In the realm of medical mysteries, there are few conditions as perplexing and enigmatic as the malignant hydatidiform mole.
This elusive entity, born from the depths of abnormal fertilization, weaves a tangled web of twisted placental tissue, defying the very essence of a healthy pregnancy.
Join us on a dark journey into the realm of molar pregnancies, where hidden dangers lurk and the stakes could not be higher.
malignant hydatidiform mole
A malignant hydatidiform mole, also known as a molar pregnancy, is a condition characterized by abnormal fertilization of the egg.
It leads to the formation of an abnormal fetus and normal growth of the placenta with little or no fetal tissue growth.
The placental tissue forms a mass in the uterus with a grape-like appearance on ultrasound.
Older women and those with a history of molar pregnancy are at a higher risk of developing this condition.
There are two types of molar pregnancy, partial and complete, depending on the presence or absence of fetal development.
Although there is no known prevention, mortality rate from a hydatidiform mole is essentially zero due to early diagnosis and appropriate treatment.
Approximately 20% of women with a complete mole develop a trophoblastic malignancy, but it is almost 100% curable.
Factors such as advanced maternal age, high levels of hCG, and eclampsia increase the risk of developing malignant disease.
Overall, the risk of adverse outcomes in subsequent pregnancies following a molar pregnancy is similar to that of the general population.
It is important to closely monitor hCG levels and be aware of potential complications such as coagulopathy and respiratory insufficiency.
Key Points:
- Malignant hydatidiform mole is a condition characterized by abnormal fertilization of the egg.
- It leads to the formation of an abnormal fetus and normal growth of the placenta with little or no fetal tissue growth.
- Older women and those with a history of molar pregnancy are at a higher risk of developing this condition.
- There are two types of molar pregnancy, partial and complete, depending on the presence or absence of fetal development.
- Mortality rate from a hydatidiform mole is essentially zero due to early diagnosis and appropriate treatment.
- Factors such as advanced maternal age, high levels of hCG, and eclampsia increase the risk of developing malignant disease.
malignant hydatidiform mole – Watch Video
💡
Pro Tips:
1. Malignant hydatidiform mole is a rare gestational trophoblastic tumor that occurs in the placenta during early pregnancy.
2. Roughly 20% of women with a molar pregnancy will develop malignant hydatidiform mole, which can spread to other organs if left untreated.
3. Malignant hydatidiform mole is characterized by abnormal growth of the placental cells, which form grapelike clusters instead of a healthy placenta.
4. The worldwide incidence of malignant hydatidiform mole is approximately 1 in every 1,500 pregnancies, making it a relatively uncommon condition.
5. One interesting fact about malignant hydatidiform mole is that it can cause high levels of the hormone human chorionic gonadotropin (hCG) to be released, resulting in extreme pregnancy symptoms such as nausea, vomiting, and breast enlargement, even in the absence of a developing fetus.
Introduction To Molar Pregnancy
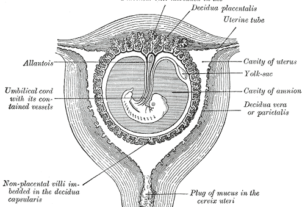
Molar pregnancy, also known as hydatidiform mole (HM) or malignant hydatidiform mole, is a rare condition that occurs due to abnormal fertilization of the egg. This abnormal fertilization leads to the growth of an abnormal fetus and the normal growth of the placenta with little or no fetal tissue development.
One of the hallmarks of molar pregnancy is the formation of a mass in the uterus with a distinctive grape-like appearance on ultrasound, consisting of small cysts within the placental tissue.
Key points:
- Molar pregnancy is more commonly observed in older women, who have a higher chance of developing this condition.
- A history of previous molar pregnancy further increases the risk of experiencing another molar pregnancy.
It is essential to understand the different types of molar pregnancy to comprehend the implications and potential complications associated with this condition.
“Molar pregnancy is a rare condition caused by abnormal fertilization, leading to the growth of an abnormal fetus and a normal placenta. It is more commonly observed in older women and those with a history of previous molar pregnancies.”
- Molar pregnancy is a rare condition caused by abnormal fertilization, leading to the growth of an abnormal fetus and a normal placenta.
- It is more commonly observed in older women and those with a history of previous molar pregnancies.
Types Of Molar Pregnancy
There are two main types of molar pregnancy: partial molar pregnancy and complete molar pregnancy.
- In a partial molar pregnancy, there is an abnormal placenta along with some fetal development. However, this fetal development is typically not viable and does not result in a healthy pregnancy.
- In contrast, a complete molar pregnancy is characterized by an abnormal placenta and the absence of a fetus. This means that no fetal tissue is formed, and the pregnancy is not viable.
