Anovular Menstruation: Causes, Symptoms, and Effective Treatment Options
– Anovular menstruation is when an egg does not come out of the ovary during the menstrual cycle.
– Chronic anovulation is a common cause of infertility.
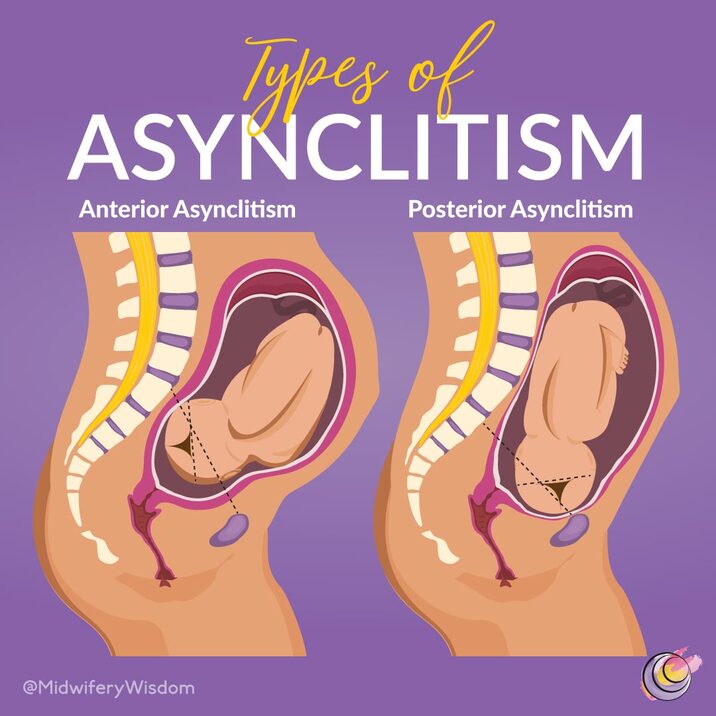
– Ovulation is the release of the egg from the ovary, typically on day 14 of a 28-day menstrual cycle.
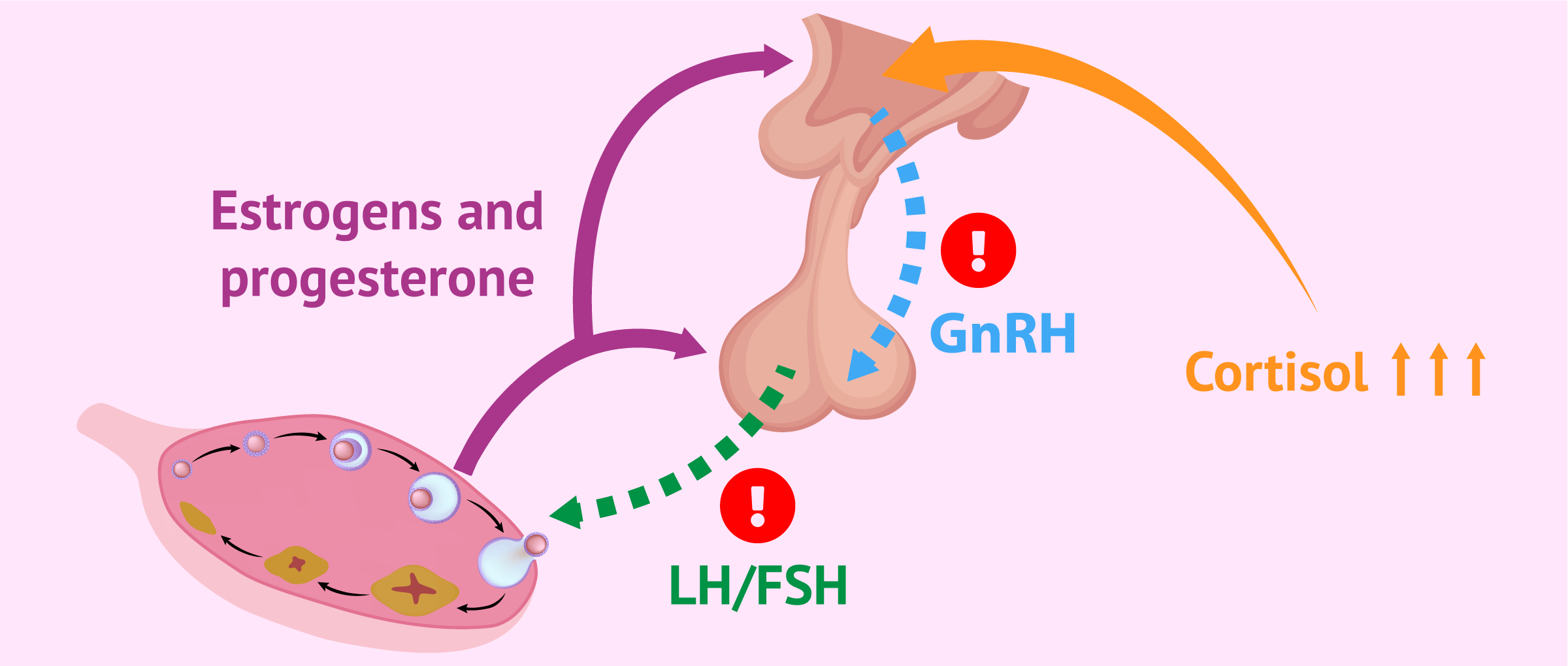
– Ovulation is regulated by hormones including gonadotropin-releasing hormone, follicle-stimulating hormone, and luteinizing hormone.
