Perimenopausal Syndrome: Understanding Symptoms, Treatments, and SelfCare Strategies
– Menopause typically occurs between the ages of 40 and 58, with an average age of 51.
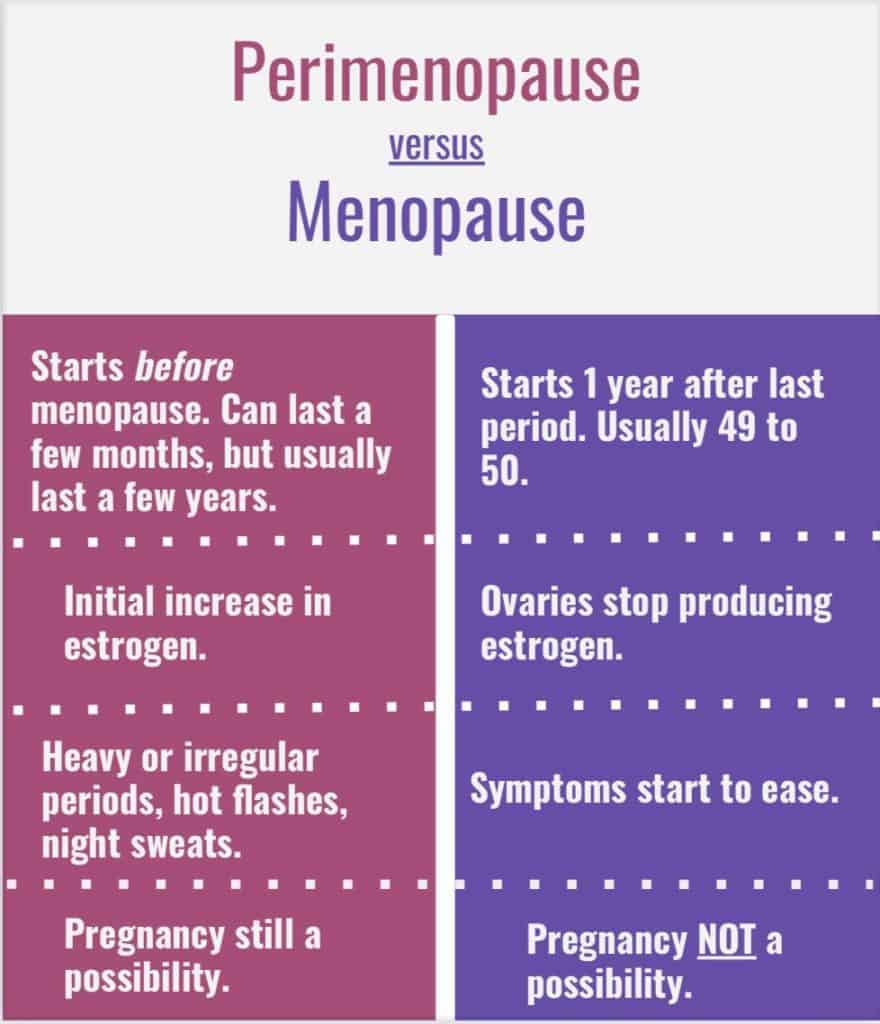
– Perimenopause is the transitional phase before menopause and can last for 4 to 8 years.
– Smoking and genetics can influence the timing of natural menopause.
– Hot flashes are the most common symptom of menopause, lasting 1 to 5 minutes and often accompanied by a cold chill.
– Night sweats, hot flashes at night, can disrupt sleep.