Distinguishing between the two types of molar pregnancy is crucial as they have different implications and potential risks.
- Partial molar pregnancies may have a lower risk of complications compared to complete molar pregnancies.
- However, both types require careful management and monitoring to ensure early detection of any potential complications.
Risk Factors For Molar Pregnancy
Several factors can increase the risk of developing a molar pregnancy. These include:
- Advanced maternal age: Older women have a higher likelihood of experiencing abnormal fertilization, which can lead to molar pregnancy.
- Previous history of molar pregnancy: If a woman has had a molar pregnancy in the past, she is at a higher risk of recurrence.
- High levels of human chorionic gonadotropin (hCG): This hormone, produced during pregnancy, can be elevated in women with molar pregnancy.
- Eclampsia: Women with eclampsia, a condition characterized by high blood pressure during pregnancy, are also at an increased risk of molar pregnancy.
- Hyperthyroidism: Having hyperthyroidism, an overactive thyroid gland, can contribute to the risk of molar pregnancy.
- Bilateral theca lutein cysts: The presence of these ovarian cysts, which are associated with excessive hCG levels, can also be a risk factor for molar pregnancy.
It is important to note that these factors do not guarantee the development of a molar pregnancy but rather increase the chances. Regular prenatal care and monitoring can help in the early detection and management of molar pregnancy.
Importance Of Early Diagnosis And Treatment
Early diagnosis and appropriate treatment are crucial in managing molar pregnancy and minimizing potential complications. The mortality rate from hydatidiform mole is essentially zero due to early detection. Regular prenatal care and ultrasound examinations can aid in the early identification of the characteristic grape-like appearance of the molar pregnancy mass in the uterus.
Treatment for molar pregnancy typically involves surgical removal of the abnormal placental tissue through a procedure called suction curettage. Following the procedure, close monitoring and regular hCG testing are necessary to ensure the complete removal of molar tissue and detect any potential complications. In cases where there is a high risk of developing gestational trophoblastic neoplasia, additional chemotherapy may be required.
- Early diagnosis and treatment are crucial in managing molar pregnancy
- Mortality rate is essentially zero due to early detection
- Regular prenatal care and ultrasound examinations are important for early identification
- Treatment involves surgical removal of abnormal tissue through suction curettage
- Close monitoring and hCG testing are necessary after the procedure
- Additional chemotherapy may be required in high-risk cases.
Risk Of Gestational Trophoblastic Neoplasia
Gestational trophoblastic neoplasia (GTN) is a rare complication that can develop in a small percentage of molar pregnancies. Approximately 20% of women with a complete mole may develop GTN, which is almost 100% curable with appropriate treatment.
GTN is characterized by abnormal growth of cells from the trophoblast, the outer layer of cells in the developing embryo.
Several risk factors are associated with the development of GTN, including:
- Advanced maternal age
- High levels of hCG (>100,000 mIU/mL)
- Eclampsia
- Hyperthyroidism
- Presence of bilateral theca lutein cysts.
However, predicting who will develop GTN can be challenging, and regular monitoring of hCG levels is essential to detect the early signs of potential malignancy.
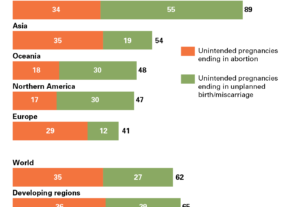
Outcomes Of Subsequent Pregnancies
Women who have experienced molar pregnancies may be concerned about the impact on subsequent pregnancies. Fortunately, studies suggest that the outcomes of subsequent pregnancies in women with a history of molar pregnancy are similar to those in the general population. The incidence of another molar pregnancy is relatively low, occurring in about 1.7% of cases, while stillbirth rates in subsequent pregnancies are around 1.3%. However, careful monitoring and early detection remain crucial to ensuring the well-being of both the mother and the baby.
- The outcomes of subsequent pregnancies in women with a history of molar pregnancy are similar to those in the general population.
- The incidence of another molar pregnancy is relatively low, occurring in about 1.7% of cases.
- Stillbirth rates in subsequent pregnancies are around 1.3%.
“Careful monitoring and early detection remain crucial to ensuring the well-being of both the mother and the baby.”
Increased Risk Of Preterm Birth
Following a molar pregnancy, there is an increased risk of preterm birth, defined as the birth of a baby before 37 weeks of gestation. The reasons for this higher risk are not fully understood, but it is believed that the impact of molar pregnancy on the uterus plays a role. Preterm birth poses challenges for both the baby and the mother, necessitating specialized medical care and monitoring to ensure the best possible outcomes.
Likelihood Of Large-For-Gestational-Age Birth And Stillbirth
In addition to the increased risk of preterm birth, women who have experienced a molar pregnancy may also have a higher likelihood of delivering a baby that is larger than expected for their gestational age. This condition, known as large-for-gestational-age birth, can pose challenges during delivery.
