List pertinent to the keyword ‘epithelial tumour of ovary’:
1. Epithelial ovarian tumors are classified as benign, borderline, or malignant.
2. Benign tumors are non-cancerous.
3. Borderline tumors may become harmful if allowed to grow.
4. Malignant tumors, called carcinomas, are invasive cancers that can spread to other areas of the body.
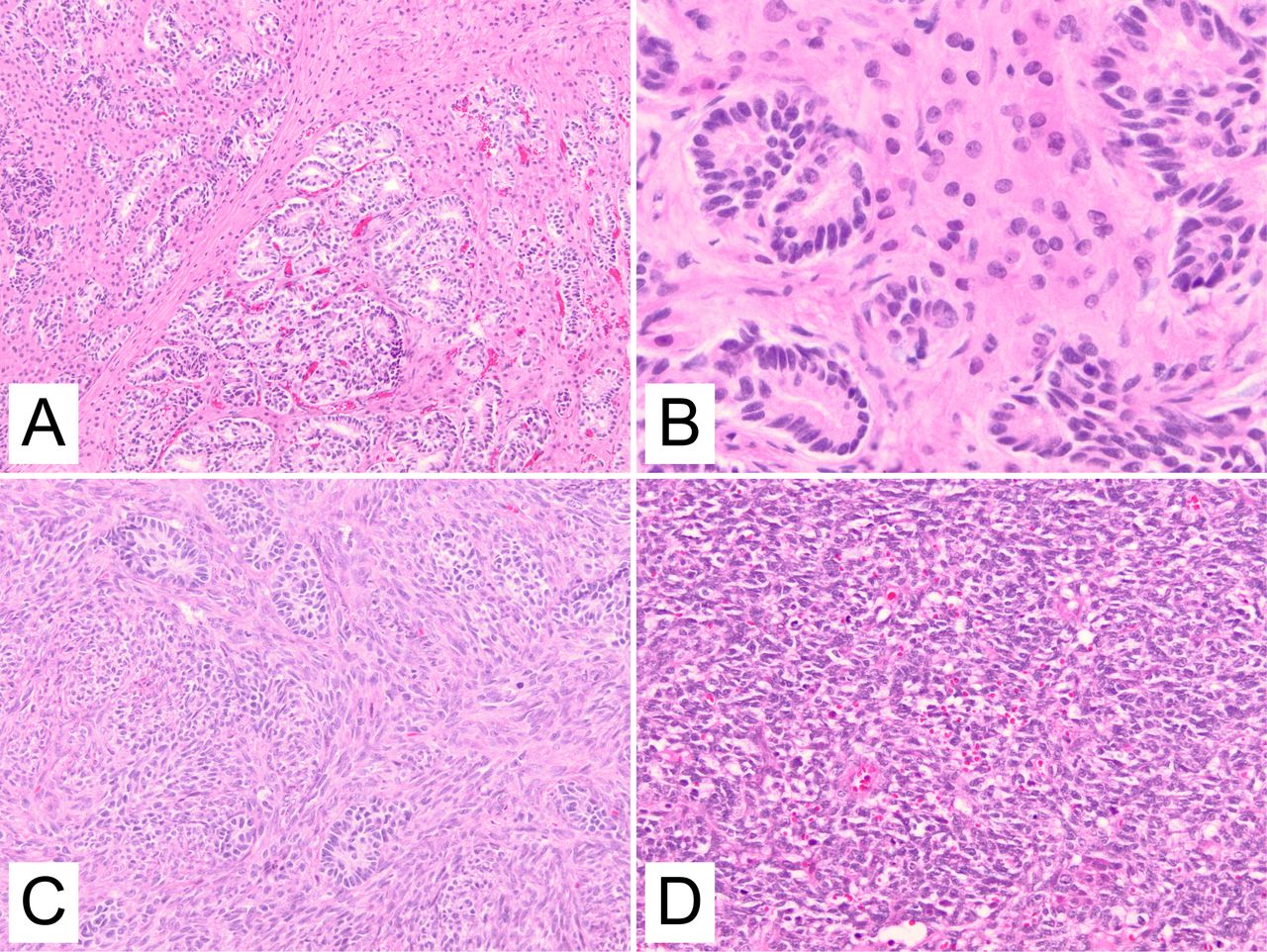
5. The four main types of epithelial ovarian cancer are serous carcinoma, mucinous carcinoma, endometrioid carcinoma, and clear cell carcinoma.
