Imagine a hidden predator silently infiltrating your body, wreaking havoc on your most intimate of organs.
Pelvic Inflammatory Disease (PID), a stealthy infection born from the shadows of sexually transmitted diseases, descends upon its unsuspecting victims.
Its tentacles of pain, fever, and abnormal discharge spread like wildfire.
But fear not, for knowledge is power, and this vicious intruder can be stopped in its tracks with swift, prompt treatment.
Brace yourself as we delve into the treacherous depths of PID, its causes, symptoms, and the vital importance of timely intervention.
pelvic inflammatory disease
Pelvic inflammatory disease (PID) is an infection of a woman’s reproductive organs.
It is often caused by sexually transmitted diseases (STDs) like chlamydia and gonorrhea, but non-sexually transmitted infections can also lead to PID.
Risk factors for PID include untreated STDs, multiple sex partners, a partner with other sex partners, a history of PID, being sexually active and under 25, douching, and using an intrauterine device for birth control.
To reduce the risk of PID, it is recommended to practice abstinence or have sex in a long-term mutually monogamous relationship and use condoms correctly.
PID can be diagnosed through a medical history, physical examination, and other test results.
Symptoms of PID include lower abdominal pain, fever, unusual discharge with a bad odor, pain or bleeding during sex, burning sensation during urination, and bleeding between periods.
It is important to see a doctor if these symptoms occur, if there is suspicion of an STD, or if there are any genital symptoms.
Early diagnosis and treatment can cure PID, but damage to the reproductive system cannot be reversed.
Completing the full course of antibiotics and informing recent sex partners for testing and treatment is crucial.
If left untreated, PID can lead to complications such as scar tissue formation in the fallopian tubes, ectopic pregnancy, infertility, and long-term pelvic or abdominal pain.
To reduce the risk of PID, one should abstain from vaginal, anal, or oral sex, be in a long-term mutually monogamous relationship with a partner who has tested negative for STDs, and use latex condoms correctly.
It is important to consult a doctor if any PID symptoms occur or if there is suspicion of STD exposure.
Early treatment can prevent complications and partners should also be informed to get tested and treated for STDs.
Having had PID before increases the chances of getting it again.
Early treatment of PID can prevent complications such as tubal blockage caused by scar tissue formation.
Key Points:
- Pelvic inflammatory disease (PID) is an infection of a woman’s reproductive organs, often caused by sexually transmitted diseases (STDs) like chlamydia and gonorrhea.
- Risk factors for PID include untreated STDs, multiple sex partners, a history of PID, and douching.
- To reduce the risk of PID, it is recommended to practice abstinence or have sex in a long-term mutually monogamous relationship and use condoms correctly.
- PID can be diagnosed through a medical history, physical examination, and other test results. Symptoms include lower abdominal pain, fever, unusual discharge, and pain or bleeding during sex.
- Early diagnosis and treatment can cure PID, but damage to the reproductive system cannot be reversed. Completing the full course of antibiotics and informing recent sex partners for testing and treatment is crucial.
- If left untreated, PID can lead to complications such as scar tissue formation, ectopic pregnancy, infertility, and long-term pelvic or abdominal pain.
pelvic inflammatory disease – Watch Video
💡
Pro Tips:
1. Pelvic inflammatory disease (PID) is primarily caused by sexually transmitted infections (STIs) such as chlamydia and gonorrhea. However, it can also occur as a result of other non-sexually transmitted bacterial infections, such as from appendicitis or a ruptured appendix.
2. PID can sometimes lead to long-term complications like infertility, ectopic pregnancy (pregnancy outside the womb), and chronic pelvic pain. It is important to seek early treatment to minimize the risk of these complications.
3. During the Victorian era, pelvic inflammatory disease was a known but misunderstood condition referred to as “pelvic cellulitis,” and it was commonly attributed to “hysteria” or regarded as a psychosomatic disorder rather than a physical illness.
4. In some cases, pelvic inflammatory disease can present with subtle or nonspecific symptoms, which makes diagnosing it challenging. Symptoms may include lower abdominal pain, abnormal vaginal discharge, painful intercourse, irregular menstrual bleeding, and low-grade fever.
5. Pelvic inflammatory disease can affect women of all ages, but it is most common in sexually active women under the age of 25. It is crucial to practice safe sex and undergo regular STI screenings to reduce the risk of developing PID.
1. Introduction To Pelvic Inflammatory Disease (PID)
Pelvic Inflammatory Disease (PID) is a serious infection that affects a woman’s reproductive organs. It occurs when bacteria, usually from sexually transmitted diseases (STDs) such as chlamydia and gonorrhea, spread from the vagina and cervix into the uterus, fallopian tubes, and ovaries. However, it’s important to note that PID can also be caused by non-sexually transmitted infections.
PID is a common health issue, particularly among sexually active women under the age of 25. It can have severe implications for a woman’s fertility and overall reproductive health. Therefore, understanding the causes, symptoms, and prevention measures of PID is crucial to maintaining reproductive well-being.
- PID is a serious infection affecting the reproductive organs.