Furthermore, there is a small increased risk of stillbirth in subsequent pregnancies following gestational trophoblastic neoplasia. While the overall risk is relatively low, regular monitoring and close medical attention are necessary during subsequent pregnancies to minimize any potential risks.
Complications During Evacuation Of Molar Pregnancy
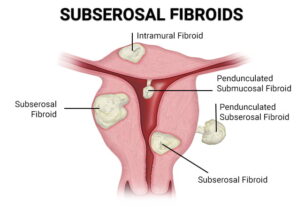
During the surgical evacuation of molar pregnancy, there are potential complications that can arise. Perforation of the uterus is one such complication, which may require laparoscopic guidance to complete the procedure safely. Hemorrhage is another common complication during the evacuation process. Intravenous administration of oxytocin, a hormone that stimulates uterine contractions, should be initiated at the beginning of suctioning to ensure proper hemostasis.
Other medications such as Methergine and Hemabate may also be necessary to control bleeding, and blood for possible transfusion should be readily available. These precautions are taken to prevent excessive blood loss and its associated risks during and after the procedure.
Potential Complications And Risks Of Molar Pregnancy
Aside from the immediate complications during the evacuation of molar pregnancy, there are potential long-term risks and complications associated with this condition. Malignant trophoblastic disease can develop in a subset of molar pregnancies, occurring in approximately 15-20% of complete hydatidiform moles and 2-3% of partial moles. Regular monitoring of hCG levels is essential to detect any signs of malignancy.
Molar tissue releases factors that could trigger the coagulation cascade, leading to disseminated intravascular coagulopathy (DIC), a condition characterized by abnormal blood clotting throughout the body. Additionally, trophoblastic embolism can cause acute respiratory insufficiency, where trophoblastic cells enter the bloodstream and block blood vessels in the lungs. These potential complications highlight the importance of careful monitoring and early detection in the management of molar pregnancy.
💡
You may need to know these questions about malignant hydatidiform mole
Is a hydatidiform mole benign or malignant?
Hydatidiform moles, classified as complete or partial, are generally seen as benign but are actually considered premalignant. Although typically noninvasive, they have the capacity to develop into a malignant and invasive form. While most hydatidiform moles are harmless, it is crucial to monitor them closely as they can potentially progress into a malignant state.
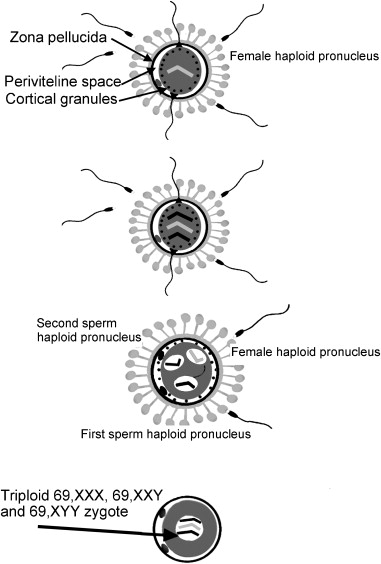
What causes hydatidiform mole?
Hydatidiform mole, also known as molar pregnancy, occurs due to an abnormal fertilization process of the oocyte. In this condition, the fertilized egg develops abnormally, leading to the absence or minimal growth of fetal tissue. However, the placenta grows normally and forms a mass in the uterus. This condition can arise from errors in the chromosomes of either the egg or the sperm, resulting in an imbalanced and nonviable pregnancy.
What is the serious complication of hydatidiform mole?
One significant complication of a hydatidiform mole is the development of an invasive mole, where the abnormal tissue grows deeper into the uterine wall. This can lead to complications such as excessive bleeding and damage to the surrounding organs. However, the most serious complication is the development of a choriocarcinoma, a malignant cancer that can spread to other parts of the body. Choriocarcinoma typically occurs after the hydatidiform mole has been expelled, and early detection and treatment are crucial to prevent its metastasis and potential life-threatening consequences.
Can a molar pregnancy become malignant?
Molar pregnancies are typically benign and pose a low risk of becoming malignant. However, it is essential to ensure that all molar cells are properly removed to minimize the chances of cancerous transformation. If any molar cells remain, there is a small possibility that they could develop into cancerous cells. Although rare, this emphasizes the importance of complete removal and vigilant monitoring to mitigate any potential risks associated with molar pregnancies.
Reference source
https://medlineplus.gov/genetics/condition/recurrent-hydatidiform-mole/
https://www.ncbi.nlm.nih.gov/books/NBK459155/
https://medlineplus.gov/ency/article/000909.htm
https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1111/j.1471-0528.1958.tb09192.x