– Preeclampsia is a complication of pregnancy.
– Symptoms include high blood pressure, proteinuria, and organ damage.
– It usually occurs after 20 weeks of pregnancy in women with previously normal blood pressure.
– If left untreated, it can be fatal for both mother and baby.
– Early delivery of the baby is often recommended, based on the severity of the condition and gestational age.
– Treatment includes monitoring and medications to lower blood pressure and manage complications.
– Preeclampsia can also develop after delivery, known as postpartum preeclampsia.
– Preeclampsia is a serious condition that can occur after the 20th week of pregnancy or after giving birth.
– It can cause high blood pressure and affect the functioning of organs such as the kidneys and liver.
– Preeclampsia is responsible for 10 to 15 percent of maternal deaths worldwide.
– In the United States, it affects 5 to 8 percent of pregnancies and often leads to preterm birth.
– Signs and symptoms of preeclampsia include high blood pressure, changes in vision, headaches, nausea, pain in the upper right belly area, sudden weight gain, swelling, and trouble breathing.
– Taking low-dose aspirin may help reduce the risk of preeclampsia and preterm birth for some women.
– Low-dose aspirin, also known as baby aspirin or 81 mg aspirin, can be bought over-the-counter or prescribed by a healthcare provider.
– It is important to follow the recommended dosage and instructions given by the healthcare provider when taking low-dose aspirin for preeclampsia prevention.
– The American College of Obstetricians and Gynecologists (ACOG) states that taking low-dose aspirin during pregnancy has a low risk of serious complications and is considered safe.
– Risk factors for preeclampsia include a history of preeclampsia in a previous pregnancy, pregnancy with multiples (twins, triplets), high blood pressure, diabetes, kidney disease, or autoimmune diseases like lupus. Other risk factors include being a first-time mother, having obesity, a family history of preeclampsia, complications in previous pregnancies, fertility treatment like in vitro fertilization (IVF), and being older than 35.
– Certain groups, such as African-American women and those with lower income, are at higher risk for complications like preeclampsia due to historical health disparities and unequal access to healthcare.
