List of Pertinent Information About ‘Asphyxia Pallida’:
1. Asphyxia is defined as a condition with a severe decrease in oxygen concentration in the body and an increase in carbon dioxide concentration.
2. Asphyxia can result in loss of consciousness or death.
3. Causes of asphyxia include choking, drowning, electric shock, injury, and inhaling toxic gases.
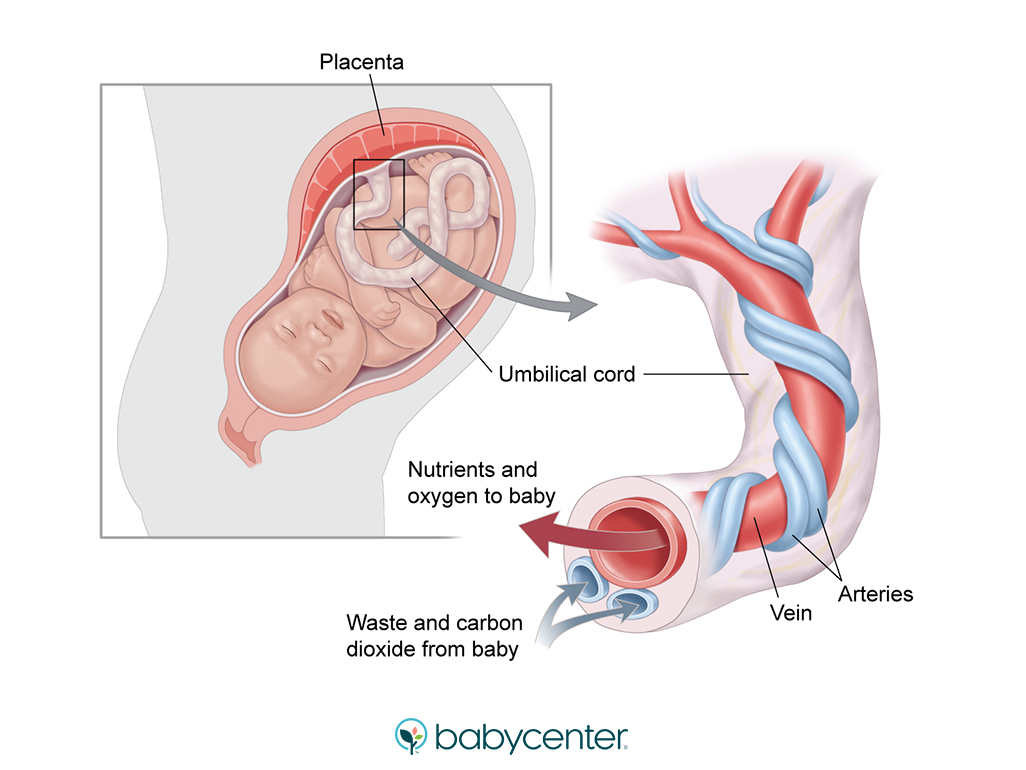
4. Foetal asphyxia refers to inadequate oxygenation and elimination of carbon dioxide in the womb.
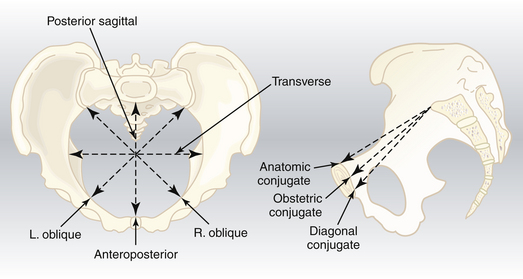
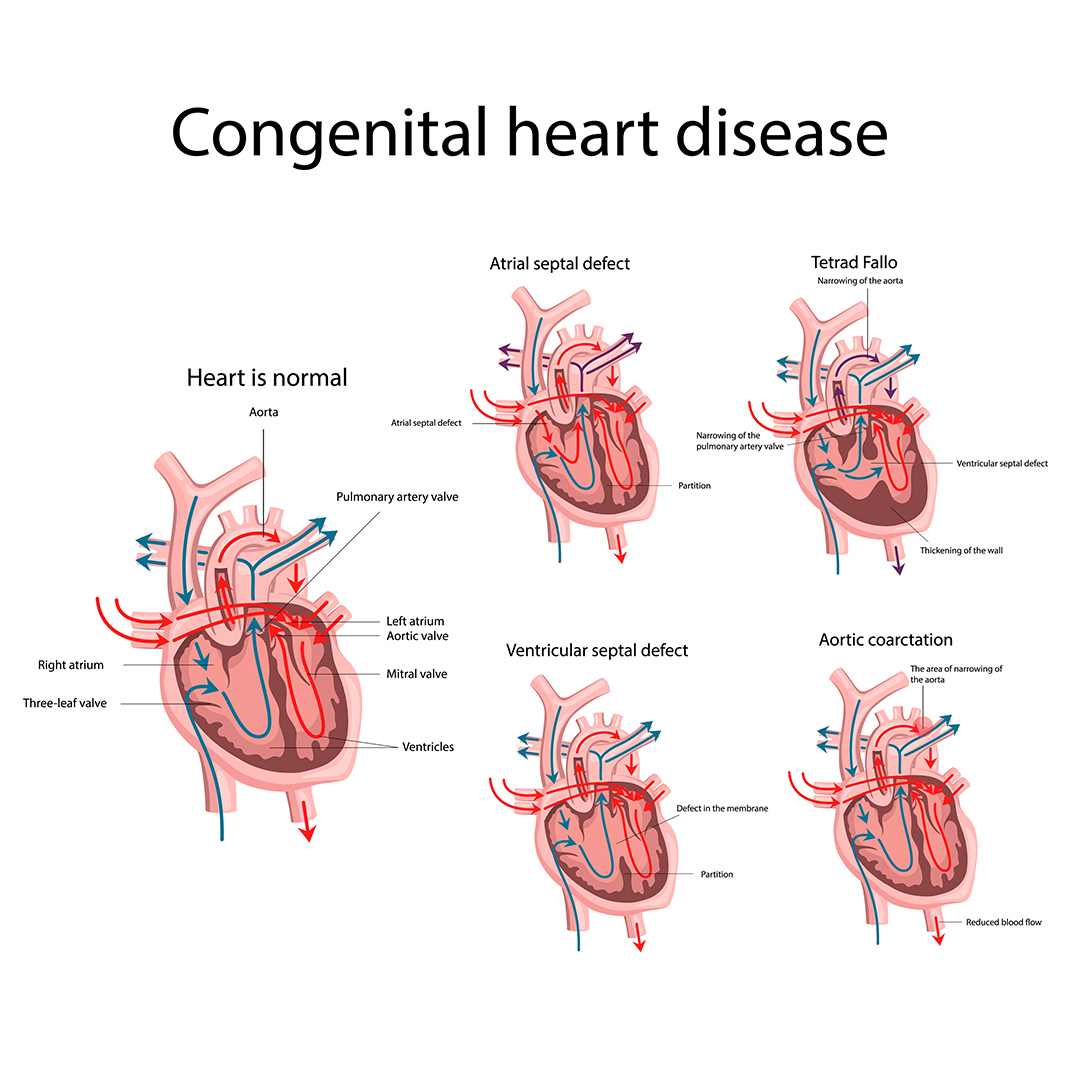
5. Causes of intrauterine asphyxia include maternal factors like cardiac failure, pulmonary diseases, and anaesthetic agents causing hypotension, as well as placental and foetal factors.
6. Signs of foetal distress include changes in foetal heart rate, meconium stained amniotic fluid, foetal acidosis, increased foetal movements, and weak cord pulsation if the cord is prolapsed.
7. Management of foetal distress involves stopping oxytocin, placing the mother in a left lateral position, administering oxygen to the mother, and considering immediate delivery if conservative methods fail.
8. Asphyxia neonatorum can be caused by various factors including respiratory center paralysis or depression, respiratory distress syndrome, and obstructed air passages.
9. Diagnosis of asphyxia is based on clinical features.
10. Asphyxia pallida is a type/stage of asphyxia, with characteristics such as skin color, respiratory efforts, heart rate, muscle tone, reflexes, and prognosis.
11. The Apgar score is used to assess the newborn’s condition and response to resuscitation, evaluating factors such as heart rate, respiratory effort, muscle tone, reflexes, and color.
12. Prophylaxis of asphyxia neonatorum involves proper antenatal care, intranatal monitoring, avoiding specific medications, minimizing exposure to anesthesia during labor, and clearing the air passages of the fetus after delivery.
13. Treatment of asphyxia follows the ABCD arrangement, including airway suctioning, stimulating breathing, mouth-to-mouth breathing, oxygen mask use, endotracheal intubation, cardiac massage, and administration of specific drugs.
14. No links are provided in the article.
Continue Reading