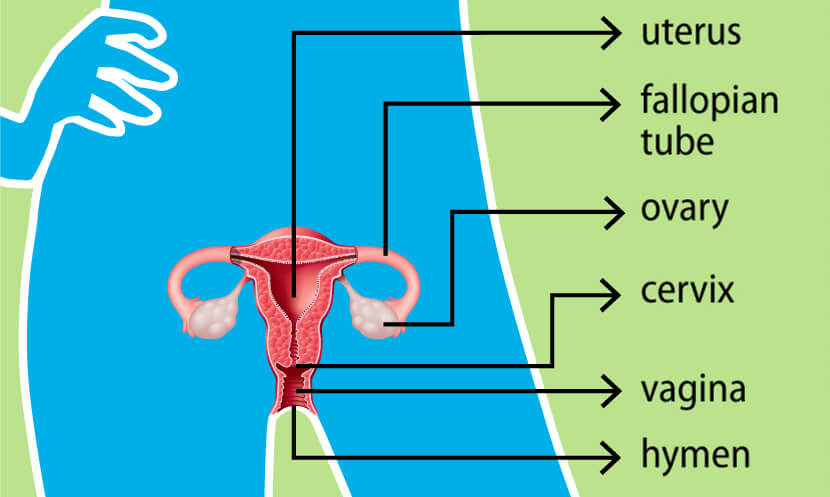
– Placental abruption is when the placenta detaches partially or completely from the wall of the uterus, causing bleeding in the mother.
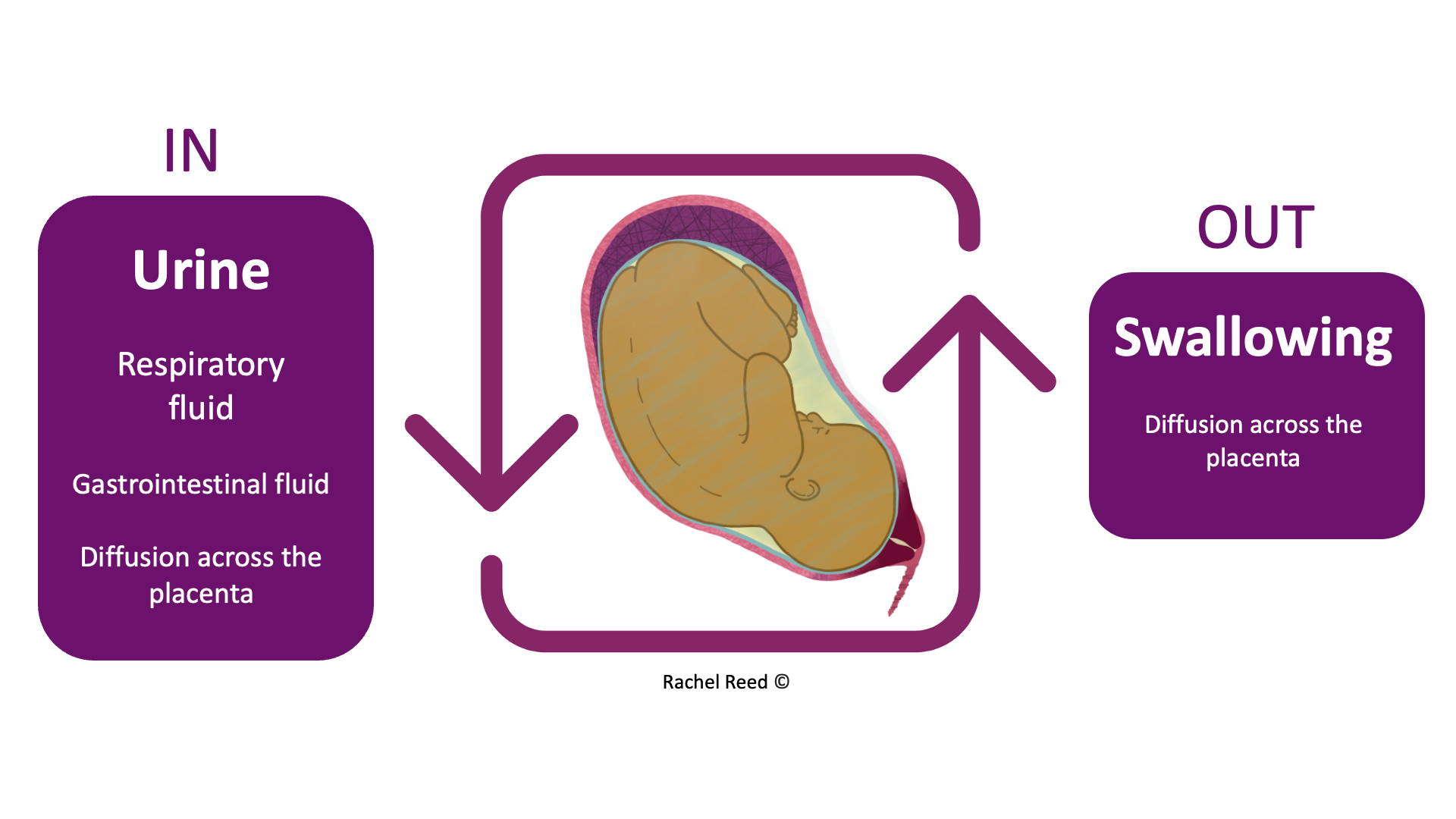
– It can interfere with the baby’s supply of oxygen and nutrients from the mother’s bloodstream through the lining of the uterus.
