Discover the remarkable journey of medical oophorectomy, a procedure that holds the power to transform lives.
Delve into the complex world of surgical precision, as one or both ovaries bid farewell, leaving behind a trail of diverse outcomes.
Brace yourself for the twist in the tale: a potential entrance into a new chapter, marked by menopause and unforeseen challenges in fertility.
medical oophorectomy
Medical oophorectomy is a surgical procedure that involves the removal of one or both of the ovaries.
It can be performed as part of a hysterectomy or as an independent procedure.
The reasons for undertaking a medical oophorectomy include tubo-ovarian abscess, ovarian cancer, endometriosis, noncancerous ovarian tumors or cysts, and reducing the risk of ovarian or breast cancer in high-risk individuals.
While it carries certain risks such as bleeding, infection, organ damage, rupture of a tumor, and the retention of ovary cells that cause symptoms, it can offer relief from these conditions.
However, it is important to note that the removal of both ovaries will result in menopause, with associated symptoms such as hot flashes, vaginal dryness, depression, anxiety, heart disease, memory problems, decreased sex drive, and osteoporosis.
Preparing for a medical oophorectomy typically involves fasting, discontinuing certain medications, and undergoing various imaging tests.
It is advisable for individuals who desire to have children to discuss infertility preservation options with their doctor.
Key Points:
- Medical oophorectomy involves removing one or both ovaries, either as part of a hysterectomy or as an independent procedure.
- The procedure is performed for various reasons, including tubo-ovarian abscess, ovarian cancer, endometriosis, noncancerous ovarian tumors or cysts, and reducing the risk of ovarian or breast cancer in high-risk individuals.
- Although it carries risks such as bleeding, infection, and organ damage, it can provide relief from certain conditions.
- Removing both ovaries will result in menopause and its associated symptoms such as hot flashes, depression, and decreased sex drive.
- Preparing for the procedure involves fasting, discontinuing certain medications, and undergoing imaging tests.
- Individuals desiring to have children should discuss infertility preservation options with their doctor.
medical oophorectomy – Watch Video
https://www.youtube.com/watch?v=mUap2-UnDHI
💡
Pro Tips:
1. Oophorectomy, the surgical removal of one or both ovaries, was first performed in the late 19th century as a treatment for various gynecological conditions.
2. The term “oophorectomy” is derived from the Greek words “oophoron” (meaning ovary) and “ektomē” (meaning excision or removal).
3. While oophorectomy is commonly associated with women, it can also be performed on male individuals in cases where testicular cancer has spread to the ovaries.
4. The removal of both ovaries through a bilateral oophorectomy is often recommended as a preventative measure for individuals with a high risk of developing ovarian cancer due to a genetic mutation, such as the BRCA1 or BRCA2 gene.
5. Oophorectomy is sometimes performed as part of gender affirming surgeries for transgender men to support their hormone replacement therapy and align their physical appearance with their gender identity.
Introduction To Medical Oophorectomy
Medical oophorectomy is a surgical procedure that involves the removal of one or both of the ovaries. The ovaries are almond-shaped organs located within the female reproductive system. This procedure can be performed independently or as part of another operation, such as the removal of the uterus. Oophorectomy is typically recommended for various reasons, including the treatment of conditions such as tubo-ovarian abscess, ovarian cancer, endometriosis, noncancerous ovarian tumors or cysts, as well as reducing the risk of ovarian or breast cancer in high-risk individuals.
Reasons For Undergoing Oophorectomy
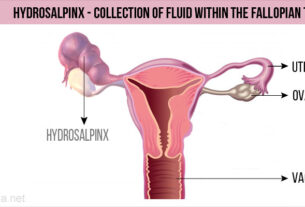
There are several reasons why an individual may choose to undergo an oophorectomy. One common reason is the presence of tubo-ovarian abscess, which is a serious infection involving the fallopian tubes and ovaries. Oophorectomy can help eliminate the infection and prevent further complications. Additionally, individuals diagnosed with ovarian cancer may undergo oophorectomy as part of their treatment plan. For those with endometriosis, a condition where tissue similar to the lining of the uterus grows outside of it, oophorectomy may be recommended to alleviate symptoms and improve quality of life. Noncancerous ovarian tumors or cysts may also require surgical removal through oophorectomy. Lastly, individuals at high risk of developing ovarian or breast cancer due to genetic mutations may opt for preventative oophorectomy to reduce their cancer risk.
