Imagine a world where a woman’s dreams of motherhood are shattered by an unexpected diagnosis.
Uterine hypoplasia, a condition often shrouded in mystery, wreaks havoc on reproductive health and causes a myriad of challenges.
From fertility struggles to perplexing menstrual irregularities, this condition leaves no stone unturned.
Delve into the complexities of an infantile uterus and discover the remarkable treatments that may hold the key to unlocking a woman’s hope.
infantile uterus
An infantile uterus refers to a condition called uterine hypoplasia, where the uterus is abnormally small or underdeveloped.
This can lead to fertility issues, menstrual irregularities, and difficulties during pregnancy.
The causes of uterine hypoplasia can include genetic abnormalities, exposure to toxins, hormonal imbalances, infections or inflammations of the uterus, and past surgeries or other conditions.
Symptoms may include abnormal menstrual cycles, infertility, pelvic pain, and abnormalities detected through imaging tests.
Treatment options range from hormonal medications to surrogacy and uterine reconstruction surgery, depending on the individual’s needs.
It is important to consult with a healthcare provider for personalized recommendations based on individual needs and medical history.
Key Points:
- Infantile uterus refers to uterine hypoplasia, where the uterus is underdeveloped or abnormally small.
- It can cause fertility issues, menstrual irregularities, and pregnancy difficulties.
- Causes can include genetic abnormalities, exposure to toxins, hormonal imbalances, infections or inflammations of the uterus, and past surgeries or conditions.
- Symptoms may include abnormal menstrual cycles, infertility, pelvic pain, and abnormalities detected through imaging tests.
- Treatment options include hormonal medications, surrogacy, and uterine reconstruction surgery.
- Consult a healthcare provider for personalized recommendations based on individual needs and medical history.
infantile uterus – Watch Video
💡
Pro Tips:
1. The term “infantile uterus” is used to describe a rare medical condition called “uterus infantilis” in which the uterus remains significantly smaller than normal, often causing fertility issues in women.
2. Although a small uterus is common in infants, uterus infantilis can persist into adulthood. It is estimated to affect approximately 1 in 4,000 women.
3. Uterus infantilis is often diagnosed during adolescence or early adulthood when a woman seeks medical attention for fertility concerns or irregular menstrual cycles.
4. Aside from fertility issues, some women with a small or infantile uterus may experience painful periods (dysmenorrhea) or increased menstrual cramps.
5. Surgical interventions like the “Vidal-Pavone-Oppenheimer” procedure have been developed to increase the size of the infantile uterus, potentially improving fertility outcomes. However, the success of these procedures varies on a case-by-case basis.
Understanding Uterine Hypoplasia: Causes And Symptoms
Uterine hypoplasia is a women’s reproductive health condition characterized by an abnormally small or underdeveloped uterus. This condition can have various implications for fertility, menstrual cycles, and pregnancy. There are multiple possible causes, including genetic abnormalities, exposure to toxins, hormonal imbalances, uterus infections or inflammations, and prior surgeries or medical conditions.
Symptoms of uterine hypoplasia include abnormal menstrual cycles, such as irregular periods, unusually light or heavy bleeding, or even the absence of periods (amenorrhea). Infertility is a common issue due to the underdeveloped uterus’s inability to support proper embryo growth and development. Pelvic pain may also arise from the abnormal structure and size of the uterus. Imaging tests may reveal additional abnormalities, such as a small or misshapen uterus.
Degrees Of Uterine Hypoplasia: Explained
Uterine hypoplasia can be categorized into three degrees based on the severity of the condition:
- First-degree uterine hypoplasia: Mildly underdeveloped uterus, slightly smaller in size and shape than average.
- Second-degree uterine hypoplasia: More noticeable underdevelopment, smaller uterus with possible abnormal shape or structure.
- Third-degree uterine hypoplasia: Most severe form, significantly smaller uterus with deformities that impede proper functioning.
The classification of uterine hypoplasia into different degrees helps determine the appropriate treatment options and prognosis for individuals with this condition. The degree of uterine hypoplasia can guide healthcare providers in making informed decisions regarding:
- Hormonal therapy
- Fertility treatments
- Surgical interventions
These interventions aim to achieve the best possible outcomes for individuals with uterine hypoplasia.
“The classification of uterine hypoplasia into different degrees helps determine the appropriate treatment options and prognosis for individuals with this condition.”
