Prepare to be intrigued by one of the rarest and most enigmatic medical conditions – myxoma peritonei.
This perplexing syndrome, shrouded in mystery and complexity, has bewildered doctors and researchers alike.
With its origins rooted deep within the abdomen, join me on an extraordinary journey as we unravel the enigma of myxoma peritonei.
myxoma peritonei
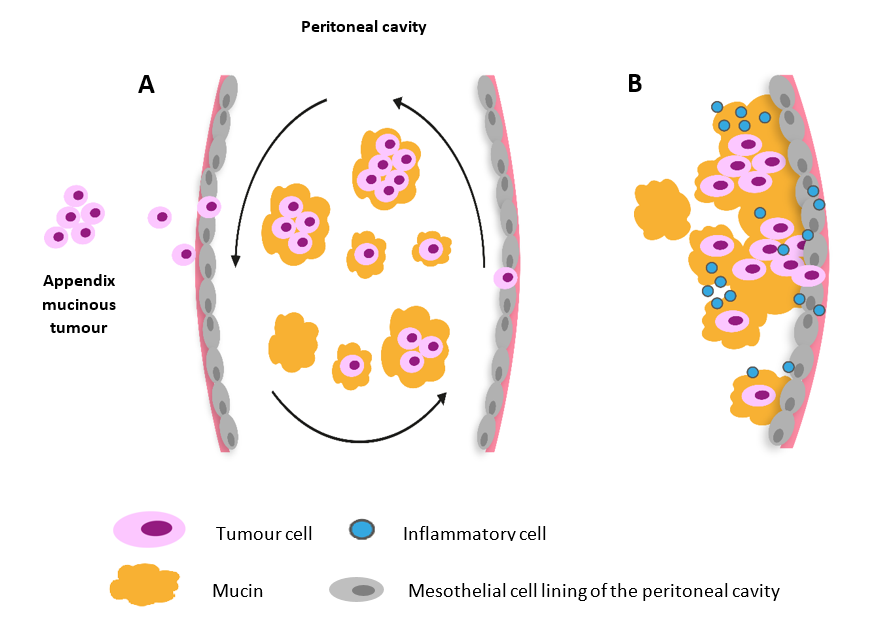
Myxoma peritonei is a rare condition characterized by the presence of mucin-secreting tumors within the peritoneal cavity.
It is often associated with low-grade appendiceal neoplasms, which can rupture and release mucinous material into the abdomen.
The mucin-secreting tumors then proliferate and disseminate throughout the peritoneal cavity, leading to the development of myxoma peritonei.
This condition typically presents with abdominal pain, distension, and a palpable mass.
Treatment usually involves surgical debulking and removal of the mucin-secreting tumors, along with systemic chemotherapy to target any residual cancer cells.
Key Points:
- Myxoma peritonei is a rare condition with mucin-secreting tumors in the peritoneal cavity.
- It is often associated with low-grade appendiceal neoplasms that rupture and release mucinous material.
- The tumors spread throughout the peritoneal cavity, causing the development of myxoma peritonei.
- Symptoms include abdominal pain, distension, and a palpable mass.
- Treatment involves surgical debulking and removal of tumors, along with systemic chemotherapy.
- The goal is to target any remaining cancer cells in the peritoneal cavity.
myxoma peritonei – Watch Video
💡
Pro Tips:
1. Myxoma peritonei is a rare and unusual condition characterized by the growth of mucous-producing tumors within the peritoneal cavity.
2. The term “myxoma peritonei” was first coined by Paul Kucera in 1951 to describe a specific subtype of myxoma originating in the peritoneal cavity.
3. In some instances, myxoma peritonei is associated with a primary tumor known as a “borderline mucinous tumor,” which typically arises in the appendix.
4. The pathogenesis of myxoma peritonei is still not fully understood; however, it is believed to originate from the rupture or seeding of mucinous adenocarcinoma cells into the peritoneal cavity.
5. Researchers have found that myxoma peritonei can lead to a phenomenon called “jelly belly,” where the tumors can grow to such an extent that they fill the entire abdominal cavity, giving it a gelatinous appearance.
Definition Of Myxoma Peritonei
Myxoma peritonei is a rare condition characterized by the presence of mucinous tumor deposits that arise from the lining of the abdominal cavity, known as the peritoneum. The term “myxoma” refers to the gelatinous or mucinous nature of these tumors.
When cells from a primary tumor, usually originating in the appendix, ovary, or colon, spread to the peritoneum and produce excessive mucin, it leads to the development of myxoma peritonei. This condition is often associated with pseudomyxoma peritonei, which is characterized by the accumulation of mucin in the abdominal cavity.
The tumors associated with myxoma peritonei are typically slow-growing and can range in size from small nodules to large masses that occupy a significant portion of the abdominal cavity. The mucinous material produced by these tumors can cause compression and displacement of surrounding organs, leading to various symptoms and complications.