- It is often caused by STDs like chlamydia and gonorrhea.
- Non-sexually transmitted infections can also lead to PID.
- Sexually active women under 25 are at higher risk.
- PID can have severe implications for fertility.
- Understanding the causes, symptoms, and prevention is crucial.
“PID is a serious infection that affects a woman’s reproductive organs.”
2. Common Causes Of PID: STDs and Non-Sexually Transmitted Infections
The most common cause of PID is the contraction of STDs, specifically chlamydia and gonorrhea. When left untreated, these infections can travel up through the cervix and into the reproductive organs, resulting in PID. However, it’s important to note that other types of bacteria, such as those causing bacterial vaginosis or pelvic infections after childbirth or abortion, can also lead to PID.
One of the primary concerns with STDs is that they often go undiagnosed and untreated. This lack of treatment allows the infections to progress and cause significant damage to the reproductive organs. Therefore, practicing safe sex and getting regular screenings for STDs is essential in preventing PID.
3. Factors That Increase The Risk Of PID
Several factors can increase a woman’s risk of developing Pelvic Inflammatory Disease (PID). These include:
- Having an untreated sexually transmitted disease (STD)
- Engaging in sexual activities with multiple partners
- Having a partner who engages in sexual activities with other partners
- Having a history of PID
- Being sexually active and under the age of 25
- Douching
- Using an intrauterine device (IUD) for birth control
These risk factors highlight the importance of education and awareness about safe sexual practices. By understanding these potential risks and taking necessary precautions, individuals can minimize their chances of developing PID.
- Bullet points:
- Untreated STD
- Multiple sexual partners
- Partner engaging in sexual activities with others
- Previous history of PID
- Sexually active and under 25
- Douching
- Using IUD for birth control
Blockquote:
“These risk factors emphasize the importance of education and awareness about safe sexual practices. By understanding the potential risks and taking necessary precautions, individuals can minimize their chances of developing PID.”
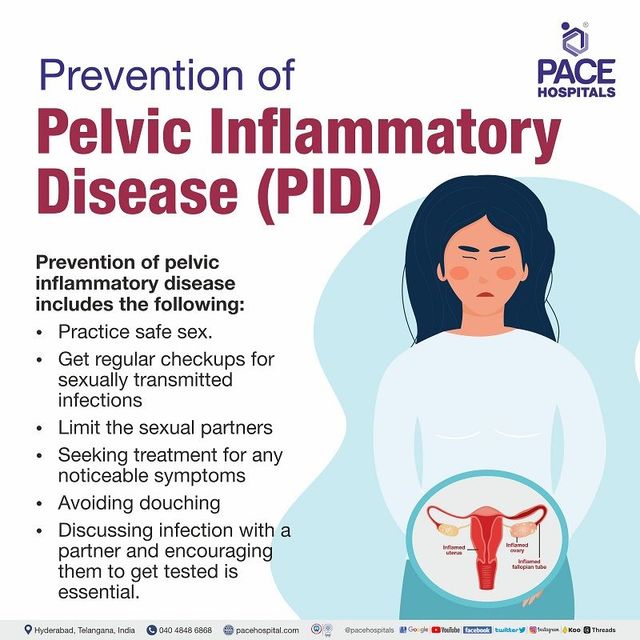
4. Recommendations To Reduce The Risk Of Getting PID
To reduce the risk of contracting PID, it is crucial to practice abstinence from sexual activities or engage in a long-term mutually monogamous relationship where both partners have been tested and are free of STDs. For individuals who are sexually active, using condoms correctly and consistently can provide a significant level of protection against STDs and consequently, PID.
It’s worth noting that douching has been linked to an increased risk of PID. Therefore, it is recommended to avoid this practice as it can disrupt the natural balance of bacteria in the vagina, making it more susceptible to infections.
- Practice abstinence or engage in long-term monogamous relationships with tested partners to reduce risk of PID.
- Use condoms correctly and consistently for protection against STDs and PID.
- Avoid douching as it disrupts the natural balance of bacteria in the vagina and increases the risk of PID.
5. Diagnosis Of PID: Medical History, Physical Examination, and Tests
Diagnosing PID can be challenging as there are no specific tests for the condition. However, healthcare professionals rely on a combination of medical history, physical examination, and laboratory tests to ascertain whether a patient has PID.
During a physical examination, the healthcare provider may look for tenderness in the lower abdomen or back, as well as unusual vaginal discharge. They may also order laboratory tests such as blood tests, urine tests, and cultures to identify any presence of infection or inflammation.
It’s important for individuals experiencing symptoms or suspecting exposure to STDs to seek medical attention promptly. Early diagnosis is crucial in preventing further complications associated with PID.
- Seek medical attention promptly if experiencing symptoms or suspecting exposure to STDs.
- Physical examination may involve checking for tenderness in the lower abdomen or back, as well as unusual vaginal discharge.
- Laboratory tests, such as blood tests, urine tests, and cultures, are commonly used to identify infection or inflammation in PID.
