Low Forceps Delivery: Reducing Risks and Ensuring Success
– Low forceps delivery is a method used in complicated or prolonged childbirth
– Forceps deliveries can cause serious injuries if done improperly
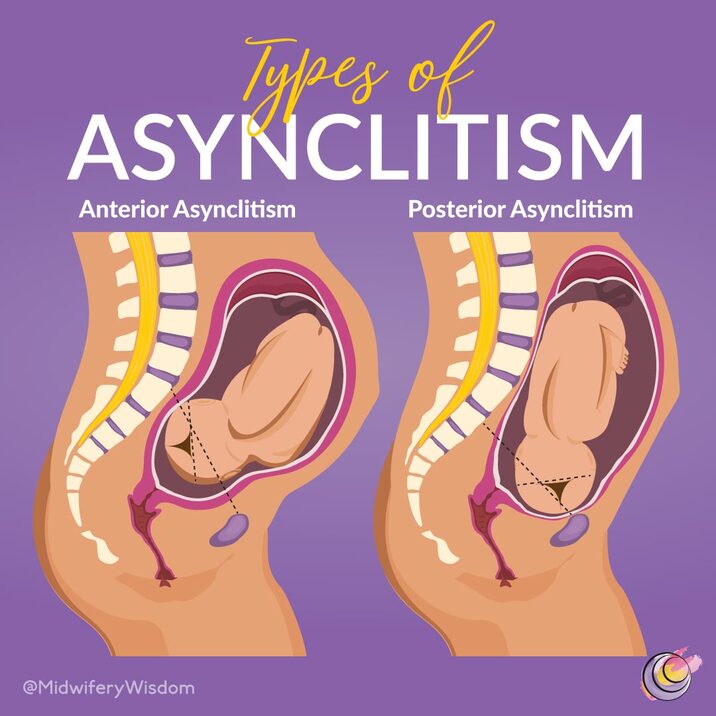
– Forceps are used when a baby is stuck in the birth canal and showing signs of distress
– Low cavity/mid-cavity forceps and rotational forceps are other types of forceps used
– Vacuum extraction is also a common form of assisted delivery, but forceps are associated with less failure
– In 2013, only 3% of children were delivered using forceps or vacuum extraction
– Proper use of forceps is important to avoid complications
– Forceps may cause birth injuries to both the mother and baby