Due to its rarity and the lack of awareness about myxoma peritonei, diagnosis and appropriate management can be challenging.
Causes And Risk Factors Of Myxoma Peritonei
The precise cause of myxoma peritonei is not yet fully understood. However, it is believed to occur as a result of the dissemination of tumor cells from primary appendiceal, ovarian, or colorectal tumors.
In the case of appendiceal tumors, the tumor cells may spread by direct extension or through the lymphatic system, leading to the development of myxoma peritonei. The exact mechanisms by which these tumor cells produce excessive mucin and form mucinous deposits in the peritoneum are still under investigation.
Certain risk factors have been identified that may increase the likelihood of developing myxoma peritonei. These include:
- history of appendiceal or ovarian tumors, especially those with a mucinous component
- family history of myxoma peritonei or other related tumors
It is important to note that while these factors may increase the susceptibility to myxoma peritonei, the development of the condition is still rare.
Signs And Symptoms Of Myxoma Peritonei
The signs and symptoms of myxoma peritonei can vary depending on the size and location of the tumor deposits and the extent of mucinous accumulation in the abdominal cavity.
In some cases, the condition may be asymptomatic, and the tumors are incidentally discovered during imaging studies or surgery for other reasons.
However, when symptoms are present, they may include:
- Abdominal pain or discomfort
- Bloating
- A sense of fullness
- Weight loss
- Changes in bowel habits
As the tumors grow and displace surrounding organs, they can lead to additional complications. These may include:
- Intestinal obstruction
- Urinary symptoms, such as frequent urination or urinary retention
- Compression of blood vessels, resulting in edema or venous thromboembolism
In rare cases, the tumors may rupture, causing acute abdomen and potentially leading to peritonitis.
It is essential to recognize these signs and symptoms to facilitate early detection and appropriate management of myxoma peritonei.
––-*
Diagnosis Of Myxoma Peritonei
The diagnosis of myxoma peritonei involves:
- Clinical evaluation
- Imaging studies
- Pathological examination of tumor samples
Since myxoma peritonei is often associated with primary tumors in the appendix, ovaries, or colon, a thorough medical history and physical examination are crucial in identifying potential sources of metastatic spread to the peritoneum.
Following this, imaging techniques such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) may be employed to visualize and assess the extent of mucinous deposits in the abdominal cavity.
To confirm the diagnosis, a surgical procedure called exploratory laparotomy or laparoscopy may be performed to obtain tissue samples for histopathological analysis.
The collected samples are then evaluated by pathologists who examine the tissue under a microscope to identify the characteristic features of myxoma peritonei, such as the presence of mucinous material and the origin of the tumor cells.
A comprehensive diagnostic approach is necessary for accurate identification and characterization of myxoma peritonei, as this rare condition often requires prompt and appropriate management to optimize patient outcomes.
- Clinical evaluation
- Imaging studies
- Pathological examination of tumor samples
- Thorough medical history and physical examination
- Imaging techniques:
- Ultrasound
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Surgical procedure:
- Exploratory laparotomy or laparoscopy
- Tissue samples for histopathological analysis
- Evaluation by pathologists
- Characteristics of myxoma peritonei:
- Presence of mucinous material
- Origin of tumor cells
Treatment Options For Myxoma Peritonei
The treatment of myxoma peritonei involves a multidisciplinary approach, often including surgical management and additional therapies based on the individual’s specific circumstances. The primary goal of treatment is to remove or reduce the tumor burden in the abdominal cavity, alleviate symptoms, and improve the quality of life for affected individuals.
Surgery plays a central role in the management of myxoma peritonei. The primary surgical intervention is known as cytoreductive surgery (CRS), which aims to remove visible tumor deposits in the peritoneum and other involved organs. This procedure requires a highly skilled surgical team and may involve extensive resection of affected areas, such as the peritoneal lining, appendix, ovaries, or colon. In some cases, the surgery may also include the removal of distant metastases or affected lymph nodes.
During CRS, the surgeons also perform peritonectomy procedures, which involve meticulous stripping or excision of the peritoneal lining to remove tumor deposits. This meticulous approach is necessary to achieve optimal tumor removal while minimizing damage to healthy tissues. Following CRS, individuals may undergo hyperthermic intraperitoneal chemotherapy (HIPEC), which involves the delivery of heated chemotherapy directly into the abdominal cavity. This method helps to eradicate any remaining microscopic tumor cells and prevent disease recurrence.
In certain situations, additional treatment modalities may be recommended to enhance the effectiveness of surgery or manage specific aspects of the disease. These can include systemic chemotherapy, targeted therapy, or radiation therapy, depending on the individual’s overall health, tumor characteristics, and treatment response.
