– Stress incontinence is the unintentional loss of urine.
– It occurs when physical movement or activity puts pressure on the bladder, causing urine leakage.
– It is more common in women than men.
– Symptoms include leaking urine when coughing, sneezing, laughing, bending over, lifting something heavy, or during exercise or sex.
– Stress incontinence can be managed with treatment.
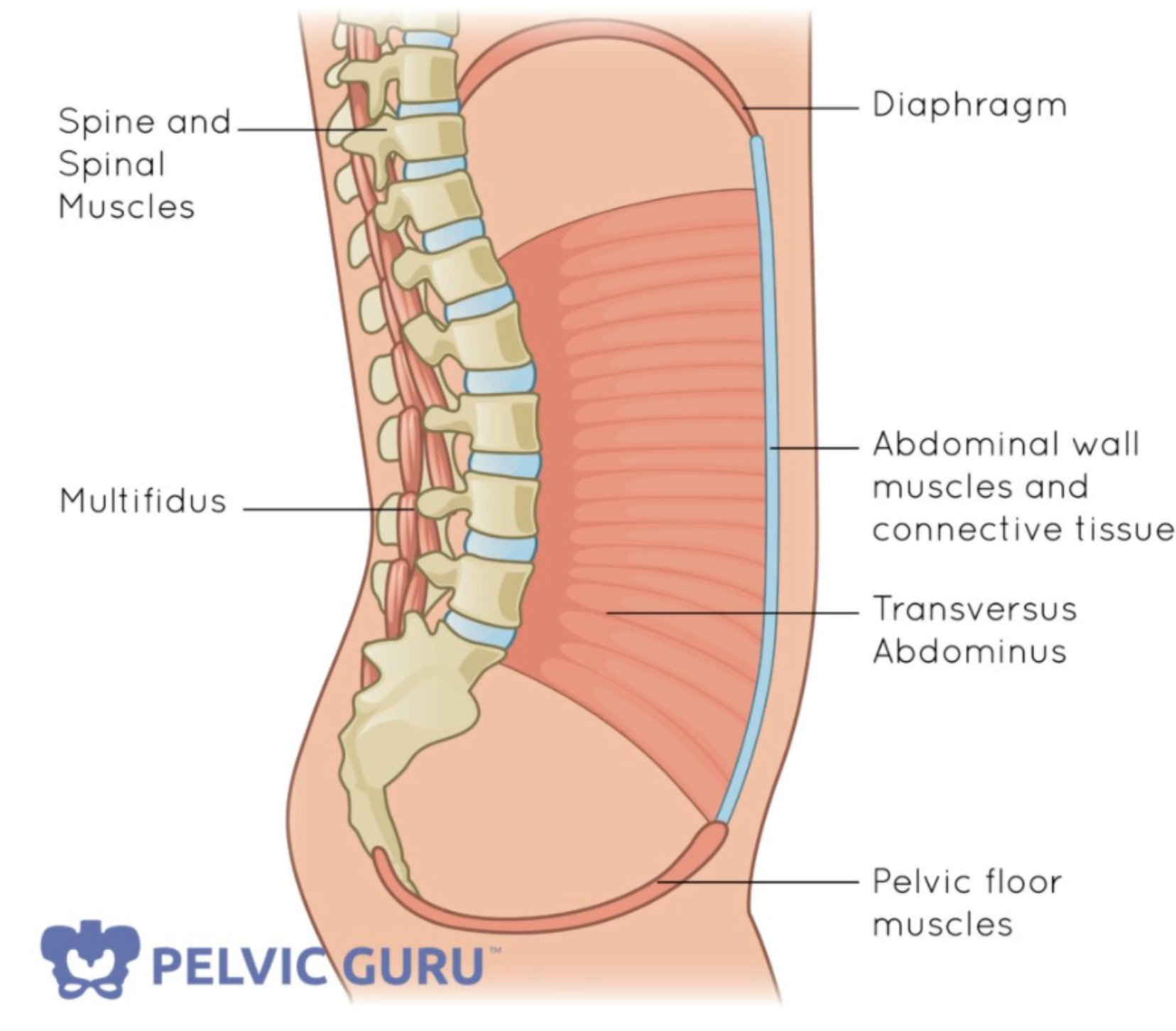
– Stress incontinence is characterized by the weakening of the muscles that control the release of urine in the urinary sphincter.
– This can result in urine leakage when abdominal and pelvic muscles are exerted by actions such as sneezing, bending over, lifting, or laughing hard.
– Common causes of weakened pelvic floor muscles and urinary sphincter include childbirth and prostate surgery.
– Other factors that may worsen stress incontinence include chronic coughing, obesity, smoking, and high-impact activities.
– Risk factors for developing stress incontinence include age, type of childbirth delivery (vaginal delivery increases the risk), body weight (overweight or obese individuals have a higher risk), and previous pelvic surgery (hysterectomy in women and surgery for prostate cancer in men).
– Diagnosis of urinary stress incontinence may include a medical history, physical exam, urine sample, and neurological exam.