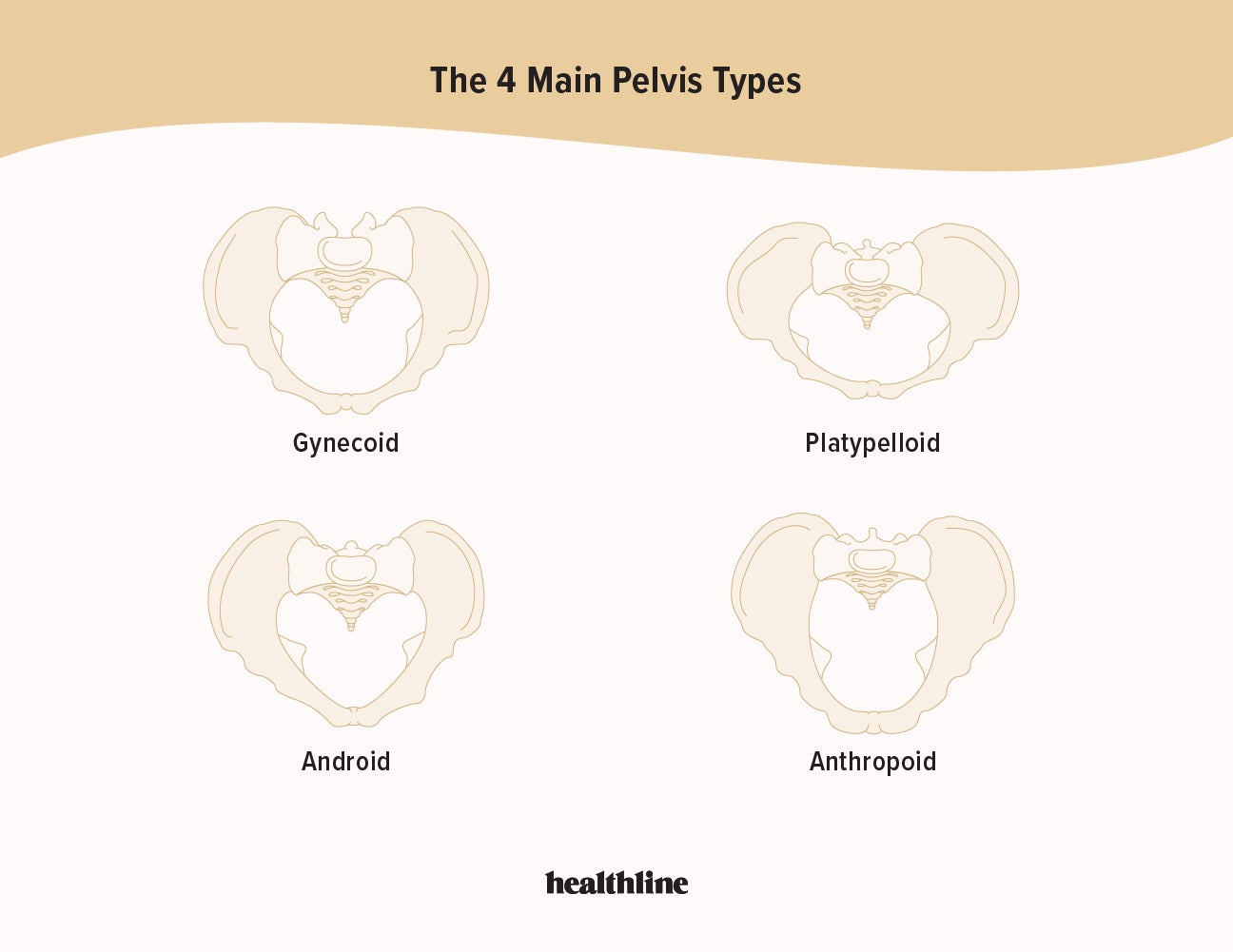
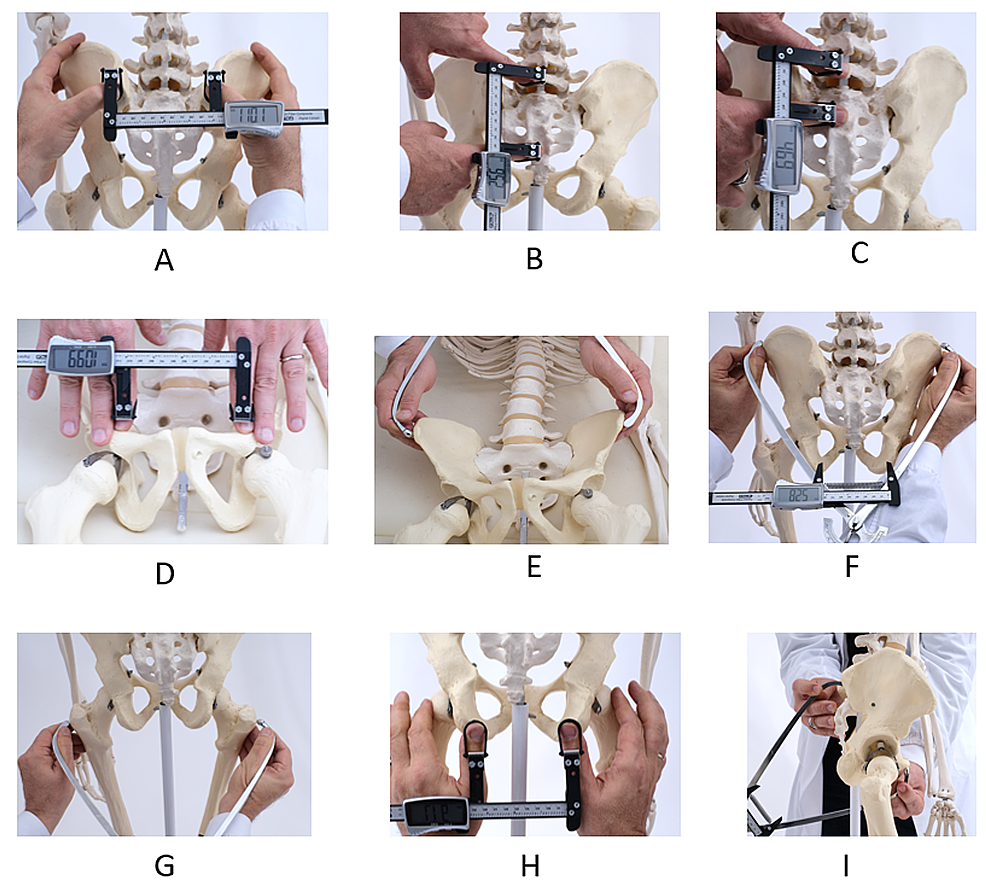
– Forceps delivery should not be used in certain situations, such as when the baby cannot fit through the mother’s pelvis or has a bleeding disorder or weakened bones
– Complications from forceps delivery can cause brain damage, bleeding, jaundice, seizures, fractures, bumps or bruises on the baby’s head, cuts or lacerations on the baby’s face, and facial muscle weakness in the baby
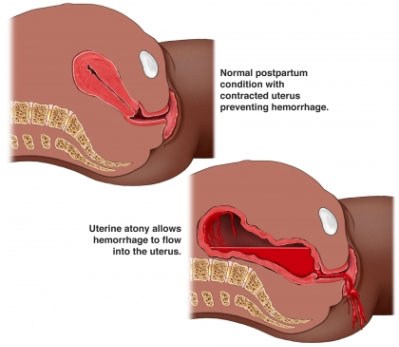
– Maternal birth injuries from forceps delivery are more common and can include blood clots, bladder injuries, incontinence, pain in the perineum, uterine rupture, and vaginal or rectal tears
