In the world of pregnancy, few words instill both wonder and concern like “macrosomia.” Picture this: A tiny life growing within, yet exceeding expectations by packing on more pounds than the average baby.
But with this growth comes a reality check – complications during delivery and potential health issues awaiting on the other side.
Brace yourself as we delve into the fascinating world of fetal macrosomia.
macrosomia
Macrosomia refers to the condition in which a newborn is considerably larger than the average size.
A baby with fetal macrosomia weighs more than 8 pounds, 13 ounces (4,000 grams), regardless of the duration of gestation.
This condition affects approximately 9% of newborns globally.
However, the risks associated with macrosomia become significantly higher when the birth weight exceeds 9 pounds, 15 ounces (4,500 grams).
Vaginal delivery can be difficult in cases of fetal macrosomia and may put the baby at risk of birth injuries.
Additionally, macrosomia increases the baby’s chances of experiencing health issues after birth.
Key Points:
- Macrosomia refers to newborns who are considerably larger than average size
- Fetal macrosomia is defined as a baby weighing over 8 pounds, 13 ounces, regardless of gestation length
- Approximately 9% of newborns worldwide are affected by macrosomia
- Risks associated with macrosomia increase significantly when birth weight exceeds 9 pounds, 15 ounces
- Vaginal delivery may be difficult and put the baby at risk of birth injuries in cases of fetal macrosomia
- Macrosomia increases the likelihood of health issues for the baby after birth
macrosomia – Watch Video
💡
Pro Tips:
1. Macrosomia, a condition characterized by abnormally large size of a newborn, is more commonly found in babies of mothers with diabetes during pregnancy.
2. The term “macrosomia” comes from the Greek words “makros” meaning large and “soma” meaning body, reflecting the disproportionate size of the affected baby’s body.
3. Although the exact cause of macrosomia is not understood entirely, certain risk factors, such as maternal obesity and excessive weight gain during pregnancy, have been associated with this condition.
4. Babies with macrosomia are more likely to experience birth injuries, such as fractures or nerve damage, due to the challenges posed by their larger size when passing through the birth canal.
5. Although macrosomia can present some challenges during delivery, most infants with this condition can lead healthy lives without long-term complications. However, they may be at an increased risk of developing conditions like obesity and type 2 diabetes later in life.
1. Definition Of Fetal Macrosomia
Fetal macrosomia refers to a newborn who is significantly larger than the average size at birth. It is defined as a baby weighing more than 8 pounds, 13 ounces (4,000 grams), regardless of gestational age. It is typically identified through ultrasound measurements during pregnancy.
Fetal macrosomia can pose risks to both the mother and the baby, making it a condition that needs to be understood and managed effectively.
It is important to note that fetal macrosomia is not a common occurrence, with only about 9% of babies worldwide being born weighing more than 8 pounds, 13 ounces. However, the risks associated with this condition increase significantly when the birth weight surpasses 9 pounds, 15 ounces (4,500 grams).
Some of the risks associated with fetal macrosomia include:
- Difficulties during childbirth: A larger baby may have difficulty passing through the birth canal, increasing the likelihood of birth injuries or the need for a cesarean section.
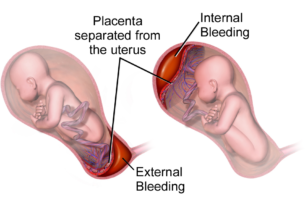
- Shoulder dystocia: This is a condition where the baby’s shoulders get stuck behind the mother’s pubic bone during delivery. It can lead to complications and injuries for both the baby and the mother.
- Increased risk of gestational diabetes: Fetal macrosomia is often linked to gestational diabetes, a condition that affects the mother’s blood sugar levels during pregnancy.
- Birth injuries: The larger size of the baby can increase the risk of injuries during delivery, such as fractures or nerve damage.
In conclusion, fetal macrosomia is a condition where a newborn is larger than average at birth. It is important to be aware of the risks associated with this condition, particularly when the birth weight exceeds 9 pounds, 15 ounces. Effective management and understanding of fetal macrosomia are crucial to ensure the well-being of both the mother and the baby.