– Without treatment, preeclampsia can have serious health consequences for both the mother and baby, potentially leading to death.
– Preeclampsia is a condition during pregnancy that can lead to serious complications and even death for both the mother and baby.
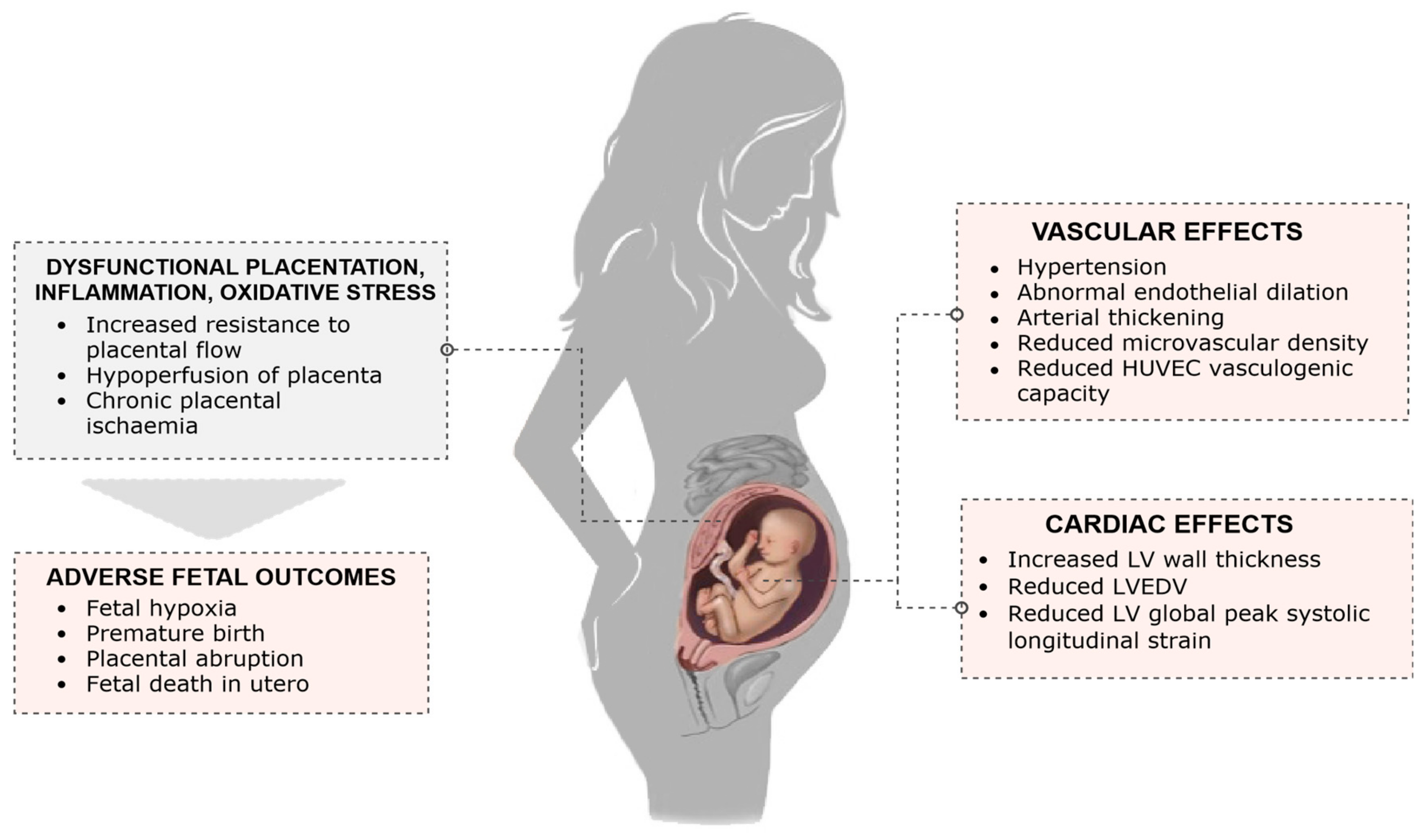
– The condition can cause kidney, liver, and brain damage, as well as problems with blood clotting.
– Eclampsia, characterized by seizures or a coma, is a rare and life-threatening complication that can occur after preeclampsia.
– Stroke can occur if the blood supply to the brain is interrupted or reduced.
– Pregnancy complications from preeclampsia include preterm birth, placental abruption, and intrauterine growth restriction.
– Preeclampsia narrows blood vessels in the uterus and placenta, resulting in poor growth of the baby in the womb.
– Low birth weight and postpartum hemorrhage are potential complications of preeclampsia.
– Preeclampsia increases the risk of heart disease, diabetes, and kidney disease later in life.
– Diagnosis of preeclampsia involves measuring blood pressure and testing urine for protein at every prenatal visit. Additional lab work and ultrasound tests may be done.
– Treatment for preeclampsia depends on its severity and the stage of pregnancy. Mild cases may require regular monitoring and check-ups, potentially including hospitalization.
– Most women with mild preeclampsia are delivered by 37 weeks of pregnancy.
– Severe preeclampsia combined with HELLP syndrome requires early delivery. Blood transfusions may be necessary.
– Vaginal birth may be safer than a C-section, as long as there are no complications with blood clotting.
– Postpartum preeclampsia is a rare condition that can occur within 48 hours to 6 weeks after giving birth. It requires medical attention.
– Possible risk factors for postpartum preeclampsia include previous gestational hypertension or preeclampsia, obesity, and c-section.
– Complications from postpartum preeclampsia include HELLP syndrome, seizures, pulmonary edema, stroke, and thromboembolism.
– Diagnosis is done through blood and urine tests.
– Treatment may include magnesium sulfate to prevent seizures and medication to lower blood pressure.
Continue Reading