– Prompt medical treatment is necessary to prevent dire consequences for both the mother and baby, including death.
– Worldwide, placental abruption occurs in about one pregnancy in every 100.
– About 50% of cases are mild and can be managed with ongoing monitoring. 25% are moderate, and 25% threaten the life of both the baby and the mother.
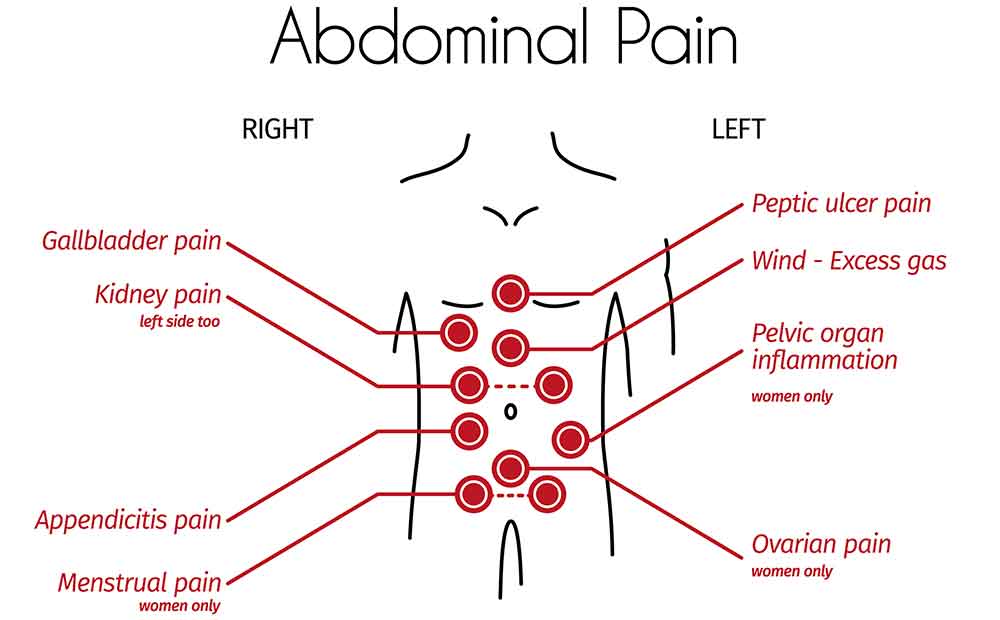
– Symptoms of moderate to severe placental abruption include bleeding, continuous abdominal and lower back pain, tender and hard uterus, very frequent uterine contractions, and fetal distress.
– In some cases, bleeding may be scanty or non-existent due to a retroplacental clot.