Treatment Options For Hypoplastic Uterus
Treatment for uterine hypoplasia depends on the individual’s specific circumstances, including the severity of the condition and the desired outcomes. Various options are available to address the challenges associated with a hypoplastic uterus. Hormonal medications, such as fertility drugs, may be prescribed to stimulate the growth and development of the uterus. Intrauterine insemination (IUI) or in vitro fertilization (IVF) may be recommended to enhance the chances of conception.
In some cases, surrogacy can be considered when a woman with uterine hypoplasia is unable to carry a pregnancy herself. This involves the use of a gestational surrogate who carries the embryo to term on behalf of the intended parents. Uterine reconstruction surgery is another option, where the structure and size of the uterus are manipulated to improve its functionality. Psychological counseling is often recommended to provide emotional support throughout the treatment journey, as infertility can be a challenging and emotionally taxing experience.
Diagnostic Tests For Uterine Hypoplasia
To diagnose uterine hypoplasia, healthcare providers may conduct several diagnostic tests. Ultrasound imaging is one of the most commonly used techniques to assess the size, shape, and structure of the uterus. It can help identify any abnormalities or underdevelopment. Hysterosalpingography (HSG) is another diagnostic test where a contrast dye is injected into the uterus and X-rays are taken to visualize the uterus and fallopian tubes. Magnetic resonance imaging (MRI) may also be employed to obtain detailed images of the uterus and aid in diagnosis.
These diagnostic tests assist healthcare providers in determining the extent of uterine hypoplasia, guiding them in formulating an appropriate treatment plan and identifying any additional complications or factors that may affect fertility or pregnancy.
Importance Of Consulting A Healthcare Provider
When dealing with conditions such as uterine hypoplasia or a small uterus, it is crucial to seek guidance from a healthcare provider. Only a trained medical professional can accurately diagnose and evaluate the extent of the condition, taking into account the individual’s medical history and specific needs. Consulting with a healthcare provider allows for personalized recommendations and treatment plans tailored to the patient’s unique circumstances.
Additionally, a healthcare provider has the knowledge and expertise to explain the available treatment options, potential risks and benefits, and assist in making informed decisions regarding fertility treatments, hormonal therapy, or surgical interventions. Regular follow-up appointments ensure that the chosen treatment plan is effective and modified if necessary based on the patient’s progress or changing goals.
Benefits of Seeking Guidance from a Healthcare Provider
- Accurate diagnosis and evaluation of condition
- Personalized treatment plans based on individual needs
- Explanation of treatment options, risks, and benefits
- Assistance in making informed decisions
- Regular follow-up appointments for monitoring and modifications to treatment plan
Causes Of A Small Uterus: Genetic Factors And More
A small uterus refers to a uterus that is smaller than the average size. There can be various causes contributing to this condition, including:
- Genetic factors: Genetic abnormalities can significantly impact the development of a small uterus.
- Congenital disorders: Conditions like Asherman’s Syndrome or Turner Syndrome can also contribute to underdevelopment.
Environmental exposures during critical periods of fetal development, such as exposure to certain chemicals or radiation, may affect the growth and development of the uterus, leading to its smaller size.
Individuals with certain health issues, such as hormonal imbalances or previous surgeries involving the uterus, may also be prone to having a small uterus.
Understanding the underlying causes of a small uterus is important in order to determine the most appropriate treatment options.
- Congenital disorders (e.g., Asherman’s Syndrome or Turner Syndrome)
- Genetic abnormalities
- Environmental exposures during fetal development
- Hormonal imbalances
- Previous surgeries involving the uterus
Hormone Therapy For A Small Uterus
For women with a small uterus, hormone therapy is a commonly prescribed treatment option. Hormonal medications can help stimulate the growth and development of the uterus, with the goal of achieving a size that is conducive to conception and maintaining a healthy pregnancy. These medications may include gonadotropins, which are injected to stimulate ovulation and increase the chances of pregnancy.
However, it is important to note that hormone therapy may not be effective for all cases of a small uterus, particularly if the underdevelopment is severe or due to certain genetic or structural abnormalities. Consulting with a healthcare provider is imperative to determine the most appropriate treatment plan based on an individual’s specific circumstances and needs.
Amenorrhea And Investigating Underlying Conditions
Amenorrhea, the absence of menstrual periods, can be associated with a small uterus. This symptom warrants further investigation into underlying conditions that may be contributing to the absence of periods. Through medical examination, imaging tests, and hormonal evaluations, healthcare providers can identify any hormonal imbalances, genetic factors, or structural abnormalities that may be causing amenorrhea.