– After ovulation, the egg travels through the fallopian tube to reach the uterus.
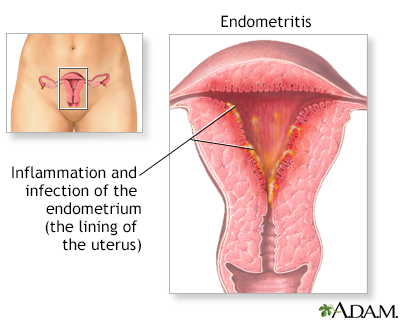
– Progesterone is produced to prepare the uterine lining for pregnancy.
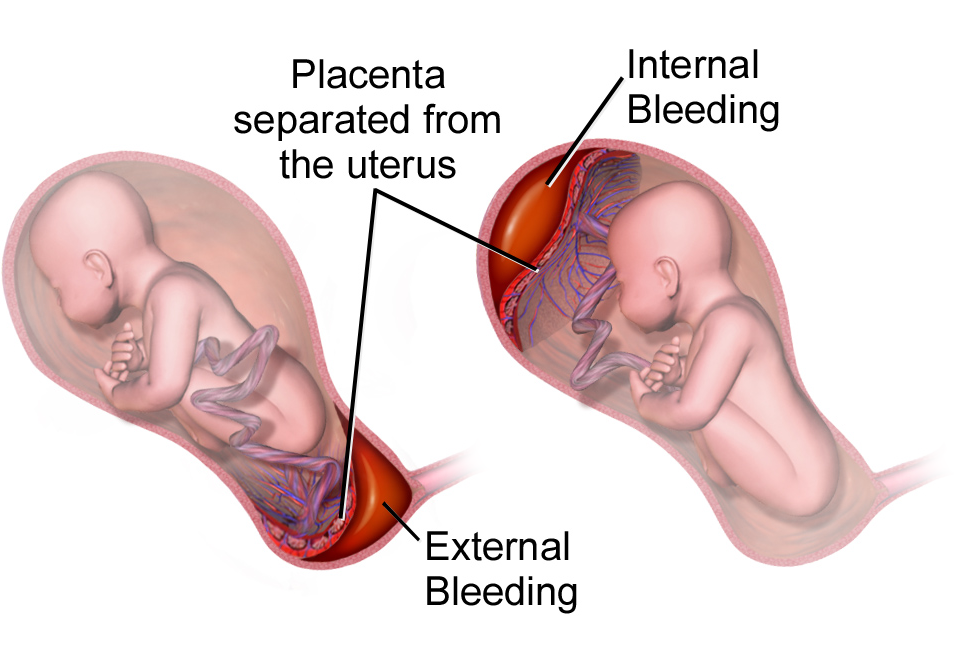
– Low progesterone levels during anovulatory cycles can cause significant bleeding.
– Symptoms of anovulation include missing periods, irregular periods, lack of cervical mucus, abnormal periods (heavy or light), and irregular basal body temperature.
– Girls who have just started their periods and women approaching menopause are at higher risk of anovulatory cycles.
– Other factors increasing the risk for anovulation include excessive exercise patterns.
– Anovulation is caused by an imbalance of hormones involved in ovulation.
– Hormonal disorders and circumstances such as hyperandrogenism, hypogonadotropic hypogonadism, hypothyroidism, hyperprolactinemia, low levels of gonadotropin-releasing hormone, and certain medications can cause anovulation.
– Irregular periods are a common sign, and diagnosis can be done through blood tests and pelvic organ examination.
– Treatment involves lifestyle changes, adjusting current medications, and potentially using a human chorionic gonadotropin injection.
– Treatment options for anovulation include hormonal medications such as clomiphene citrate, follicle-stimulating hormone injections, and gonadotropin-releasing hormone agonists and antagonists injections.
– If these treatments are unsuccessful, options such as intrauterine insemination or in vitro fertilization are available for those trying to conceive.
– Anovulatory bleeding can cause irregular, prolonged, and heavy bleeding.
– The return to ovulation after an anovulatory cycle can vary from person to person.
– Women with an anovulatory cycle typically do not experience ovulation but may experience bleeding due to hormonal changes.
– Lifestyle modifications can help naturally treat an anovulatory cycle, such as improving sleep quality, balancing hormones naturally, and adjusting dietary habits.