2. Weight Criteria For Fetal Macrosomia
The weight criteria for diagnosing fetal macrosomia is set at 8 pounds, 13 ounces, or 4,000 grams. This threshold is used regardless of gestational age, meaning that a baby can be diagnosed with fetal macrosomia even if they are born before their due date. However, it is important to emphasize that fetal macrosomia becomes particularly concerning when birth weight exceeds 9 pounds, 15 ounces (4,500 grams), as the risks for both the baby and the mother increase significantly at this point.
It is noteworthy that the weight criteria for fetal macrosomia may vary slightly depending on regional standards and specific medical guidelines. Health care providers will rely on ultrasound measurements to estimate the size of the baby, taking into account various factors such as the mother’s weight, height, and medical history. These measurements help identify whether the baby may be at risk for fetal macrosomia and inform decisions regarding the best course of action for delivery.
3. Global Prevalence Of Babies With Fetal Macrosomia
Worldwide, approximately 9% of babies are born with a birth weight greater than 8 pounds, 13 ounces, meeting the criteria for fetal macrosomia. This indicates that fetal macrosomia is not a rare condition, although its prevalence may vary among different populations and regions.
The incidence of fetal macrosomia is influenced by several factors, including maternal health, genetics, and lifestyle choices. High rates of gestational diabetes, maternal obesity, and excessive weight gain during pregnancy are known to increase the likelihood of fetal macrosomia. Furthermore, certain ethnicities, such as Hispanic and Asian populations, may have higher rates of the condition compared to others.
Understanding the global prevalence of babies with fetal macrosomia is crucial for healthcare providers in order to provide appropriate care and effectively manage the associated risks.
4. Increased Risks With Higher Birth Weights
As mentioned earlier, the risks associated with fetal macrosomia become more pronounced as birth weight exceeds 9 pounds, 15 ounces (4,500 grams). These risks primarily affect both the baby and the mother, and it is important to address them to ensure a safe delivery and post-birth health.
For the baby, higher birth weight increases the risk of birth injuries, including brachial plexus injuries, where the nerves controlling the arm and hand can be damaged during delivery. The risk of shoulder dystocia, a condition where the baby’s shoulder becomes stuck behind the mother’s pelvic bone during delivery, is also elevated. This can lead to complications, such as fractures or nerve damage. Additionally, babies with fetal macrosomia are at an increased risk of experiencing hypoglycemia (low blood sugar) after birth, as well as respiratory difficulties.
The risks for the mother include an increased likelihood of having a prolonged and difficult labor, which can lead to the need for interventions such as an emergency cesarean section. Vaginal tears and postpartum hemorrhage are also more common in cases of fetal macrosomia. Understanding and managing these risks is crucial to ensure the best possible outcome for both the mother and the baby.
- Fetal macrosomia > 9 pounds, 15 ounces (4,500 grams)
- Risks for Baby:
- Birth injuries (brachial plexus)
- Shoulder dystocia
- Hypoglycemia after birth
- Respiratory difficulties
- Risks for Mother:
- Prolonged and difficult labor
- Emergency cesarean section
- Vaginal tears
- Postpartum hemorrhage
Addressing the risks associated with fetal macrosomia is crucial for a safe delivery and post-birth health.
5. Complications With Vaginal Delivery And Fetal Macrosomia
Vaginal delivery can be complicated by the presence of fetal macrosomia. The larger size of the baby can make it challenging for the baby to pass through the birth canal, leading to an increased risk of prolonged labor and the need for interventions such as vacuum extraction or cesarean section.
Shoulder dystocia, as mentioned earlier, is one of the most significant complications associated with vaginal delivery and fetal macrosomia. It occurs when the baby’s shoulder becomes lodged behind the mother’s pelvic bone, making it difficult for the baby to be born. This condition requires prompt and skilled management by healthcare providers to avoid potential birth injuries.
To minimize the risk of complications during vaginal delivery, healthcare providers may closely monitor the progress of labor and employ strategies such as controlled pushing and different delivery positions. In some cases, they may recommend a cesarean section to ensure a safe and timely birth for both the mother and the baby.
Bullet points:
- Fetal macrosomia can complicate vaginal delivery
- Prolonged labor and interventions like vacuum extraction or cesarean section may be necessary
- Shoulder dystocia is a significant complication associated with fetal macrosomia
- Prompt and skilled management is crucial to avoid birth injuries
- Healthcare providers may monitor labor progress closely
- Controlled pushing and different delivery positions can minimize complications
- Cesarean section may be recommended for a safe and timely birth.