It is important to note that the selection of treatment options for myxoma peritonei should be based on a thorough assessment of the individual condition and multidisciplinary discussions among healthcare professionals. Personalized treatment plans offer the best chance for successful outcomes and improved long-term survival rates.
Surgical Management Of Myxoma Peritonei
The surgical management of myxoma peritonei revolves around the principle of cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) to achieve optimal tumor removal and improve patient outcomes.
CRS is a complex procedure that involves the removal of visible tumor deposits in the peritoneum and affected organs, as well as peritonectomy procedures to remove the mucinous tumor lining.
CRS requires a team of specialized surgeons who have expertise in this highly complex surgical intervention. The procedure begins with a thorough exploration of the abdominal cavity to identify and assess the extent of tumor involvement. The surgeons then proceed with meticulous tumor resection, which involves removing all visible tumor deposits while preserving as much healthy tissue as possible. This can include the resection of the peritoneum, appendix, ovaries, colon, or other affected organs.
During CRS, the surgeons also perform peritonectomy procedures, which involve stripping or excising the peritoneal lining in specific regions. By removing the mucinous tumor lining, the goal is to eliminate any microscopic tumor cells and reduce the risk of disease recurrence. Peritonectomy procedures can be complex and require advanced surgical skills to ensure the complete removal of tumor deposits without damaging critical structures.
Following CRS, HIPEC is often performed to enhance the efficacy of treatment. HIPEC involves the delivery of heated chemotherapy directly into the abdominal cavity, ensuring the maximum exposure of tumor cells to the drugs while minimizing systemic side effects. The heated chemotherapy helps destroy any remaining microscopic tumor cells and offers long-lasting disease control.
The surgical management of myxoma peritonei is highly specialized and demands a multidisciplinary team approach. It requires close collaboration between surgical oncologists, pathologists, radiologists, and other healthcare professionals to provide optimal care and improve patient outcomes.
- A team of specialized surgeons is required for CRS.
- Tumor resection involves removing all visible tumor deposits.
- Peritonectomy procedures involve removing the mucinous tumor lining.
- HIPEC is often performed after CRS to enhance treatment efficacy.
“The surgical management of myxoma peritonei is highly specialized and demands a multidisciplinary team approach.”
Prognosis And Outcomes Of Myxoma Peritonei
The prognosis of myxoma peritonei depends on various factors, including:
Complications Associated With Myxoma Peritonei
Myxoma peritonei, particularly when left untreated or inadequately managed, can lead to various complications.
These complications can arise due to the size and location of the tumor deposits or as a result of the excessive mucin production within the abdominal cavity.
One of the primary complications associated with myxoma peritonei is the compression and displacement of adjacent structures within the abdomen. As the tumors grow, they can put pressure on the intestines, bladder, and blood vessels, leading to symptoms such as abdominal pain, bloating, changes in bowel habits, frequent urination, or urinary retention. In some cases, the compression can result in intestinal obstruction, which manifests as severe abdominal pain, nausea, vomiting, and an inability to pass stools or gas.
The excessive mucin produced by myxoma peritonei can also contribute to the formation of pseudomyxoma peritonei, a condition characterized by the accumulation of mucinous fluid within the abdominal cavity. This can further exacerbate symptoms and lead to increased abdominal distension, discomfort, and a sense of fullness.
Moreover, myxoma peritonei can cause systemic complications, such as venous thromboembolism due to compression of blood vessels or the release of prothrombotic substances by tumor cells. Other potential complications include infection or abscess formation within the abdominal cavity, rupture of tumors leading to peritonitis, and nutritional deficiencies due to malabsorption or obstruction of the digestive tract.
Early detection, appropriate management, and regular monitoring can help minimize the risk of complications associated with myxoma peritonei. Engaging in a comprehensive treatment plan that addresses both the local tumor burden and systemic symptoms can significantly improve patient outcomes and quality of life.
Research Advances In Understanding Myxoma Peritonei
Research in myxoma peritonei is essential to enhance our understanding of this rare condition, improve diagnostic approaches, and explore novel treatment strategies. Although myxoma peritonei is relatively rare, recent advancements in molecular techniques, imaging modalities, and surgical techniques have contributed to better disease management and outcomes.
Researchers are actively investigating the biological mechanisms underlying myxoma peritonei, including the origin and behavior of tumor cells, the processes involved in tumor spread, and the triggering factors for excessive mucin production. By unraveling the genetic and molecular pathways involved in myxoma peritonei development, potential therapeutic targets can be identified.
Advancements in imaging techniques, such as multiphase contrast-enhanced CT or MRI, have improved the ability to visualize and assess the extent of tumor involvement in the peritoneum. This allows for more accurate preoperative planning and facilitates the identification of optimal candidates for surgery. Additionally, novel imaging modalities, such as positron emission tomography (PET) imaging, are being explored to better evaluate tumor biology and monitor treatment response.
