Left Occipitoanterior: A Guide to Fetal Positioning and Birth
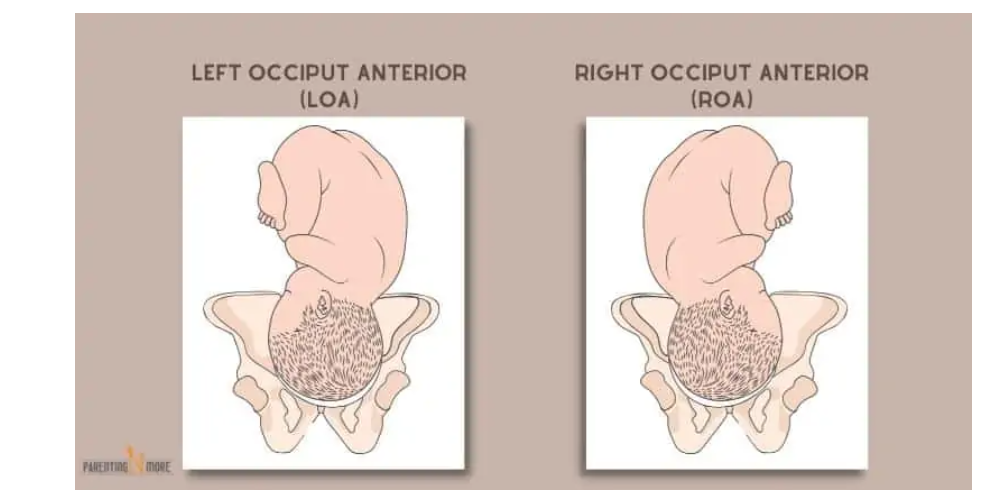
– LOA: Left Occiput Anterior. Occiput (back of the baby’s head) is on the left side of the pelvis, baby’s back is closest to the mother’s belly.
– LOP: Left Occiput Posterior. Occiput is on the left side of the pelvis, baby’s back is closest to the mother’s spine.
– LOT: Left Occiput Transverse. Occiput is on the left side of the pelvis, baby’s back is on the left side of the mother’s body.
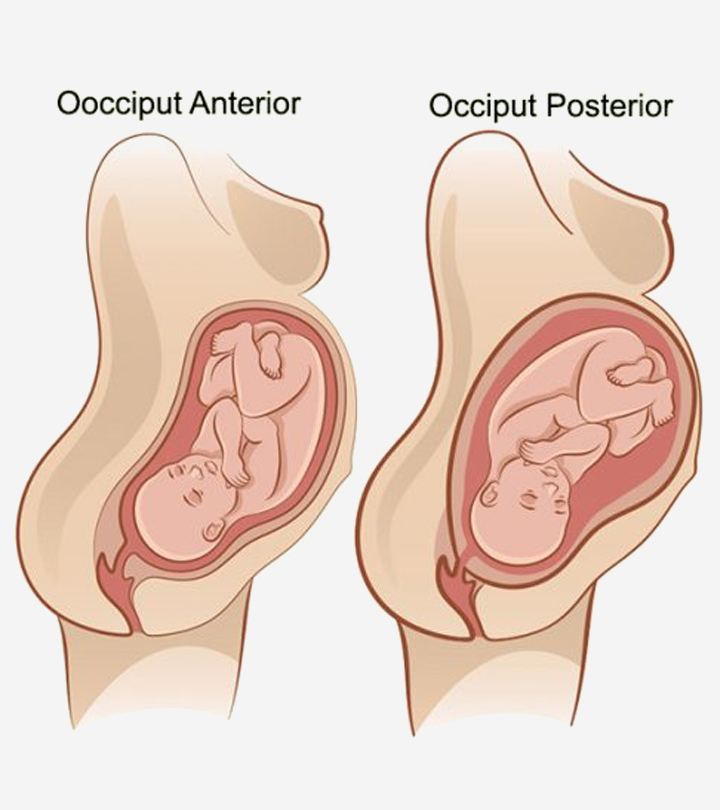
– OA: Occiput Anterior. Occiput is in the central portion of the pelvis, baby’s back is lined up directly central on the mother’s belly.
– OP: Occiput Posterior. Occiput is in the central portion of the pelvis, baby’s back is lined up against mother’s spine.
– RMA: Right Mentum Anterior. Mentum (chin) is on the right side of the pelvis, back is closest to the mom’s belly.
– RMP: Right Mentum Posterior. Mentum is on the right side of the pelvis, back is closest to the mom’s spine.
– RMT: Right Mentum Transverse. Mentum is on the right side of the pelvis, back is on mom’s right side.
– LMA: Left Mentum Anterior. Mentum is on the left side of the pelvis, back is closest to the mom’s belly.
– LMP: Left Mentum Posterior. Mentum is on the left side of the pelvis, back is closest to the mom’s spine.
– LMT: Left Mentum Transverse. Mentum is on the left side of the pelvis, back is on mom’s left side.
– MA: Mentum Anterior. Mentum is in the central portion of the pelvis, back is directly lined up the center of mom’s abdomen.
– MP: Mentum Posterior. Mentum is in the central portion of the pelvis, back is directly lined up against mom’s spine.
– RFA: Right Frontum Anterior. Frontum (forehead) is on the right side of the pelvis, back is closest to mom’s belly.
