Pregnancy is often a time of excitement and anticipation, but sometimes, nature takes an unexpected turn.
Meet the invasive mole – a rare and mysterious intruder that can disrupt the joy of pregnancy.
With abnormal cells and water-filled sacs in the womb, this enigma presents challenges in diagnosis and treatment.
Brace yourself for a journey into the realms of gestational trophoblastic disease, where modern medicine battles against odds to preserve the miracle of life.
invasive mole
An invasive mole refers to a form of gestational trophoblastic disease (GTD), specifically choriocarcinoma.
GTD encompasses both cancerous and non-cancerous abnormalities in the cells that form the placenta.
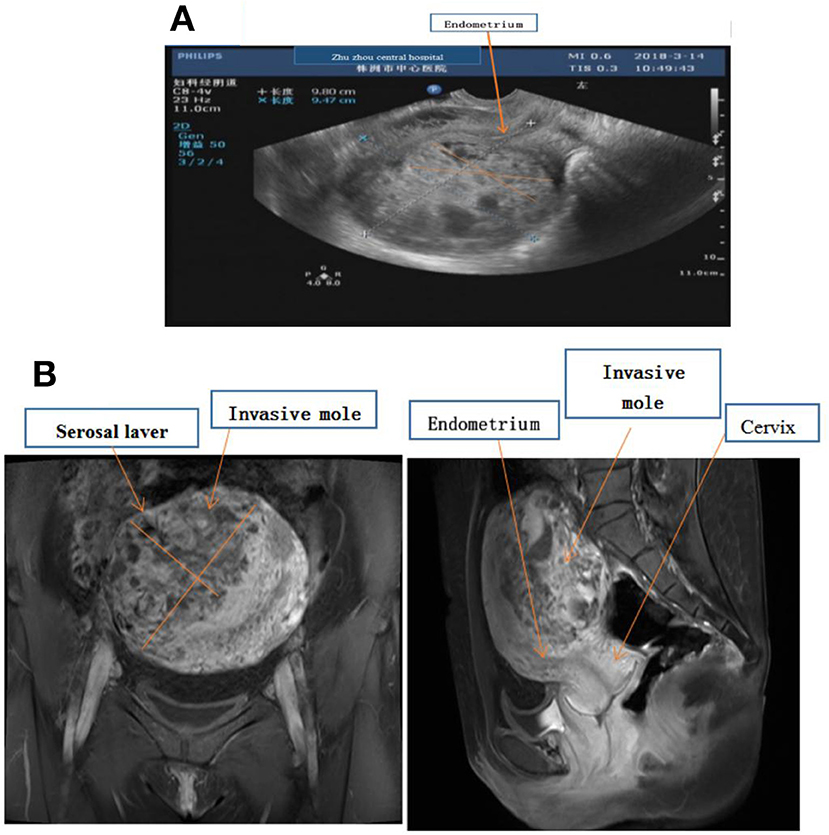
In the case of an invasive mole, abnormal cells form water-filled sacs in the womb.
An invasive mole is often a result of a molar pregnancy, occurring in approximately 1 in 590 pregnancies in the UK and 1 in 50,000 pregnancies overall.
Diagnosing an invasive mole can be challenging, but treatment options typically include chemotherapy and surgical intervention.
It is important to note that the cure rate for invasive moles is generally high.
Key Points:
- Invasive moles are a form of gestational trophoblastic disease (GTD), specifically choriocarcinoma.
- GTD includes cancerous and non-cancerous abnormalities in placental cells.
- Abnormal cells form water-filled sacs in the womb in the case of an invasive mole.
- Invasive moles are often associated with molar pregnancies, occurring in 1 in 590 pregnancies in the UK and 1 in 50,000 pregnancies overall.
- Diagnosis of invasive moles can be challenging, but treatment options typically involve chemotherapy and surgery.
- The cure rate for invasive moles is generally high.
invasive mole – Watch Video
💡
Pro Tips:
1. The invasive mole, also known as the European mole (Talpa europaea), is not actually native to North America. It was introduced to the United States in the 19th century by European settlers.
2. Despite being called an “invasive” mole, this species is not considered invasive in areas where it is introduced. This is because the European mole occupies a similar ecological niche as the native Eastern mole (Scalopus aquaticus) in North America.
3. Invasive moles have an extremely high metabolic rate, which means they need to consume large amounts of food to sustain their energy levels. They can eat up to 50% of their body weight in earthworms and insects every day.
4. The invasive mole is well-known for its digging abilities, as it can dig tunnels at an impressive rate of 15 feet per hour! These extensive tunnel systems help them forage for food, avoid predators, and create nesting burrows.