Risks And Complications Of Oophorectomy
Oophorectomy, like any surgical procedure, involves risks and potential complications. These may include bleeding, infection, damage to nearby organs, rupture of a tumor during surgery, and the retention of ovary cells that can cause symptoms. It is crucial for patients to have a conversation with their healthcare provider to thoroughly understand these risks and weigh them against the potential benefits of the procedure.
Effects Of Oophorectomy On Menopause
If both ovaries are removed during an oophorectomy, the individual will experience menopause. Menopause is a natural process that marks the end of a woman’s reproductive years, but removing the ovaries induces menopause abruptly. This can lead to various signs and symptoms, including:
- Hot flashes
- Vaginal dryness
- Depression
- Anxiety
- Heart disease
- Memory problems
- Decreased sex drive
- Osteoporosis
It is crucial for individuals who undergo oophorectomy to be aware of these potential effects, as they can have a significant impact on overall quality of life.
Increased Risks Of Early Menopause
Undergoing an oophorectomy at a younger age may increase the risks associated with early menopause. The sudden, premature onset of menopause can have a profound effect on an individual’s physical and emotional well-being. It is important for patients considering oophorectomy to discuss the potential consequences with their healthcare provider and explore the available options for managing menopausal symptoms.
- Oophorectomy at a younger age may increase risks of early menopause.
- Early menopause can have a profound effect on physical and emotional well-being.
- Patients considering oophorectomy should discuss potential consequences with healthcare provider.
Preparing For Oophorectomy
Preparing for an oophorectomy involves several important steps:
-
Fasting: Patients may be required to fast before the surgery to ensure an empty stomach during the procedure.
-
Medication: Certain medications may need to be stopped prior to surgery, as they can interfere with the healing process or increase the risk of complications.
-
Imaging tests: Imaging tests such as ultrasounds and blood tests may be performed to provide a comprehensive assessment of the ovaries and surrounding tissues.
It is crucial for patients to carefully follow their healthcare provider’s instructions to ensure a successful procedure.
Options For Infertility Preservation
For individuals who wish to have children in the future, it is highly recommended to discuss options for infertility preservation with a healthcare provider. Oophorectomy is a procedure that involves the removal of both ovaries and fallopian tubes, and it can have a significant impact on fertility. However, there are still options available for individuals who undergo this procedure.
One such option is in vitro fertilization (IVF). Despite the removal of the ovaries and fallopian tubes, IVF can still be considered as a means of achieving pregnancy. This procedure involves fertilizing an egg with sperm in a laboratory and then transferring the resulting embryo into the uterus.
Another option to consider is egg freezing. This technique allows individuals to preserve viable eggs for future reproductive attempts. By undergoing a process called cryopreservation, the eggs can be stored and used at a later time.
To recap, for individuals concerned about preserving fertility after oophorectomy, it is important to consult with a healthcare provider. Options such as IVF and egg freezing can offer hope for future parenthood.
Improvements:
- Added emphasis using italics and bold
- Clarified the impact of oophorectomy on fertility
- Provided details on IVF and egg freezing as alternative options
- Summarized the importance of consulting with a healthcare provider
Bullet points:
- Oophorectomy may negatively affect fertility
- In vitro fertilization (IVF) can still be considered after oophorectomy
- Egg freezing is an option for preserving viable eggs for future reproductive attempts
Methods Of Performing Oophorectomy
There are two commonly used methods to perform oophorectomy: laparotomy and laparoscopic surgery. Laparotomy involves making a larger incision in the abdomen to access and remove the ovaries. On the other hand, laparoscopic surgery utilizes small incisions and a special instrument called a laparoscope, allowing for a less invasive approach. Both methods involve separating the ovaries from their blood supply and surrounding tissue before removal.
Laparoscopic or robotic oophorectomy is generally associated with quicker recovery, less pain, and a shorter hospital stay compared to laparotomy.