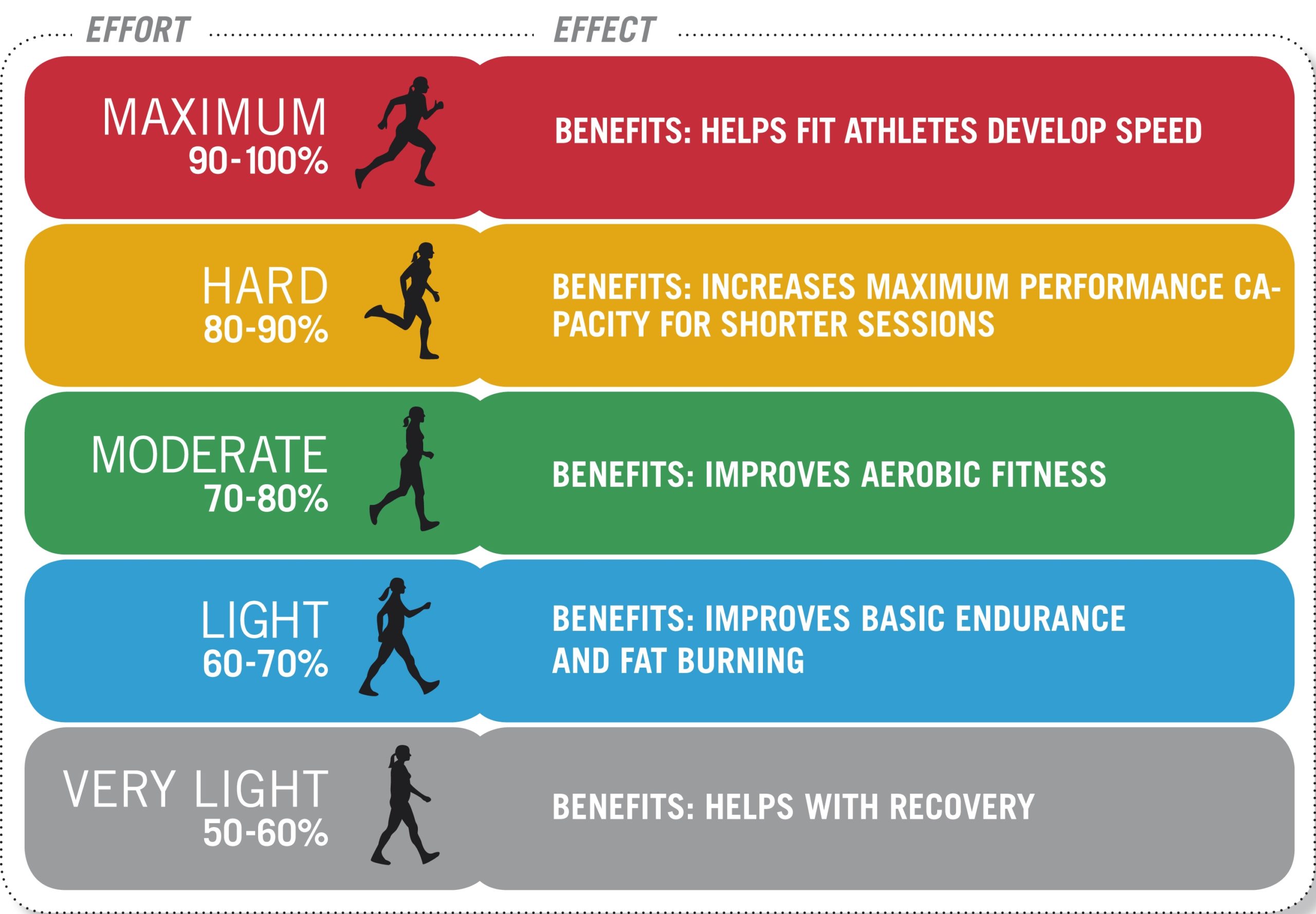
– Treatments for hot flashes and night sweats include lifestyle changes, nonprescription remedies, hormone therapy, and nonhormonal prescription drugs.
– Estrogen decline during menopause can lead to vaginal atrophy, resulting in dryness and thinning of vaginal tissues.
– Over-the-counter lubricants and moisturizers can alleviate pain during intercourse.
– For severe symptoms, low-dose vaginal estrogen products may be necessary.
– Perimenopausal syndrome occurs when a woman has missed her period for 12 consecutive months with no other causes.
– Each woman’s experience of menopause is unique, with some experiencing no physical changes during perimenopause and others having symptoms such as hot flashes, night sweats, and vaginal changes.
– Severity of body changes during perimenopause varies, but they are generally considered natural and normal.
