– An intrauterine device (IUD) is a popular form of reversible birth control that is more than 99% effective at preventing pregnancy with typical use.
– It is possible to become pregnant with an IUD inserted, although it is rare. The failure rate of IUDs is as low as 0.02%, meaning pregnancy could happen in about 1 out of every 5,000 people with an IUD.
– Pregnancy with an IUD can occur if the IUD is not effective immediately or if it shifts its position.
– Copper IUDs, like Paragard, protect against pregnancy immediately due to the copper changing the uterine environment. Hormonal IUDs, like Mirena or Kyleena, take about seven days to start working, but are effective immediately if inserted during your period.
– If an IUD shifts position or remains in the body longer than recommended, it may no longer be fully effective at preventing pregnancy.
– It is important to contact healthcare providers if pregnancy is suspected while an IUD is in place, as it can be dangerous.
– Healthcare providers can discuss options for terminating the pregnancy or continuing with the pregnancy in these cases.
– IUDs have varying recommended durations of use: Skyla (3 years), Kyleena (5 years), Mirena (8 years), Paragard (10 years), Liletta (8 years).
– Signs that the IUD may be out of place and the person may be at risk of pregnancy include: inability to feel the strings, shorter or longer strings than usual, ability to feel the IUD itself, pelvic pain, abnormal vaginal bleeding, severe cramping, and changes in discharge.
– Symptoms of pregnancy with an IUD are similar to typical early pregnancy symptoms: missed periods, nausea and vomiting, headaches, sore and enlarged breasts, tiredness or fatigue, mild cramping, and light spotting.
– It is recommended to take an at-home pregnancy test if pregnancy is suspected, but accuracy depends on following instructions and not testing too early after conception. It is also advised to consult a healthcare provider and consider a pregnancy test in the office.
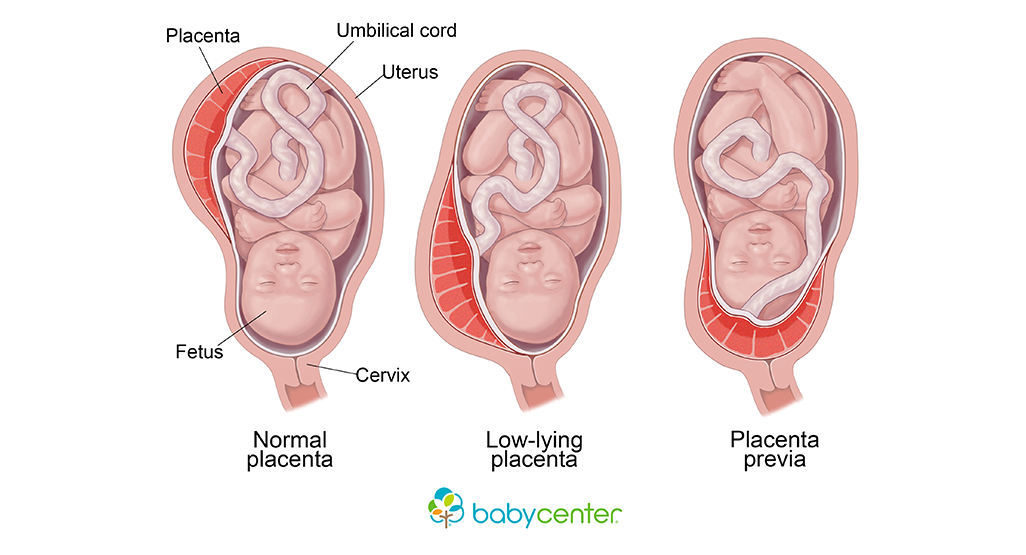
– Risks of pregnancy with an IUD include ectopic pregnancy, miscarriage, preterm delivery, uterine and fetal infections, slow fetal growth, early membrane rupture, and low birth weight.
– It is important to see a healthcare provider immediately if any problems with the IUD or suspicion of pregnancy arise.
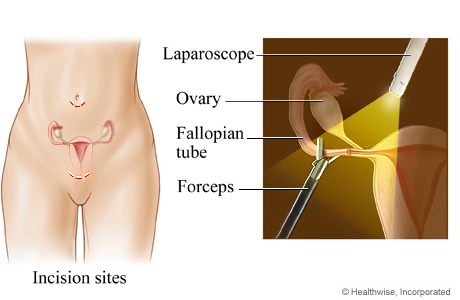
– Terminating the pregnancy should be discussed with a healthcare professional, especially in cases of ectopic pregnancy where it is necessary due to health risks.
– Pregnancies can be terminated with medication or surgery, depending on the stage of pregnancy.
– Removing the IUD can reduce complications, but the pregnancy is still considered high risk.
– IUDs have a lower risk of pregnancy, including ectopic pregnancy, compared to other forms of contraception.
– It is possible to deliver a healthy baby if the embryo is viable.
– Contact a healthcare professional if you suspect your IUD is not effective.
– If you choose to continue the pregnancy, the IUD will likely need to be removed and complications will be monitored throughout the pregnancy.
– Seeking care from an Obstetrician/Gynecologist (Ob/Gyn) is important to reduce the risk of serious complications.
Continue Reading