6. Serous carcinomas are the most common, accounting for 52% of cases.
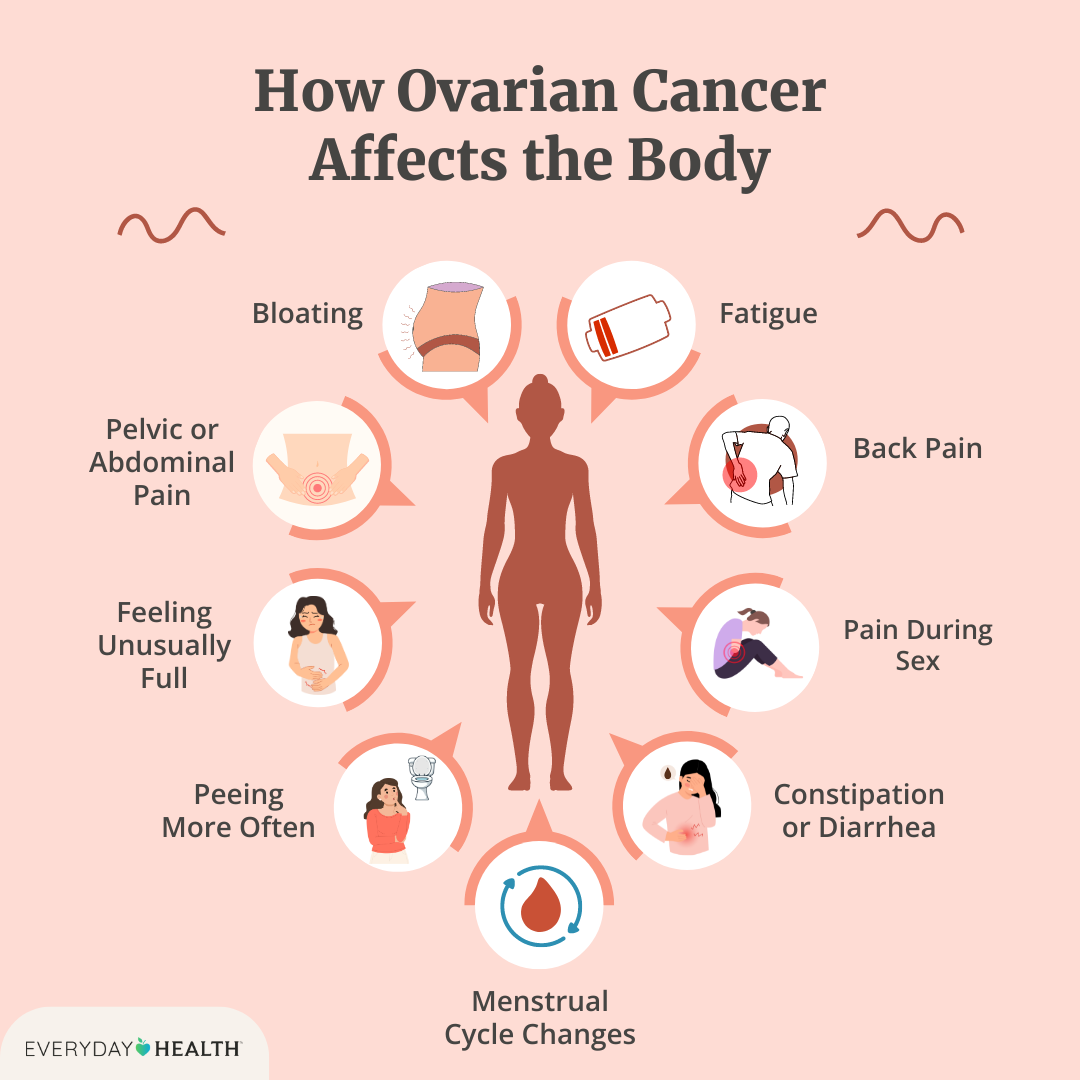
7. Symptoms of epithelial ovarian cancer include feeling full quickly after eating, loss of appetite, bloating, abdominal and pelvic pain, ascites, urinary symptoms, vaginal bleeding, and digestive issues.