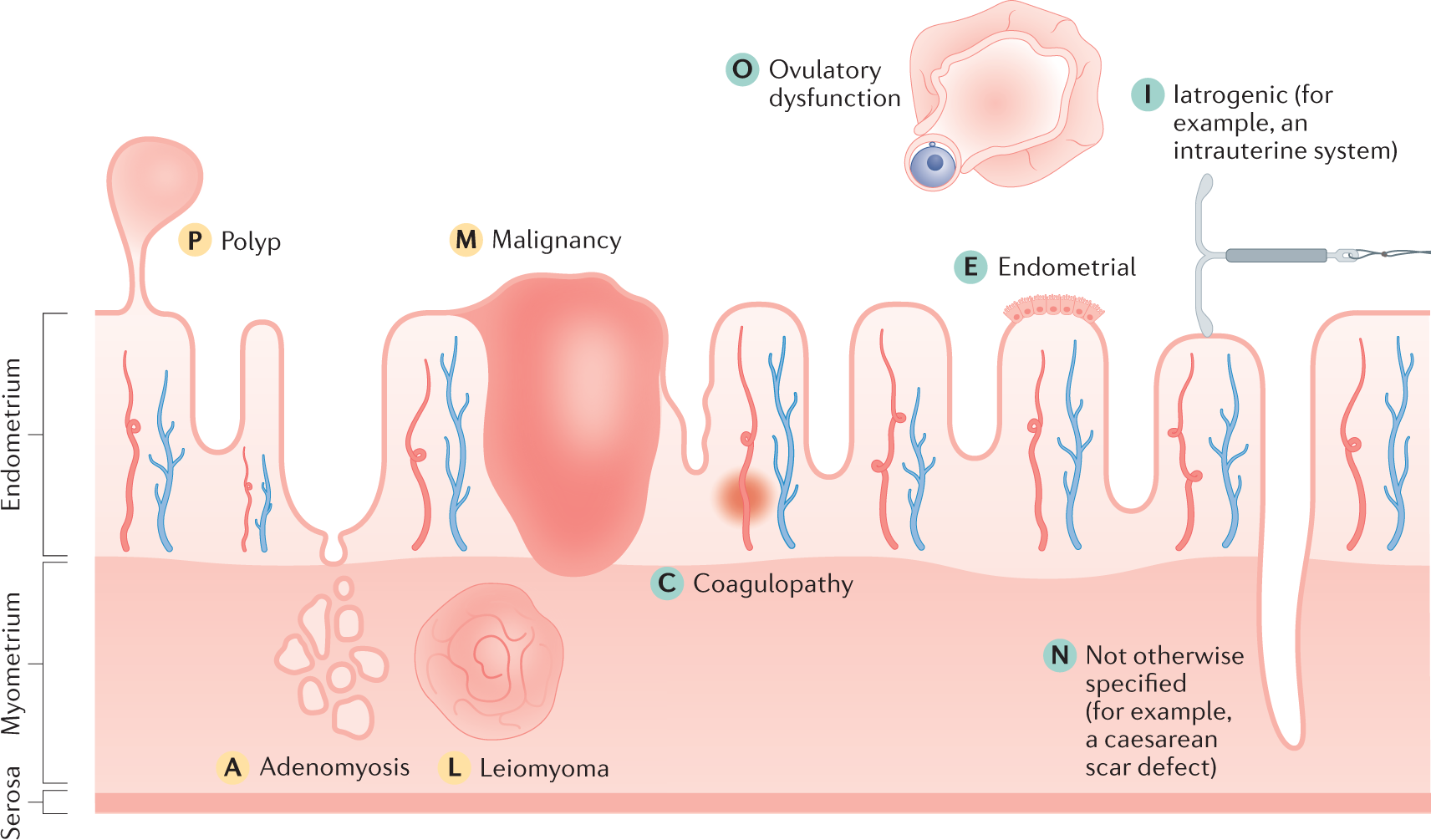
– Perimenopause begins in a woman’s 40s or even earlier and involves fluctuating estrogen levels, leading to irregular menstrual cycles, hot flashes, sleep problems, vaginal dryness, mood changes, and bladder problems.
– Treatments are available to alleviate these symptoms.