– Bladder function tests such as measurements of post-void residual urine, measuring bladder pressures through cystometry, and creating images of the bladder through video urodynamics may be ordered.
– Cystoscopy, a procedure to look for blockages or abnormalities in the bladder and urethra, may also be conducted.
– Results of tests should be discussed with a healthcare provider to determine treatment strategy.
– Mayo Clinic offers expertise in treating urinary stress incontinence.
– Strategies for treating stress incontinence may include pelvic floor muscle exercises, fluid consumption management, healthy lifestyle changes (quitting smoking, losing weight, treating chronic cough), and bladder training.
– There are no approved medications in the US specifically for treating stress incontinence, but the antidepressant duloxetine is used in Europe.
– Devices that can help control stress incontinence in women include vaginal pessaries and urethral inserts.
– Inserts are generally used for heavy activity, such as lifting, running, or playing tennis.
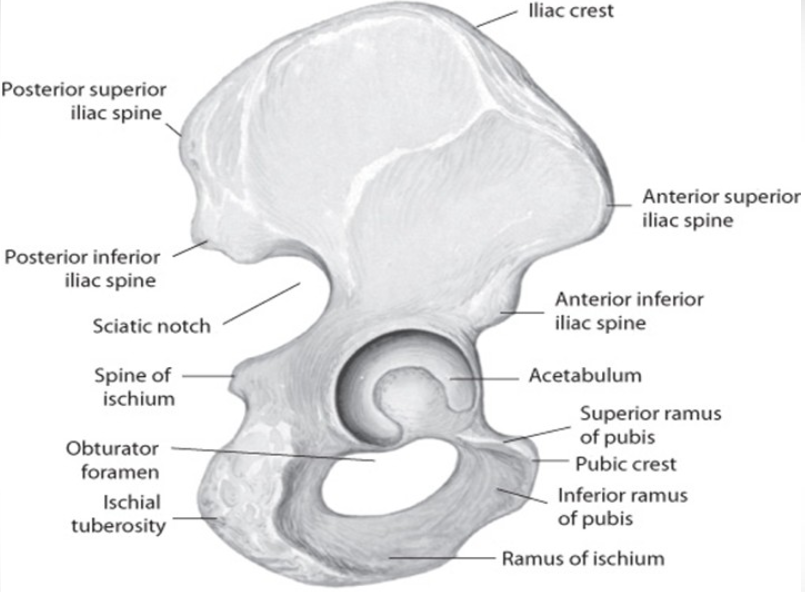
– Surgery options for stress incontinence include the Burch procedure, sling procedure, injectable bulking agents, retropubic colposuspension, and inflatable artificial sphincter.
– The sling procedure is the most common procedure for women with stress urinary incontinence and can also be used for men.
– Injectable bulking agents are synthetic materials that can be injected to bulk up the area around the urethra and improve the closing ability of the sphincter.
– Retropubic colposuspension involves sutures attached to ligaments along the pubic bone to lift and support tissues near the bladder neck and urethra.
– Inflatable artificial sphincter is a surgically implanted device for men that replaces the function of the sphincter.
– Healthy lifestyle practices, such as shedding extra weight, can help ease symptoms of stress incontinence.
– Eating high-fiber foods like whole grains, legumes, fruits, and vegetables can relieve and prevent constipation, which can contribute to urinary incontinence.
– Avoiding foods and beverages like chocolate, coffee, tea, and carbonated beverages that can irritate the bladder may help reduce urinary leakage.
– Smoking can worsen the symptoms of stress incontinence and is a factor in many cases of bladder cancer.
– Treatments for stress incontinence can significantly reduce or eliminate urine leakage.
– Being prepared with sufficient incontinence pads or protective undergarments, a change of clothes, and familiarizing yourself with restroom locations can help when going out.
– Prolonged contact with wet clothing can cause skin irritation, so it is important to keep the skin dry.
– Leaking urine during sexual intercourse can be managed through open communication with your partner.
– Incontinence is not a normal part of aging.
– Treatments are available to cure or significantly reduce the effects of stress incontinence.
– The article suggests being upfront with your partner about your symptoms to make them easier to handle.
– Emptying the bladder before intimacy and avoiding drinking fluids beforehand can reduce the chances of leakage.
– Altering positions during sex may make leakage less likely, with being on top giving better control of pelvic muscles for women.
– Kegel exercises can strengthen pelvic floor muscles and reduce urine leakage.
– Having towels or using disposable pads on the bed can ease worry and contain leakage.
– It is recommended to find a healthcare provider who can work with you to determine the best treatment options for your incontinence.
– Support groups can provide opportunities to voice concerns and offer motivation for self-care strategies.
– Preparing for your healthcare appointment may include filling out a questionnaire and keeping a bladder diary.
– Specialized testing may require referral to a urologist or urogynecologist.
– It is important to provide your healthcare provider with a list of symptoms and any medications, herbs, or vitamin supplements you are taking.
Continue Reading