– RFP: Right Frontum Posterior. Frontum is on the right side of the pelvis, back is closest to mom’s spine.
– Complete Breech: Baby is sitting cross-legged in the pelvis, sacrum is presenting part.
– Frank Breech: Baby is in a pike position with legs extended towards the face, sacrum is presenting part.
– Single or Double Footling Breech: Baby has one or both feet lower in the pelvis than the rest of the body.
– Kneeling Breech: Baby is kneeling, knees enter the pelvis first.
– Right sacrum anterior: Sacrum is on the right side of the pelvis, back is closest to the mother’s belly.
– Right sacrum posterior: Sacrum is on the right side of the pelvis, back is closest to the mother’s spine.
– Right sacrum transverse: Sacrum is on the right side of the pelvis, back is on the mother’s right side.
– Left sacrum anterior: Sacrum is on the left side of the pelvis, back is closest to the mother’s belly.
– Left sacrum posterior: Sacrum is on the left side of the pelvis, back is closest to the mother’s spine.
– Left sacrum transverse: Sacrum is on the left side of the pelvis, back is on the mother’s left side.
– Sacrum anterior: Sacrum is in a central portion of the pelvis, baby’s back is directly in the center of the mother’s abdomen.
– Sacrum posterior: Sacrum is in a central portion of the pelvis, baby’s back is lined up against the mother’s spine.
– Transverse position: Baby’s spine and mother’s spine make a right angle, presenting part is usually the shoulder.
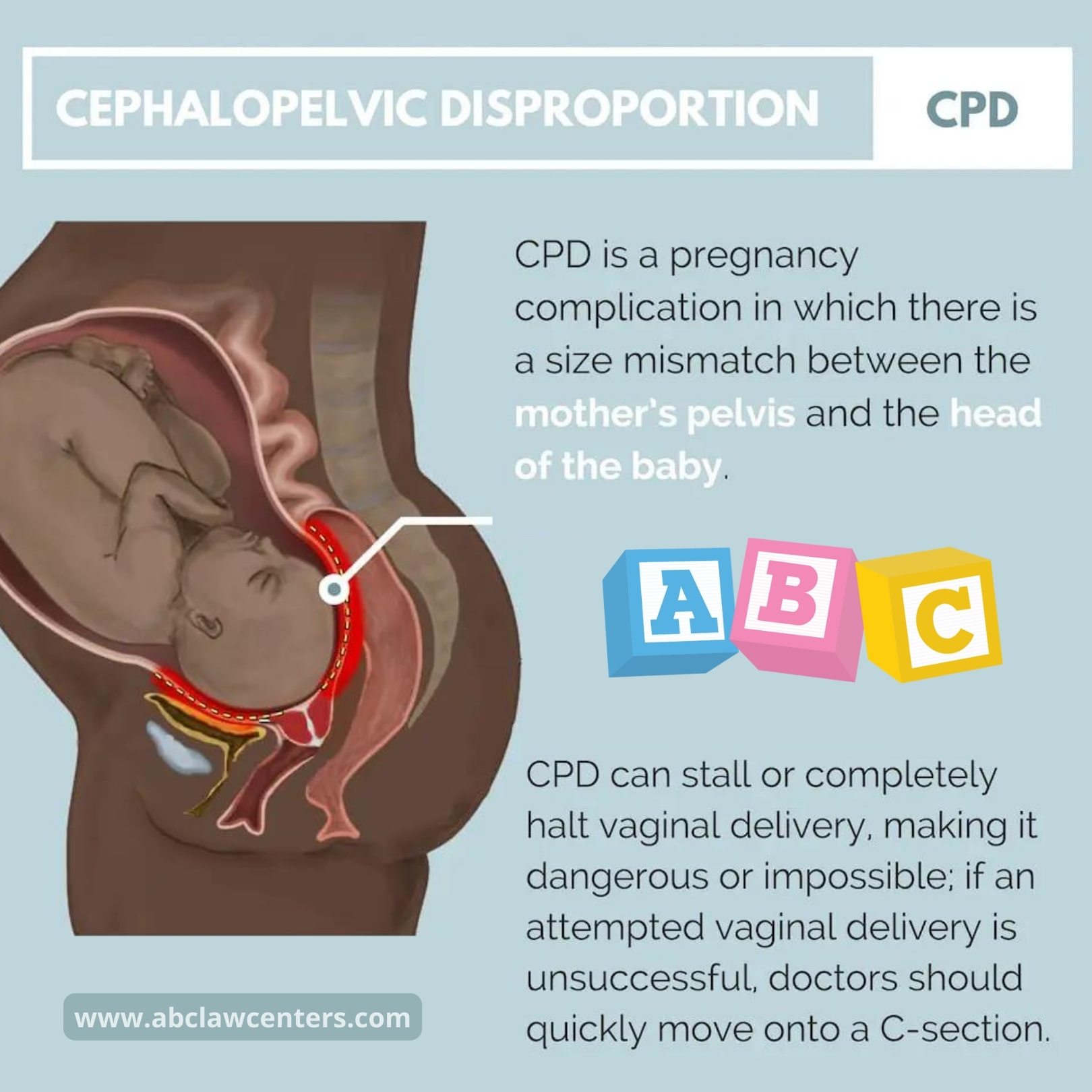
– Optimal position for birth: Baby is head down and anterior, with the back close to the mother’s belly.