– Once a woman has gone through 12 consecutive months without a menstrual period, she has officially reached menopause.
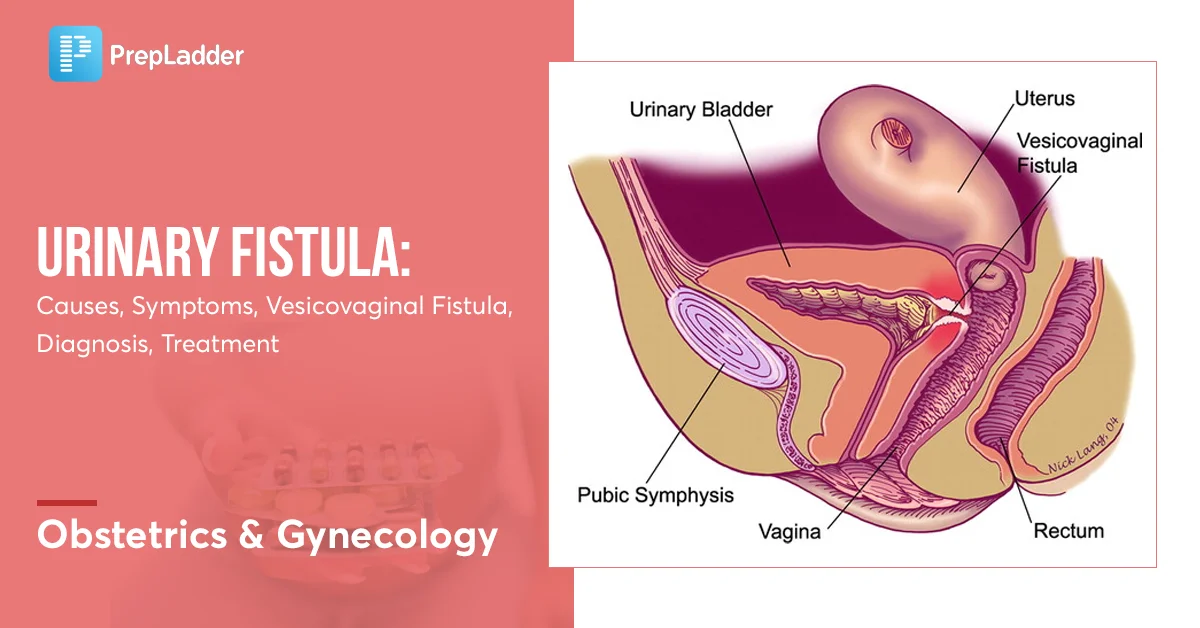
– Decreased estrogen levels during perimenopause can lead to loss of tissue tone, making women more vulnerable to urinary or vaginal infections and contributing to urinary incontinence.
– Low estrogen levels can cause painful intercourse due to vaginal tissues losing lubrication and elasticity.
– Fertility decreases during perimenopause, but pregnancy is still possible until no periods occur for 12 months.
– Sexual arousal and desire may change during perimenopause, but previous satisfactory sexual intimacy is likely to continue.
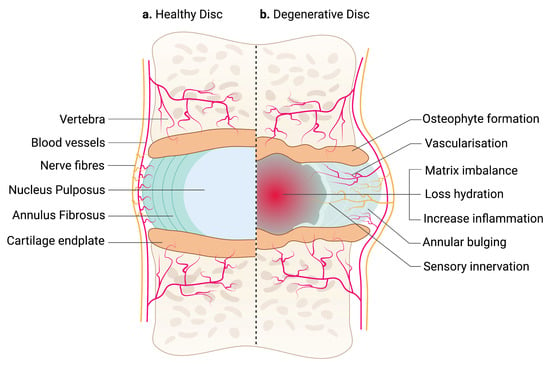
– Declining estrogen levels increase the risk of osteoporosis as bone loss outpaces replacement.
– Cholesterol levels change during perimenopause, with an increase in “bad” cholesterol (LDL) and a decrease in “good” cholesterol (HDL), increasing the risk of heart disease.
– Women experiencing disruptive symptoms during perimenopause should seek evaluation and management from a doctor.