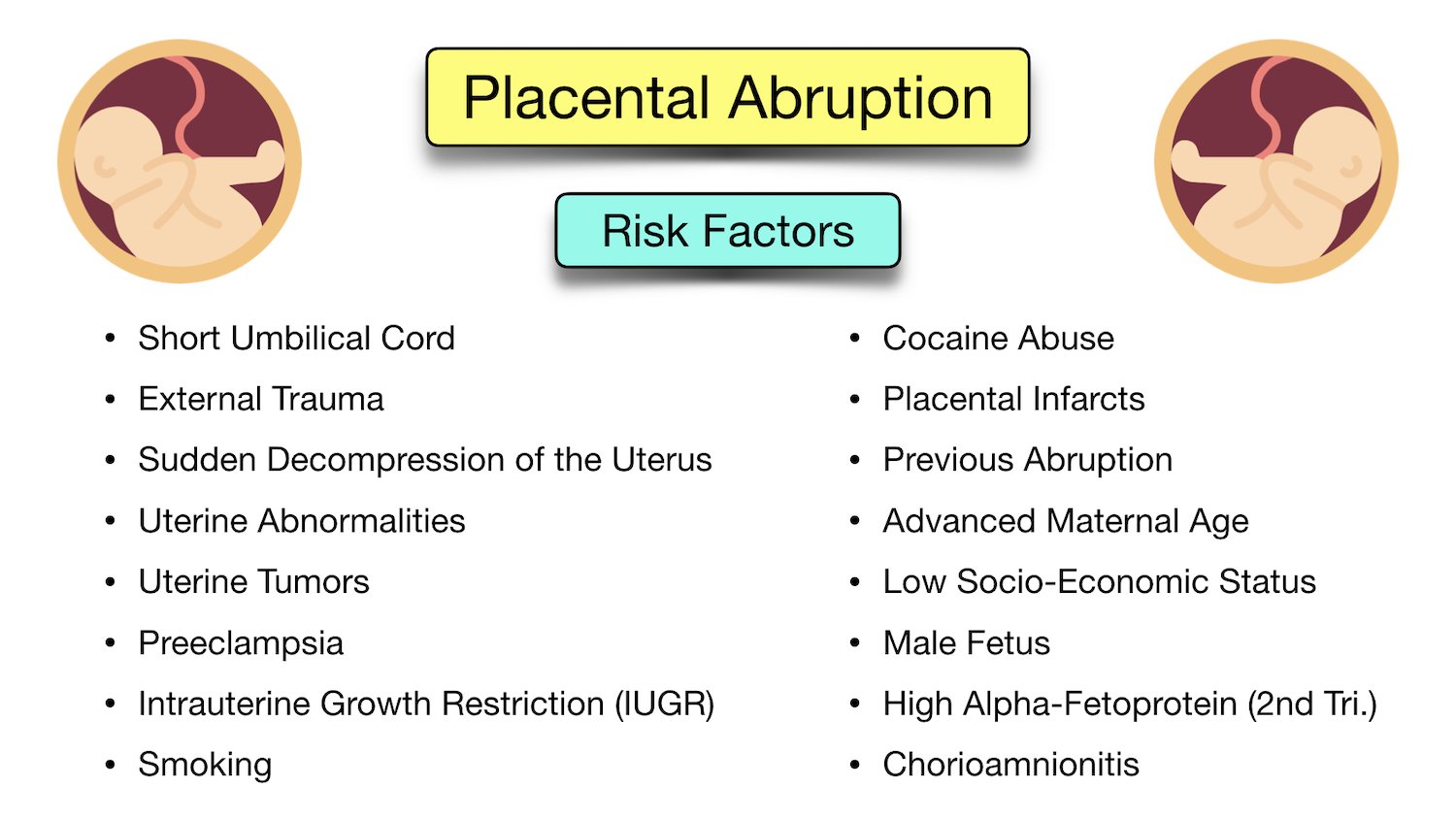
– The exact cause of placental abruption is unknown in most cases, but it is thought that abnormal blood supply in the uterus or placenta may play a role.
– Known causes of placental abruption include abdominal trauma and uterine decompression.
– Certain factors, such as advanced maternal age, prior pregnancies, and carrying multiple fetuses, increase the risk of placental abruption.