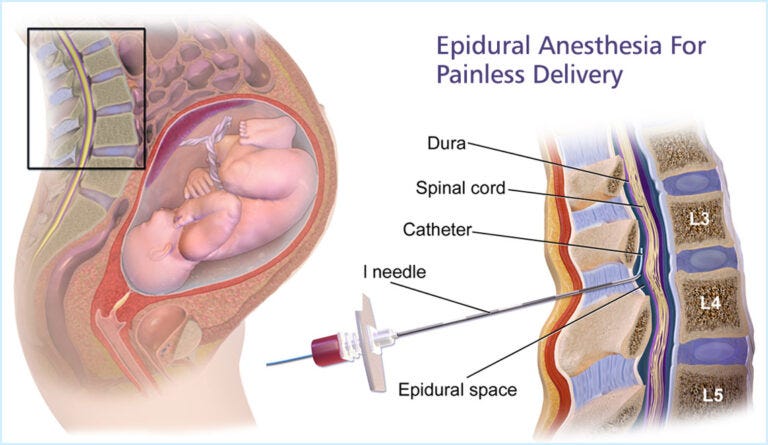
– Doctors may perform an episiotomy (incision between the vagina and anus) during forceps delivery
– Treatment for forceps delivery injuries may include examination for injuries, minor injuries healing on their own, stitches for cuts or tears, catheter insertion for incontinence, and longer healing times or surgery for severe tears
– Many complications from forceps delivery are caused by medical negligence and may be considered medical malpractice
– Those who have experienced a birth injury caused by forceps delivery may be eligible for financial compensation
– The history and development of obstetrical forceps
– Factors that have decreased the use of forceps deliveries in modern obstetrics.