5. Despite the invasive mole’s underground lifestyle, it has a preference for specific soil types. It tends to avoid acidic soils due to the adverse effects they have on the development of earthworms, which make up a significant part of its diet.
Invasive Mole: Understanding The Basics
Invasive moles, also known as choriocarcinomas, are a rare but serious condition that falls under the category of gestational trophoblastic disease (GTD). They are abnormal cells that develop in the womb, specifically in the form of water-filled sacs. This condition is most commonly associated with molar pregnancies, where a noncancerous tumor forms instead of a fetus.
Invasive moles have a prevalence of 1 in 590 pregnancies in the UK and 1 in 50,000 pregnancies worldwide.
Choriocarcinoma: A Rare But Serious Condition
Choriocarcinoma is a highly malignant tumor that develops from the trophoblast cells, responsible for forming the placenta during pregnancy. This type of cancer can occur in both males and females, although it is more commonly observed in women of reproductive age.
Early detection and treatment are crucial for a positive prognosis as choriocarcinoma can spread rapidly to other organs, including the lungs, liver, and brain.
To summarize:
- Choriocarcinoma is a highly malignant tumor originating from trophoblast cells.
- Both males and females can be affected, but it is more commonly observed in women of reproductive age.
- Early detection and treatment are essential for a favorable outcome.
- This type of cancer can spread rapidly to organs such as the lungs, liver, and brain.
“Choriocarcinoma poses a significant risk due to its aggressive nature and potential for metastasis.”
Gestational Trophoblastic Disease (GTD): Explained
Gestational Trophoblastic Disease (GTD) is a group of conditions that result in abnormal cell growth in the uterus following conception. This includes both cancerous and non-cancerous forms, such as:
- Hydatidiform moles
- Invasive moles
- Choriocarcinomas
- Placental-site trophoblastic tumors
- Epithelioid trophoblastic tumors
While GTD is considered rare, it is crucial to be aware of its different forms for early detection and appropriate treatment.
“Early diagnosis and appropriate treatment are essential in managing Gestational Trophoblastic Disease.”
- GTD encompasses abnormal cell growth in the uterus after conception.
- It includes cancerous and non-cancerous forms.
-
Forms include hydatidiform moles, invasive moles, choriocarcinomas, placental-site trophoblastic tumors, and epithelioid trophoblastic tumors.
-
Gestational Trophoblastic Disease (GTD):
- Abnormal cell growth in the uterus after conception
- Includes cancerous and non-cancerous forms:
- Hydatidiform moles
- Invasive moles
- Choriocarcinomas
- Placental-site trophoblastic tumors
- Epithelioid trophoblastic tumors
- Early diagnosis and appropriate treatment measures are crucial in managing GTD.
Cancerous And Non-Cancerous GTD: Differentiating The Types
One of the critical aspects of GTD is distinguishing between cancerous and non-cancerous forms.
- Non-cancerous GTD, such as hydatidiform moles, typically do not invade the uterine wall or spread to other parts of the body.
On the other hand, cancerous GTD, including choriocarcinomas and invasive moles, have the potential to metastasize and cause significant harm if left untreated.
Therefore, accurate diagnosis and appropriate management strategies become crucial in ensuring the best possible outcomes for patients.
Abnormal Cells: A Key Characteristic Of GTD
At the core of GTD lies the presence of abnormal cells, specifically in the trophoblasts. These cells are responsible for the formation and development of the placenta during pregnancy.
In GTD, these trophoblast cells grow in an uncontrolled and abnormal manner, leading to the various conditions observed within the GTD spectrum.
The identification of these abnormal cells is essential for accurate diagnosis and prompt treatment to prevent further complications.
- Abnormal cells in trophoblasts are the central feature of GTD
- Trophoblast cells are responsible for placenta formation and development during pregnancy
- Uncontrolled and abnormal growth of trophoblast cells characterizes GTD
- Accurate diagnosis and prompt treatment are crucial for preventing complications
“The identification of these abnormal cells is essential for accurate diagnosis and prompt treatment to prevent further complications.”
Water-Filled Sacs: Unusual Growth In The Womb
One of the key features of GTD, particularly invasive moles, is the formation of water-filled sacs within the womb. These sacs are caused by the abnormal overgrowth of trophoblast cells and can lead to a range of symptoms, including:
- Vaginal bleeding
- Abdominal pain
- Enlarged uterus
The presence of these water-filled sacs serves as a vital diagnostic clue in identifying GTD, prompting further evaluation and appropriate treatment interventions.
Note:
When experiencing symptoms such as vaginal bleeding, abdominal pain, or an enlarged uterus, it is important to seek medical attention for proper evaluation and possible treatment.