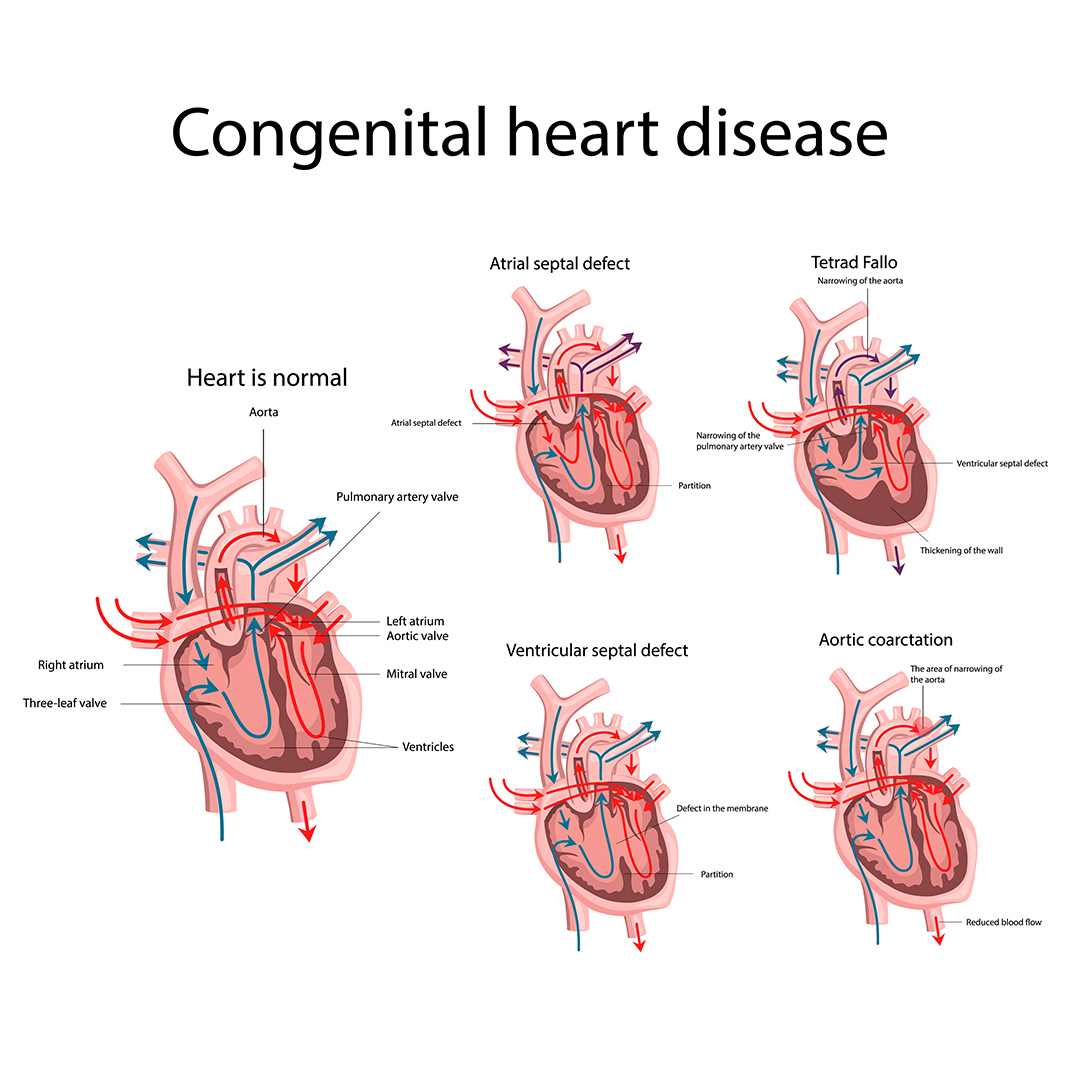
– High blood pressure increases the risk of abnormal bleeding between the placenta and the uterine wall.
– Excessive amniotic fluid increases the risk of bleeding between the placenta and the uterine wall.
– Substance use during pregnancy, such as smoking, alcohol use, and taking drugs like methamphetamine or cocaine, increase the risk of placental abruption.
– Any blood condition that affects the blood’s ability to clot can increase the risk of placental abruption.
– Procedures such as amniocentesis and amnioreduction involve a needle inserted through the mother’s abdomen into the uterus and can rarely cause bleeding.
– External cephalic version, a procedure to turn a breech baby to a head-down position, can occasionally dislodge the placenta.
– Complications in severe cases of placental abruption can include decreased oxygen to the baby, stillbirth, and maternal blood loss.
– Diagnosis of placental abruption can be done through medical history, physical examination, blood tests, ultrasound, and fetal heartbeat monitoring.
– Treatment depends on the severity of the condition and may include rest, induction of labor, vaginal birth or caesarean section, and immediate delivery.
– Severe cases may require supportive care, blood transfusion, or emergency hysterectomy.
– It is impossible to prevent placental abruption, but the risk can be reduced by avoiding substances such as cigarettes, alcohol, and street drugs, and controlling high blood pressure.
Continue Reading