6. Possible Birth Injuries For Babies With Fetal Macrosomia
Babies with fetal macrosomia are at an increased risk of birth injuries compared to those of average size. The size and weight of the baby can put additional strain on the mother’s pelvic structures, potentially leading to birth injuries.
One common birth injury associated with fetal macrosomia is a brachial plexus injury. This occurs when the nerves controlling the arm and hand are damaged during the birthing process. Shoulder dystocia, as mentioned earlier, is a key risk factor for brachial plexus injuries. These injuries may range from mild to severe and can result in temporary or permanent impairment of arm and hand function.
In addition to brachial plexus injuries, babies with fetal macrosomia are also at an increased risk of fractures, particularly in the clavicle (collarbone) and humerus (upper arm bone). These fractures arise from the pressure exerted on the baby’s bones during a difficult delivery. While fractures generally heal well with proper medical care, they can cause temporary pain and discomfort for the baby.
7. Post-Birth Health Problems Linked To Fetal Macrosomia
Fetal macrosomia is a condition that can increase the risk of health problems in newborns. One of the most common issues is hypoglycemia, or low blood sugar levels, which occurs due to the baby’s larger size and increased need for glucose during pregnancy. Close monitoring and appropriate management of blood sugar levels are crucial to prevent complications like seizures or neurological impairment.
Babies with fetal macrosomia are also more likely to experience respiratory difficulties, including respiratory distress syndrome. These challenges may be attributed to the baby’s larger size or other factors associated with the condition. Additional medical support, such as respiratory assistance or oxygen therapy, may be necessary to ensure the baby’s well-being.
Moreover, infants with fetal macrosomia face an increased risk of obesity and metabolic disorders later in life. This emphasizes the importance of long-term monitoring and preventive strategies to address these potential health concerns.
- Hypoglycemia can occur due to the baby’s larger size and increased glucose demands during pregnancy.
- Close monitoring and appropriate management of blood sugar levels are essential.
- Respiratory distress syndrome is more common in babies with fetal macrosomia.
- Additional medical support like respiratory assistance or oxygen therapy may be needed.
- Babies with fetal macrosomia have an increased risk of obesity and metabolic disorders later in life.
8. Factors Contributing To Fetal Macrosomia
Several factors contribute to the development of fetal macrosomia.
Maternal factors such as gestational diabetes, obesity, excessive weight gain during pregnancy, and a history of previous macrosomic births are significant risk factors.
- Gestational diabetes affects the baby’s metabolism and can result in excessive growth.
Genetic factors can also influence the risk of fetal macrosomia. Babies with parents of larger stature may be more prone to being born larger. Additionally, certain ethnicities, such as Hispanic and Asian populations, have higher rates of fetal macrosomia.
Lifestyle choices, such as poor nutrition and lack of physical activity during pregnancy, can also contribute to the development of fetal macrosomia. Smoking and alcohol use during pregnancy have been associated with the condition as well.
Understanding these contributing factors is crucial for healthcare providers to identify high-risk pregnancies and implement appropriate monitoring and management strategies.
- Maternal factors:
- Gestational diabetes
- Obesity
- Excessive weight gain during pregnancy
- History of previous macrosomic births
- Genetic factors:
- Parents of larger stature
- Certain ethnicities (e.g., Hispanic, Asian populations)
- Lifestyle choices:
- Poor nutrition
- Lack of physical activity during pregnancy
- Smoking
- Alcohol use during pregnancy
Now let’s add the blockquote to emphasize the importance of understanding the contributing factors:
“Understanding these contributing factors is crucial for healthcare providers to identify high-risk pregnancies and implement appropriate monitoring and management strategies.”
9. Diagnosis And Management Of Fetal Macrosomia
The diagnosis of fetal macrosomia is typically made through ultrasound measurements that estimate the baby’s size during pregnancy. This can help identify potential risks and guide decisions regarding the mode of delivery. Health care providers will take into account several factors, including the mother’s weight, height, previous pregnancies, and medical history when assessing the risk of fetal macrosomia.
Once fetal macrosomia is diagnosed, a comprehensive management plan will be developed to ensure the best possible outcomes for both the mother and the baby. This plan may involve regular monitoring of blood sugar levels in the mother, dietary adjustments, and, in some cases, a modified delivery approach.
Early discussions with the healthcare team can help address concerns and ensure that appropriate care is provided throughout the pregnancy and delivery process.