- Bullet point 1
- Bullet point 2
- Bullet point 3
Molar Pregnancy: An Overview Of This Condition
Molar pregnancy, also known as hydatidiform mole, is a condition in which a noncancerous tumor develops in the uterus instead of a normal fetus. This occurs due to an abnormal fertilization process, resulting in a mass of abnormal cells. Molar pregnancies can be categorized as either complete or partial, depending on the presence or absence of a fetal heartbeat and fetal tissue. Early diagnosis and proper management are crucial to prevent complications and the potential progression to more serious forms of GTD, such as invasive moles or choriocarcinomas.
Cure Rate: Promising Outcomes For GTD Patients
Despite the seriousness of GTD, especially in its cancerous forms, there is a high cure rate associated with appropriate treatment. This rate is particularly promising for those diagnosed with choriocarcinoma and invasive mole. With early detection and prompt initiation of chemotherapy, the cure rate can reach up to 90-95%. Regular monitoring and follow-up are essential to ensure that remission is achieved and maintained in GTD patients.
Chemotherapy: An Effective Treatment Option
Chemotherapy is the primary treatment modality used in the management of Gestational Trophoblastic Disease (GTD), which includes choriocarcinomas and invasive moles. Given that these conditions are highly vascular and capable of spreading to other organs, chemotherapy is essential in eliminating the abnormal trophoblast cells and preventing further metastasis. The specific chemotherapy regimen may vary depending on the stage and extent of the disease, but the overall goal remains unchanged: to achieve remission and prevent recurrence.
Choriocarcinoma After Molar Pregnancy: Recognizing The Risk
Choriocarcinoma can develop after a molar pregnancy, increasing the risk of developing choriocarcinomas compared to the general population. Close monitoring and follow-up care are crucial to promptly identify any signs or symptoms of choriocarcinoma after a molar pregnancy. Early diagnosis allows for swift initiation of treatment, optimizing the chances of a positive outcome.
Invasive moles, choriocarcinomas, and other forms of gestational trophoblastic disease are serious conditions that require timely diagnosis and appropriate management. Accurate identification of abnormal cells can lead to high cure rates when treatment options such as chemotherapy and surgery are promptly initiated. Regular monitoring and follow-up care are crucial to ensure remission and prevent recurrence.
By understanding the basics of these conditions and recognizing the associated risks, healthcare professionals and patients can work together to achieve favorable outcomes in their journey towards recovery.
- Recognize risk factors for choriocarcinoma after a molar pregnancy
- Close monitoring and follow-up care after a molar pregnancy
- Prompt initiation of treatment for choriocarcinoma
- Regular monitoring and care to ensure remission and prevent recurrence
💡
You may need to know these questions about invasive mole
What is an invasive mole?
An invasive mole refers to the infiltration of molar tissue, either complete or partial, into the myometrium or uterine vasculature. This condition is characterized by the invasion of edematous villus and proliferative trophoblasts into the myometrium, allowing it to be differentiated from choriocarcinoma.
Is invasive mole cancerous?
Yes, invasive moles can be cancerous. These growths, known as chorioadenoma destruens, can arise from hydatidiform moles but typically do not metastasize beyond the uterus. On the other hand, choriocarcinoma, a tumor that can develop from hydatidiform moles or various pregnancy-related events, including abortions, miscarriages, ectopic pregnancies, or full-term pregnancies, may pose a greater risk of spreading outside of the uterus. Nonetheless, it is essential to consult with a healthcare professional for an accurate diagnosis and appropriate management.
What is the prognosis for invasive moles?
The prognosis for invasive moles is generally favorable, with a high cure rate of nearly 100%. Despite their potential to spread to other parts of the body, invasive moles can be effectively treated through chemotherapy. This treatment approach helps to eliminate the molar tissue and prevent further growth, leading to a positive outcome and overall good prognosis for patients with invasive moles.
How do you treat an invasive mole?
The treatment for an invasive mole typically involves chemotherapy using anticancer drugs. This form of treatment continues until the beta human chorionic gonadotropin (beta-hCG) level returns to normal for at least three weeks after the completion of the treatment. The goal is to eradicate the abnormal cells and ensure there is no recurrence of the conditions associated with invasive mole. Regular monitoring of the beta-hCG levels is crucial to assess the effectiveness of the treatment and to ensure the complete eradication of the neoplasia.
Reference source
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5359859/
https://www.pennmedicine.org/cancer/types-of-cancer/gestational-trophoblastic-disease
https://www.cancerresearchuk.org/about-cancer/gestational-trophoblastic-disease-gtd/invasive-mole-choriocarcinoma/what-is
https://www.cancer.gov/types/gestational-trophoblastic/patient/gtd-treatment-pdq