Treatment options for amenorrhea and underlying conditions depend on the specific diagnosis. Hormonal therapy, surgical interventions, or other targeted treatments may be recommended to address the underlying cause and restore regular menstrual cycles.
Pregnancy Without A Uterus: Gestational Surrogacy
For women with uterine hypoplasia or a small uterus who are unable to carry a pregnancy themselves, gestational surrogacy offers an alternative path to parenthood.
Gestational surrogacy involves using a gestational carrier who carries the embryo for the intended parents.
In this process, the woman’s eggs or a donor’s eggs, along with the partner’s or a donor’s sperm, are fertilized through IVF and then transferred to the surrogacy.
Gestational surrogacy allows individuals or couples to experience the joy of pregnancy and childbirth despite not having a functional uterus. It offers the opportunity to be genetically related to the child while entrusting the gestational carrier to carry the pregnancy to term.
Overcoming Challenges: Successful Pregnancies With A Small Uterus
Having a small uterus can present challenges during pregnancy. However, successful pregnancies can still occur with the right care and fertility treatments. It is crucial to remember the following points:
- Regular prenatal care and monitoring are essential.
- Healthcare providers may develop personalized care plans to address potential complications and support a healthy pregnancy.
- Additional medical interventions, such as frequent ultrasounds, may be necessary.
- Advancements in reproductive medicine and ongoing research offer options for women with uterine hypoplasia or a small uterus.
- Consulting with healthcare providers who specialize in fertility and reproductive medicine is essential.
- Treatment options should be explored based on an individual’s specific circumstances and desires.
Parenthood can be realized with the right support and care, bringing immeasurable joy and fulfillment.
Remember to seek appropriate medical guidance for accurate advice tailored to your situation.
💡
You may need to know these questions about infantile uterus
What causes infantile uterus?
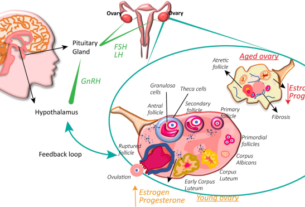
Infantile uterus, also known as hypoplastic uterus, is primarily caused by a combination of genetic and environmental factors. While malnutrition throughout a woman’s lifetime can contribute to the development of infantile uterus, it is one among several possible causes. Other factors, such as malformation of the fetus in the womb, family history, miscarriages that deform the uterus, infections, toxins, or trauma to the uterus, and tumors of the hypothalamus, pituitary gland, or ovaries, can also play a role in the development of this condition. The interplay of these factors can lead to the underdevelopment or incomplete maturation of the uterus during fetal development, resulting in an infantile uterus.
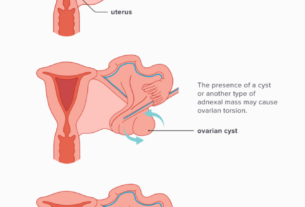
What are the complications of infantile uterus?
Having an infantile uterus can lead to various complications during pregnancy. The underdeveloped uterus can increase the risk of premature birth, where the baby is born before the completion of the full term. Additionally, there is a higher chance of placental abruption, which occurs when the placenta separates from the uterine wall before delivery. Moreover, the abnormal position of the fetus within the uterus can pose difficulties during childbirth. Lastly, the infantile uterus can also increase the likelihood of premature rupture of amniotic fluid, leading to potential complications for both the mother and the baby.
Can you carry a baby to term with a small uterus?
While a small uterus can present potential challenges, it is possible for women to carry a baby to term with a small uterus. It is important for women with this condition to receive regular prenatal care and consult with a fertility expert to assess their specific situation and develop a personalized care plan. With proper monitoring and support, many women with a small uterus have been able to achieve successful pregnancies and have healthy babies.
Can hypoplastic uterus be cured?
There is currently no known cure for hypoplastic uterus. However, treatment options such as hormone therapy, fertility treatments, surgery, and counseling can help manage the symptoms and improve chances of fertility. These interventions aim to address the underlying hormonal imbalances and promote reproductive health, but they cannot fully reverse or eliminate the condition itself. Thus, it is crucial for individuals diagnosed with hypoplastic uterus to work closely with healthcare professionals to explore the most suitable treatment approach for their specific situation.
Reference source
https://pubmed.ncbi.nlm.nih.gov/1193360/
https://www.invitra.com/en/infant-uterus/
https://www.k31.ru/en/baza-statey/infantilnost-gipoplaziya-matki/
https://www.indiaivf.in/blog/small-uterus-treatment-and-understanding/