8. Gene mutations, such as BRCA1 and BRCA2, can increase the risk of ovarian cancer.
9. Around 20-25% of ovarian cancers are inherited.
10. People with a personal or family history of breast cancer have an increased risk of ovarian cancer.
11. Common risk factors for ovarian cancer include age, family history of ovarian cancer, breast cancer, or colorectal cancer.
12. Epithelial ovarian cancer cannot be detected by one specific test.
13. CA-125 blood test may be used to detect signs of ovarian cancer.
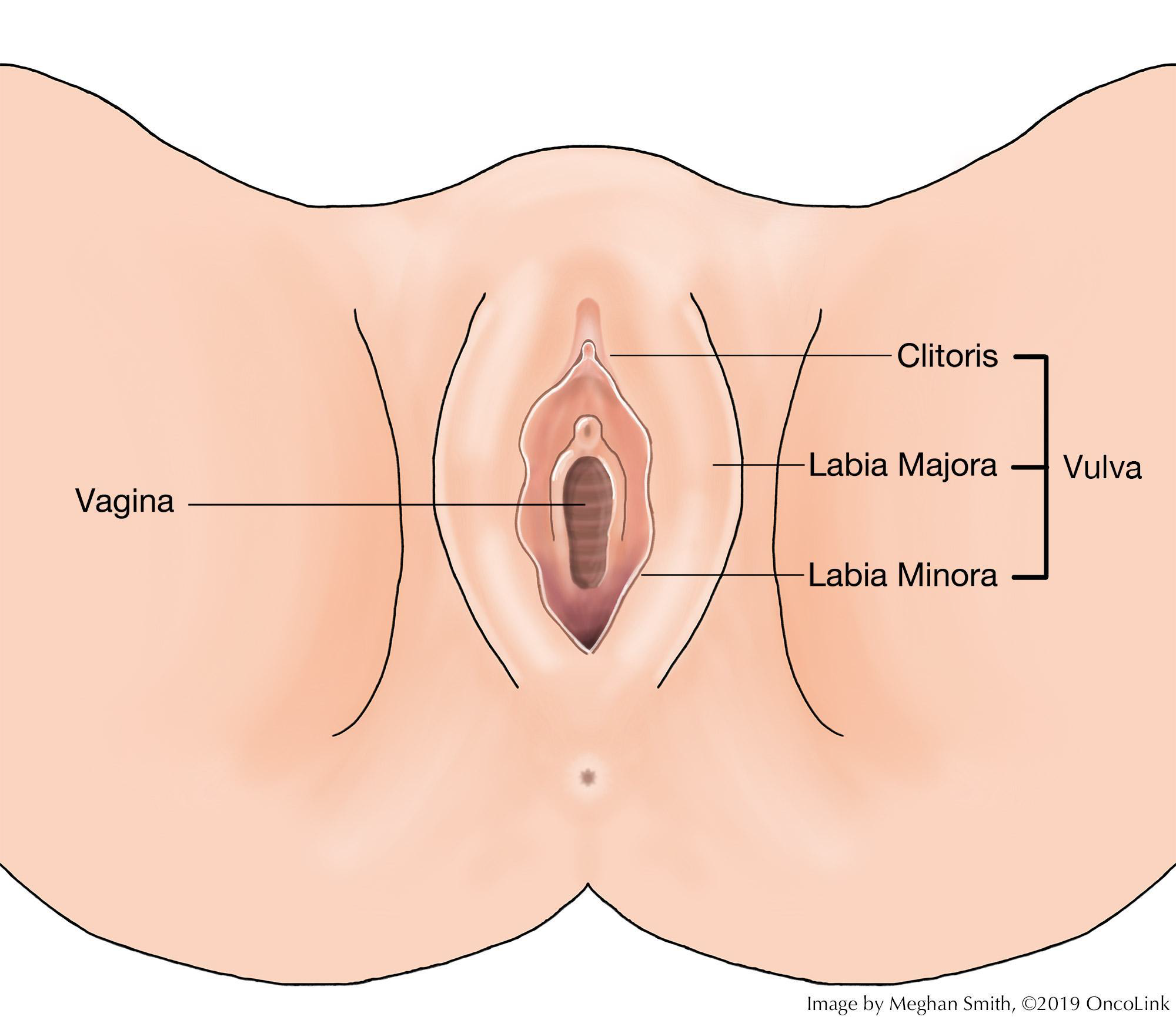
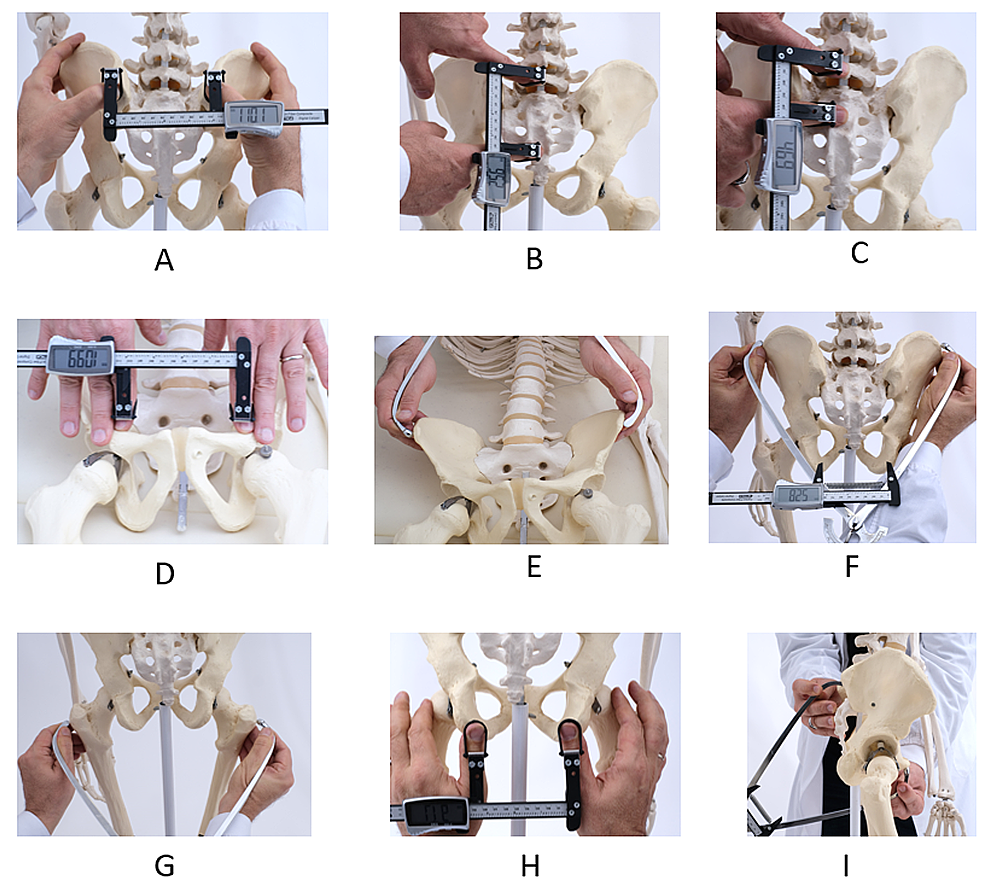
14. Imaging tests such as transvaginal ultrasound, computed tomography, or magnetic resonance imaging may be requested to examine reproductive organs.
15. Laparoscopy may be used as a surgical diagnostic test to examine reproductive organs and take tissue samples for biopsy.
16. A biopsy is the only way to determine if a mass is cancerous or benign.
17. Ascites formation in the abdomen may help in diagnosing ovarian cancer through a procedure called paracentesis.
18. Treatment for ovarian cancer is personalized based on individual needs and goals.
19. There are four stages of ovarian cancer.
20. Surgery is performed to remove as much of the cancer as possible.
21. Chemotherapy is commonly used in the treatment of epithelial ovarian cancer.
22. Targeted therapy, which attacks proteins in cells, is sometimes used in combination with surgery and chemotherapy.
23. Hormone therapy is rarely used for epithelial ovarian cancer.
24. Palliative care aims to help manage emotional stress, medication side effects, pain, and symptoms that affect the patient’s quality of life.
Continue Reading