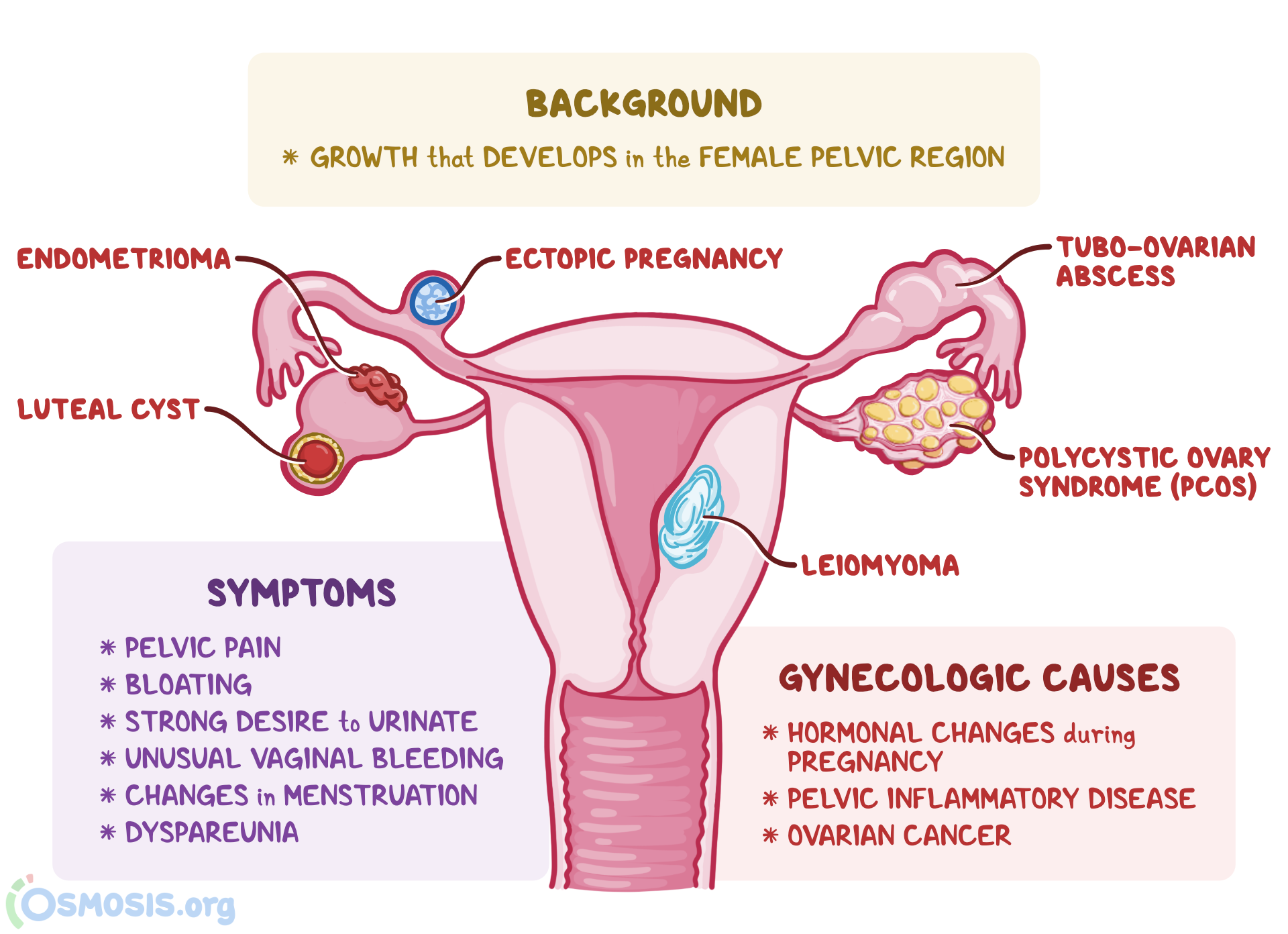
– Ovaries play a role in menstruation and conception by producing eggs and hormones.
– Around 1000 immature eggs are lost every month during menstruation.
– There are four phases of ovulation: menstrual phase, follicular phase, ovulatory phase, and luteal phase.
– Ovulation can be induced using medication like Clomiphene citrate.
– The egg can live for 12 to 24 hours after ovulation, and the fertile window for pregnancy is five days before until one day after ovulation.
– Ovulation can cause abdominal pain and light bleeding. The pain depends on which ovary is releasing the egg.
– Anovulation is when the ovaries don’t release an egg, causing irregular or absent periods.
– It is common for young girls, women approaching menopause, and women with regular cycles to experience anovulation.
– Anovulation occurs when hormonal levels are out of balance.
– Potential causes of anovulation include PCOS, weight issues, over-exercising, thyroid and pituitary disorders, and certain medications.
– Symptoms of anovulation may include heavy periods, irregular bleeding, or no bleeding at all.
– To diagnose anovulation, it is recommended to track your menstrual cycle and discuss any concerns with a doctor. They may also recommend blood tests to measure hormone levels.
– The treatment for anovulation varies depending on the underlying cause. Weight loss or weight gain, depending on whether the person is overweight or underweight, can help regulate periods.
– Fertility drugs may be prescribed if lifestyle changes do not work, and the person is otherwise healthy to conceive.
– Getting pregnant with anovulation can be challenging, but treating underlying conditions such as polycystic ovary syndrome (PCOS) and hypothyroidism can increase the chances of pregnancy.
– In some cases, the assistance of a fertility specialist may be necessary.