10. Preventive Measures For Fetal Macrosomia
While certain risk factors for fetal macrosomia, such as genetic factors, cannot be modified, there are preventive measures that can be taken to reduce the risk and manage the condition effectively.
Maintaining optimal maternal health is crucial. This includes managing gestational diabetes through proper blood sugar monitoring, dietary changes, and, if necessary, insulin therapy. Women who are overweight or obese should aim to achieve a healthy weight before pregnancy and work closely with their healthcare provider to monitor weight gain during pregnancy.
Regular prenatal care visits are essential to monitor the baby’s growth and identify any potential issues early on. Ultrasound measurements can provide valuable information about the baby’s size and help guide decisions regarding the mode of delivery.
Ultimately, prevention and management of fetal macrosomia require a collaborative effort between the healthcare team and the mother. By addressing risk factors early on and implementing appropriate interventions, the likelihood of complications can be minimized, leading to healthier outcomes for both the mother and the baby.
Precautionary measures for fetal macrosomia:
- Maintain optimal maternal health
- Monitor and manage gestational diabetes
- Make dietary changes
- Consider insulin therapy if necessary
- Achieve a healthy weight before pregnancy for overweight or obese women
- Regular prenatal care visits to monitor baby’s growth
- Use ultrasound measurements to guide delivery decisions
In conclusion, fetal macrosomia is a condition characterized by newborns who are significantly larger than average. The risks associated with this condition increase when birth weight exceeds 9 pounds, 15 ounces. Vaginal delivery can be complicated, and babies with fetal macrosomia are at risk of birth injuries and post-birth health problems such as hypoglycemia and respiratory difficulties. Factors contributing to fetal macrosomia include maternal health, genetics, and lifestyle choices. Diagnosis and management involve ultrasound measurements and a comprehensive plan to ensure the best outcome for mother and baby. Preventive measures such as managing gestational diabetes and maintaining optimal maternal health can help reduce the risk of fetal macrosomia. By understanding and addressing the risks and challenges associated with fetal macrosomia, healthcare providers can help ensure safe and healthy pregnancies and deliveries for mothers and their babies.
💡
You may need to know these questions about macrosomia
What is the concern for macrosomia?
The concern for macrosomia lies in the potential complications it can pose for both the mother and the baby. When a fetus weighs over 4000 to 4500 grams (or 9 to 10 pounds), it is considered macrosomic. This condition is linked to a higher risk of maternal and/or fetal trauma during childbirth, as well as neonatal hypoglycemia and respiratory problems. These complications can have serious consequences and thus warrant attention and preventative measures to ensure a safe and healthy delivery for both mother and baby.
Is macrosomia a reason to induce labor?
While macrosomia, the condition of babies being very large, can result in difficult and occasionally traumatic births, inducing labor solely based on the fear of a baby growing too big may not be the most effective solution. Estimating the weight of a baby before birth is challenging and often inaccurate, making it hard to establish an objective basis for inducing labor. Instead, focus should be directed towards continuous monitoring and careful assessment during pregnancy to identify any potential complications and determine if induction is necessary for the well-being of both the mother and the baby.
What is the difference between macrosomia and big baby?
While both macrosomia and big baby refer to larger babies, they differ in the timing of measurement. Big baby generally refers to a baby’s size before birth, specifically those who are large for gestational age. On the other hand, macrosomia is used to describe babies who are larger than the 90th or 95th percentile on an infant growth chart or weigh 4kg or more at birth. Therefore, macrosomia focuses on the baby’s size post-birth, whereas big baby encompasses their size during the gestational period.
Is macrosomia a complication?
Yes, macrosomia is considered a complication during childbirth. Fetal macrosomia, which refers to the birth of a larger-than-average baby, poses potential risks and challenges during delivery. Uncontrolled diabetes and obesity are major factors contributing to macrosomia. It is essential to manage these conditions to minimize the chances of having a large baby and reduce the associated complications.
Reference source
https://www.mayoclinic.org/diseases-conditions/fetal-macrosomia/symptoms-causes/syc-20372579
https://www.uptodate.com/contents/fetal-macrosomia
https://www.cochrane.org/CD000938/PREG_induction-labour-or-near-end-pregnancy-babies-suspected-being-very-large-macrosomia
https://mybabymanual.co.uk/pregnancy/complications/large-for-gestational-age-and-macrosomia/