Recovery And Hospital Stay After Oophorectomy
After an oophorectomy, patients will be required to spend time in a recovery room for observation. The length of the hospital stay can range from a few hours to a few days, depending on the individual’s overall health and the specific circumstances of the surgery. Once discharged, most people can resume their normal activities within two to four weeks, but this may vary based on individual factors. It is crucial to adhere to the post-operative care instructions provided by the healthcare team to ensure a smooth recovery.
Different Types Of Oophorectomies And Reasons For Each
There are different types of oophorectomies depending on the specific medical condition or procedure being performed.
- Unilateral oophorectomy involves the removal of one ovary, while bilateral oophorectomy involves the removal of both ovaries.
- Salpingo-oophorectomy is the removal of one ovary and one fallopian tube, while bilateral salpingo-oophorectomy involves the removal of both fallopian tubes and ovaries.
- Hysterectomy with salpingo-oophorectomy entails removing the uterus, one fallopian tube, and one ovary.
- Finally, total hysterectomy with bilateral salpingo-oophorectomy involves the removal of the uterus, cervix, both fallopian tubes, and both ovaries.
Each type of oophorectomy serves a specific purpose in treating different conditions such as endometriosis, benign cysts, preventative surgery for high-risk individuals, ovarian cancer, ovarian torsion, and infections.
In conclusion, oophorectomy is an innovative surgical procedure that empowers women to make informed decisions about their health. It is important for individuals considering oophorectomy to discuss the potential risks, benefits, and implications with their healthcare provider. By understanding the procedure and its effects, individuals can make informed choices regarding their reproductive and overall well-being.
💡
You may need to know these questions about medical oophorectomy
What is medical oophorectomy?
Medical oophorectomy, also known as ovarian removal surgery, is a medical procedure that involves the surgical removal of one or both ovaries. This procedure can be performed using various approaches, such as laparoscopy, vaginal approach, or laparotomy. When both ovaries are removed, it triggers an immediate onset of menopause due to the sudden cessation of hormonal production. Oophorectomy may be recommended in cases of ovarian tumors, certain reproductive system disorders, or as a preventive measure for individuals at high risk of ovarian cancer. By removing the ovaries, this procedure can help alleviate symptoms or reduce the risk of certain medical conditions, but it also leads to the abrupt termination of ovarian hormone production, necessitating hormone replacement therapy to manage menopausal symptoms.
Is an oophorectomy a major surgery?
An oophorectomy can indeed be classified as a major surgical procedure, but this assessment is contingent on specific circumstances and indications. For instance, if the reason behind the removal of the ovary is a considerable tumor or as part of an extensive cancer resection, then it would fall into the realm of major surgery. However, it is important to recognize that the categorization of a surgery as major or minor ultimately hinges upon the underlying factors and context surrounding the procedure.
What happens to your body after oophorectomy?
After oophorectomy, the removal of the ovaries, the body undergoes significant changes. With the sudden depletion of estrogen and progesterone, menopause-like symptoms may arise, including hot flashes and vaginal dryness. Moreover, the hormonal imbalance can exacerbate emotional well-being, potentially leading to feelings of depression or anxiety. Additionally, the absence of these hormones can increase the risk of developing heart disease, emphasizing the importance of maintaining cardiovascular health through lifestyle modifications and appropriate medical interventions.
Why would you need an oophorectomy?
There are various reasons why someone might need an oophorectomy. One of the most common indications is the presence of an ovarian cyst. If the cyst is large, causing pain or discomfort, or if it is suspected to be cancerous, an oophorectomy may be recommended. Additionally, if the ovary becomes twisted, cutting off its blood supply and causing severe pain, surgical removal may be necessary. For individuals with a high risk of developing ovarian cancer, such as those with a family history of the disease or certain genetic mutations, prophylactic oophorectomy may be performed to reduce the risk of developing ovarian cancer in the future.
Reference source
https://my.clevelandclinic.org/health/treatments/17800-oophorectomy
https://www.mdanderson.org/cancerwise/what-to-expect-after-an-oophorectomy–9-questions–answered.h00-159616278.html
https://www.mayoclinic.org/tests-procedures/oophorectomy/about/pac-20385030
https://www.healthdirect.gov.au/surgery/laparoscopic-oophorectomy