppress inflammation and immune responses, and promote the breakdown of stored energy sources like glycogen and fat. Overall, the activation of the HPA axis allows the body to mobilize its resources efficiently and adapt to real or anticipated demands.
What hormone is controlled through hypothalamic-pituitary axis?
Corticotropin-releasing hormone (CRH) is the hormone that is controlled through the hypothalamic-pituitary axis. The paraventricular nucleus of the hypothalamus plays a crucial role in the synthesis and secretion of CRH. This hormone plays a vital role in regulating the body’s response to stress and is involved in the release of cortisol from the adrenal glands. The HPA axis is responsible for maintaining a balanced and appropriate response to stress by controlling the release of CRH and subsequent cortisol production.
Reference source
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6466056/
https://www.uptodate.com/contents/hypothalamic-pituitary-axis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4867107/
https://med.uc.edu/landing-pages/reproductivephysiology/lecture-4/hypothalamic-pituitary-ovarian-axis