Imagine a world where you can have complete control over your reproductive choices while simultaneously enjoying a worry-free sex life.
Sounds too good to be true, right?
Enter the IUD – a tiny, but mighty, contraceptive device that has taken the world by storm.
In this article, we delve into the fascinating world of IUDs, exploring their incredible benefits, potential drawbacks, and everything in between.
Brace yourself for a deep dive into the realm of modern contraception.
iud
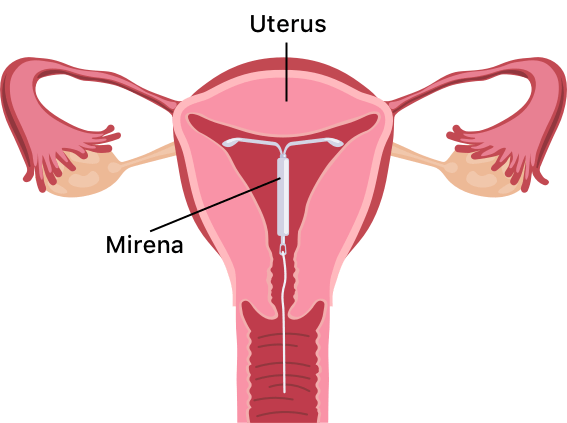
An IUD is a small T-shaped plastic and copper device that is inserted into the uterus to prevent pregnancy.
It is more than 99% effective when inserted correctly.
The IUD releases copper into the womb, making it difficult for sperm to reach an egg and survive.
It can also prevent a fertilized egg from implanting.
The IUD can be left in for 5 to 10 years, depending on the type, and can be inserted at any time during the menstrual cycle as long as the person is not pregnant.
Side effects include potentially heavier, longer, or more painful periods in the first 3 to 6 months, as well as spotting or bleeding between periods.
It does not protect against sexually transmitted infections, so additional methods like condoms may be necessary.
An IUD can be obtained for free from contraception clinics, sexual health or genitourinary medicine clinics, GP surgeries, and some young people’s services.
Contraception services are free and confidential for individuals under the age of 16.
Key Points:
- IUD is a small T-shaped plastic and copper device inserted into the uterus to prevent pregnancy
- It is over 99% effective when inserted correctly
- The IUD releases copper into the womb, making it difficult for sperm to reach an egg and survive, and can prevent a fertilized egg from implanting
- It can be left in for 5 to 10 years, depending on the type, and can be inserted at any time during the menstrual cycle as long as the person is not pregnant
- Side effects include potentially heavier, longer, or more painful periods in the first 3 to 6 months, as well as spotting or bleeding between periods
- IUD does not protect against sexually transmitted infections, so additional methods like condoms may be necessary
iud – Watch Video
https://www.youtube.com/watch?v=ES_JBy-LonY
💡
Pro Tips:
1. The earliest-known use of intrauterine devices (IUDs) dates back to ancient Egypt, around 1850 BC. However, instead of the modern methods, they used papyrus as a material for making IUDs.
2. In the late 19th century, when IUDs were first gaining popularity, the materials used included gold, silver, and even silk thread. Needless to say, the introduction of more modern materials such as rubber and plastic enhanced safety and effectiveness.
3. IUDs have been used not only as a contraceptive method but also as a tool to reduce heavy menstrual bleeding. Hormonal IUDs release progesterone, which can help regulate and lighten menstrual flow.
4. The creator of the first IUD, Dr. Ernst Grafenberg, was a German gynecologist who not only contributed to reproductive healthcare but also had other notable achievements, such as discovering the G-spot.
5. The term “intrauterine device” itself is quite broad and includes a variety of devices. Apart from the well-known T-shaped IUDs, there are also different-shaped IUDs, such as the L-shaped or frameless IUD.
Introduction to IUD: What It Is and How It Works
The intrauterine device (IUD) is a small T-shaped plastic and copper device that is inserted into the uterus to prevent pregnancy. The IUD is a highly effective form of contraception, with a success rate of more than 99% when inserted correctly. It works by releasing copper into the womb, which alters the cervical mucus and makes it difficult for sperm to reach an egg and survive. Additionally, the IUD can prevent a fertilized egg from implanting in the uterus, further preventing pregnancy.
Effectiveness of IUD and How It Prevents Pregnancy
The effectiveness of the IUD is one of its major advantages. When inserted correctly, it is more than 99% effective in preventing pregnancy. Unlike other methods of birth control, such as oral contraceptives or condoms, which rely on consistent and timely use, the IUD provides continuous protection without the need for regular administration. This is particularly beneficial for people who may forget to take a daily pill or use other contraceptive methods inconsistently.