Surgical techniques have also advanced, with the refinement of cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). Efforts are being made to streamline and standardize surgical procedures, improve patient selection criteria, and reduce postoperative complications. Additionally, the development of less invasive approaches, such as laparoscopic CRS and robotic-assisted surgery, may provide further benefits in terms of reduced morbidity and shorter recovery times.
Furthermore, ongoing research aims to identify predictive biomarkers that can aid in determining treatment response, disease progression, and prognosis in myxoma peritonei. By identifying specific molecular signatures or genetic abnormalities associated with this condition, personalized treatment approaches can be developed, maximizing the chances of treatment success.
Overall, continued research efforts are crucial to further our understanding of myxoma peritonei, refine treatment strategies, and improve patient outcomes. Collaboration between researchers, healthcare professionals, and patient advocacy groups is essential to drive advancements in this rare disease and provide individuals with myxoma peritonei with the best possible care and support.
Support And Resources For Individuals With Myxoma Peritonei
Having a rare condition like myxoma peritonei can be challenging for individuals and their families, both physically and emotionally. It is important to know that there are support networks and resources available to provide assistance, information, and emotional support throughout the journey.
-
Online communities and patient advocacy groups dedicated to myxoma peritonei can be valuable sources of support and information. These platforms offer opportunities to connect with others who have gone through or are currently undergoing similar experiences, providing a sense of understanding and camaraderie. Additionally, these networks often share updates on current research, treatment options, and medical advancements, ensuring individuals are well-informed and empowered in their healthcare decisions.
-
Medical institutions and hospitals specialized in peritoneal surface malignancies, such as myxoma peritonei and pseudomyxoma peritonei, can provide comprehensive care, including access to experienced healthcare professionals and state-of-the-art treatment facilities. Contacting these institutions or seeking referrals from primary healthcare providers can ensure that individuals receive the most appropriate and specialized care.
-
Support from family, friends, and loved ones is also crucial during this challenging time. Open communication, understanding, and empathy can help alleviate emotional distress and create an environment conducive to healing and recovery.
In conclusion, myxoma peritonei is a rare abdominal tumor characterized by mucinous deposits in the peritoneum, often resulting from the spread of primary tumors. Early diagnosis and appropriate treatment, including cytoreductive surgery and hyperthermic intraperitoneal chemotherapy, can improve patient outcomes and quality of life. Ongoing research is actively exploring various aspects of myxoma peritonei to enhance our understanding of the condition and refine treatment strategies.
- Support networks and resources are available to provide assistance and emotional support for individuals and families dealing with myxoma peritonei.
💡
You may need to know these questions about myxoma peritonei
What is myxoma peritonei?
Myxoma peritonei is a rare and aggressive condition marked by the gradual buildup of mucin-secreting tumor cells in the abdominal and pelvic regions. This condition, also known as pseudomyxoma peritonei, is characterized by the continuous growth and spread of mucinous tumors. It poses significant challenges in diagnosis and treatment due to its rarity and complex nature. Myxoma peritonei requires specialized medical attention and interventions aimed at managing the accumulation of mucus-secreting cells in the affected areas.
Is pseudomyxoma peritonei fatal?
Pseudomyxoma peritonei (PMP) can be a potentially fatal condition if left untreated. While there are different types of PMP, such as the benign Disseminated Peritoneal Adenomucinosis (DPAM), its seriousness should not be underestimated. Without appropriate medical intervention, this condition can have severe consequences, including a potentially deadly outcome. Therefore, early diagnosis and treatment are imperative to ensure the best possible outcome for individuals with PMP.
What causes pseudomyxoma peritonei?
Pseudomyxoma peritonei (PMP) is a condition characterized by the buildup of mucous-like material in the abdominal cavity. Despite extensive research, the exact causes of PMP remain elusive. It is a perplexing condition as there are no identifiable risk factors, and it does not seem to have a familial predisposition. This suggests that PMP might arise from a combination of multiple factors, including genetic and environmental influences, which are yet to be fully understood. Further research is needed to unravel the complex etiology of PMP and shed light on the mechanisms behind its development.
What is the survival rate for pseudomyxoma peritonei?
The survival rate for pseudomyxoma peritonei is relatively high, with a 5-year disease-specific survival probability of 72% in patients classified as adenomucinosis. Pseudomyxoma peritonei itself is a rare disease, occurring in approximately 1 out of every million people annually. While the incidence of this condition is low, the effectiveness of the treatment strategy suggests a favorable prognosis for those diagnosed with pseudomyxoma peritonei.
Reference source
https://rarediseases.org/rare-diseases/pseudomyxoma-peritonei/
https://www.webmd.com/digestive-disorders/pseudomyxoma-peritonei-facts
https://www.cancer.org.au/cancer-information/types-of-cancer/rare-cancers/pseudomyxoma-peritonei
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1867935/