The IUD’s mechanism of action is twofold: it alters the cervical mucus, making it difficult for sperm to reach an egg, and it hampers the implantation of a fertilized egg in the uterus. By creating these barriers, the IUD significantly reduces the chances of pregnancy. It is a reliable and long-term form of contraception that offers peace of mind to individuals seeking to prevent pregnancy without having to remember to take a contraceptive pill every day or interrupt sexual activity by using barrier methods such as condoms.
Mechanism of Action: How IUD Alters Cervical Mucus and Prevents Implantation
The IUD releases copper into the womb, which alters the cervical mucus in two ways. Firstly, it thickens the mucus, making it difficult for sperm to pass through the cervix and reach an egg for fertilization. This effectively reduces the chances of pregnancy. Secondly, the copper has a toxic effect on sperm, inhibiting their motility and viability. This prevents the sperm from reaching the egg in the first place, further enhancing the contraceptive effect of the IUD.
In addition to altering cervical mucus, the IUD can also prevent the implantation of a fertilized egg. If fertilization occurs despite the presence of the IUD, the device’s copper content creates an inhospitable environment in the uterus, making it less likely for the fertilized egg to successfully implant and develop. This dual mechanism of action reinforces the IUD’s efficacy as a highly reliable form of contraception.
Duration of IUD Effectiveness and Types Available
The effectiveness of an IUD depends on the type of device chosen. Some IUDs can be left in place for up to five years, while others can protect against pregnancy for up to ten years. This extended period of contraceptive efficacy makes the IUD an appealing option for individuals who desire long-term birth control without the need for regular maintenance or administration.
There are several types of IUDs available, including those that solely release copper and others that also contain a small amount of progestin. The copper-only IUDs provide effective contraception without introducing hormones into the body, making them a popular choice for individuals who prefer hormone-free birth control. On the other hand, progestin-releasing IUDs not only provide contraceptive benefits but can also help reduce menstrual bleeding and alleviate certain gynecological conditions such as endometriosis.
Timing and Process of IUD Insertion and Removal
The IUD can be inserted at any time during the menstrual cycle, as long as the person is not pregnant. It is a relatively straightforward procedure that can be performed by a trained doctor or nurse. The entire process usually takes around 20 to 30 minutes, with the actual IUD insertion taking only about 5 minutes.
Before inserting the IUD, a healthcare professional will typically:
- Check the position and size of the uterus
- Perform tests for any existing infections
Antibiotics may be provided to prevent infection during the insertion process. Local anesthesia can be used to ensure comfort during the procedure.
The IUD can be removed by a trained doctor or nurse at any time, and pregnancy is immediately possible after its removal. If a person does not wish to get another IUD after removal, it is recommended to use additional contraception for at least 7 days before taking out the existing device.
Side Effects of IUD: Changes in Periods, Spotting, and Bleeding
Like any form of contraception, the IUD may have some side effects. In the first 3 to 6 months after insertion, it is not uncommon for individuals to experience potentially heavier, longer, or more painful periods. Spotting or bleeding between periods is also possible. However, these side effects generally subside over time as the body adjusts to the presence of the IUD.
If discomfort is experienced after insertion, painkillers can be taken to manage any associated cramps or pain. It is important to note that while changes in menstrual flow and timing are common, persistent or severe pain or bleeding should be reported to a healthcare professional. Additionally, any abnormal discharge or other symptoms that may indicate an infection should be promptly addressed.
- Heavier, longer, or more painful periods may occur in the first 3 to 6 months.
- Spotting or bleeding between periods is also possible.
- Painkillers can be taken to manage discomfort after insertion.
- Persistent or severe pain or bleeding should be reported to a healthcare professional.
- Promptly address any abnormal discharge or other symptoms indicating an infection.
“Changes in menstrual flow and timing are common, but persistent or severe pain or bleeding should be reported to a healthcare professional.”
Risks and Potential Complications of Using an IUD
While the IUD is generally safe and well-tolerated, there are some risks and potential complications associated with its use. The main risks include a small chance of pelvic infection within 20 days of insertion, a slightly higher chance of recurring thrush, and the possibility of the IUD being displaced or rejected by the uterus. In rare cases, the IUD can make a hole in the uterus, although this is extremely uncommon.
If a pregnancy occurs despite the presence of an IUD, there is a risk of ectopic pregnancy. This is a serious condition where the fertilized egg implants outside the uterus, usually in the fallopian tube. If symptoms such as pain in the lower abdomen, high temperature, or abnormal discharge are experienced, it is important to seek medical attention promptly.
Considerations for Candidacy: Who Can and Cannot Use an IUD
The IUD is a suitable form of contraception for most people with a uterus. However, there are some considerations to take into account. It may not be suitable for individuals who are currently pregnant, have an untreated sexually transmitted infection (STI), or have certain womb or cervix problems. Those who have had an ectopic pregnancy or have an artificial heart valve should consult with their healthcare provider before getting an IUD.
The IUD can usually be fitted four weeks after giving birth, although alternative contraception should be used until this time. It can also be immediately inserted after an abortion or miscarriage, providing immediate protection against pregnancy. It is worth emphasizing that the IUD does not interfere with breastfeeding and does not affect milk supply.
Post-Insertion Care and Follow-Up Check-Ups
After having an IUD fitted, it is advisable to get the device checked by a healthcare professional after 3 to 6 weeks.
During this check-up, the position of the IUD will be assessed, and any associated concerns or questions can be addressed. If the IUD was successfully placed, this follow-up visit provides reassurance that the device is in the correct position and functioning as intended.
The IUD has two thin threads that hang down from the womb into the vagina. These threads can be checked by the individual to ensure that the IUD is still in place. If the threads cannot be felt or if the IUD has moved, additional contraception should be used, and a healthcare provider should be consulted.
Availability and Access to Free or Confidential IUD Services
The IUD, along with other forms of contraception, can be obtained for free from various healthcare providers. Potential sources for accessing an IUD include:
- Contraception clinics
- Sexual health or genitourinary medicine clinics
- GP surgeries
- Certain young people’s services
These services are typically confidential, ensuring privacy for individuals seeking contraception.
It is important to note that contraception services are both free and confidential for individuals under the age of 16. If a person under 16 wishes to access contraception, healthcare professionals will not inform their parents or carers as long as they believe the individual fully understands the information and decisions being made. Disclosure is only made if there are concerns regarding the individual’s safety or well-being, such as possible abuse or harm.
– Contraception services are available for free from various healthcare providers.
– Potential sources for obtaining an IUD include contraception clinics, sexual health or genitourinary medicine clinics, GP surgeries, and certain young people’s services.
– These services are confidential, ensuring privacy for individuals seeking contraception.
– Individuals under the age of 16 can access contraception services for free and without informing their parents or carers, unless there are safety or well-being concerns.
💡
You may need to know these questions about iud
What are side effects of IUD?
Common side effects of IUDs include spotting between periods, irregular periods, and heavier or longer periods. Additionally, some individuals may experience more or worse cramping during their periods. It is also common to feel pain when the IUD is initially inserted, and some individuals may experience cramping or back aches for a few days afterward.
Is having an IUD painful?
Despite the initial discomfort that may be experienced during the IUD placement process, the level of pain varies depending on the individual. While some individuals report minimal discomfort, others may find the cramping to be more intense. However, the positive aspect is that this discomfort typically subsides within just a couple of minutes. To alleviate any potential discomfort, doctors sometimes recommend taking pain medication prior to the procedure, which can help prevent cramps and make the overall experience more pleasant.
Do you get your period on IUD?
Women who use a hormonal IUD may experience a change in their menstrual cycles. In fact, around 50% of women using this type of IUD will stop getting their periods altogether. However, for some women, their menstrual flow may become irregular and lighter. If you are using a hormonal IUD and experience a prolonged absence of menstruation followed by a sudden resumption, it is advisable to consult with your healthcare provider for further evaluation and guidance.
What is a major disadvantage of IUD?
While IUDs offer a range of advantages, a major disadvantage is the potential for menorrhagia, dysmenorrhea, and polymenorrhea. These issues, which involve heavy, painful, and frequent periods, are often reported by users and can lead to the discontinuation of IUD usage. Additionally, it is important to note that IUDs do not provide protection against sexually transmitted infections (STIs), which is another significant drawback to consider.
Reference source
https://www.nhs.uk/conditions/contraception/iud-coil/
https://www.plannedparenthood.org/learn/birth-control/iud
https://www.plannedparenthood.org/learn/birth-control/iud/iud-side-effects
https://www.plannedparenthood.org/learn/birth-control/iud/whats-an-iud-insertion-like