6. Common Symptoms Of PID
PID can cause a range of symptoms that vary in severity. Common signs include:
- Lower abdominal pain
- Fever
- Unusual discharge with a foul odor from the vagina
- Pain or bleeding during sexual intercourse
- A burning sensation during urination
- Bleeding between periods
However, it’s worth noting that not all individuals with PID will experience symptoms.
If any of these symptoms occur, it is crucial to seek medical attention. Prompt diagnosis and treatment can prevent the progression of the infection and reduce the likelihood of long-term complications.
It is important to remember that early detection and treatment are key to managing PID effectively.
- Lower abdominal pain
- Fever
- Unusual discharge with a foul odor from the vagina
- Pain or bleeding during sexual intercourse
- A burning sensation during urination
- Bleeding between periods
7. Importance Of Seeking Medical Attention For PID Symptoms
It cannot be stressed enough how crucial it is to seek medical attention if there is a suspicion of PID or exposure to STDs. PID is a serious condition that requires prompt treatment to prevent further damage to the reproductive system. Delaying medical attention can increase the risk of complications and long-term health consequences.
Additionally, it’s important to communicate openly and honestly with healthcare providers, as this will aid in accurate diagnosis and appropriate treatment.
- Seeking prompt medical attention is crucial if there is a suspicion of PID or exposure to STDs.
- PID is a serious condition that can cause damage to the reproductive system.
- Delaying medical attention can increase the risk of complications and have long-term health consequences.
- Open and honest communication with healthcare providers is essential for accurate diagnosis and treatment.
8. Treatment And Cure Of PID
The treatment of PID involves a course of antibiotics to eliminate the infection. It is important to complete the full course of antibiotics, regardless of symptom improvement. The specific antibiotics prescribed may vary depending on the severity of the infection and individual circumstances.
It is worth noting that PID can be cured with early diagnosis and treatment. However, any damage already done to the reproductive system cannot be reversed. Therefore, seeking medical attention promptly is critical to minimize long-term complications.
9. The Role Of Partners In PID Treatment
Since PID (Pelvic Inflammatory Disease) is often caused by STDs (Sexually Transmitted Diseases), it is crucial for both partners to be involved in the treatment process. Partners should also undergo testing for STDs and, if necessary, receive appropriate treatment.
This collaborative approach is essential in preventing re-infection and promoting overall reproductive health. It allows for the identification and treatment of any underlying infections that may contribute to the development or recurrence of PID.
Open communication between partners is vital to ensure the timely and effective management of PID and reduce the risk of further complications. By discussing symptoms, concerns, and treatment plans, partners can work together to support each other’s health and well-being.
To summarize:
- Both partners should be involved in the treatment process for PID.
- Testing and treatment for STDs are important for both partners.
- Communication between partners is crucial for effective management of PID.
10. Complications Of Untreated PID
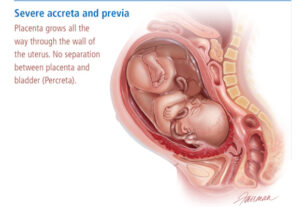
If left untreated, Pelvic Inflammatory Disease (PID) can lead to various complications. One of the most significant complications is the formation of scar tissue in the fallopian tubes, also known as tubal scarring. This scarring can cause blockages, preventing fertilized eggs from reaching the uterus, leading to infertility or an ectopic pregnancy (pregnancy outside the womb).
In addition to fertility issues, untreated PID can result in long-term pelvic or abdominal pain, which can significantly impact a woman’s quality of life. Therefore, it is crucial to seek medical attention at the earliest signs of PID to prevent these potentially severe complications.
“Untreated PID can have serious consequences such as infertility and ectopic pregnancy.”
In conclusion, PID is a serious infection that affects the reproductive organs of women. While STDs are the most common cause of PID, other non-sexually transmitted infections can also lead to this condition. It is important to understand the risk factors, symptoms, and preventive measures associated with PID to ensure optimal reproductive health. Seeking prompt medical attention and involving partners in the treatment process are critical in preventing long-term complications and promoting overall well-being.
- Understand the risk factors, symptoms, and preventive measures associated with PID.
- Seek prompt medical attention at the earliest signs of PID.
- Involve partners in the treatment process.
Keep in mind to prioritize your reproductive health and be attentive to any signs or symptoms of PID.
💡
You may need to know these questions about pelvic inflammatory disease
What are 6 symptoms of PID?
PID, or pelvic inflammatory disease, is a condition that primarily affects the female reproductive system. Common symptoms of PID include pain in the lower abdomen, fever, and vaginal discharge that may have a foul odor. Women with PID may also experience painful sex and urination, as well as irregular menstrual periods. Although rare, some individuals with PID may also experience pain in the upper right abdomen. It is important to be aware of these symptoms and seek medical attention promptly if they occur, as PID can lead to complications if left untreated.
What is the main cause of pelvic inflammatory disease?
The main cause of pelvic inflammatory disease (PID) is the transmission of sexually transmitted infections (STIs) such as chlamydia, gonorrhea, or mycoplasma genitalium. These infections typically target the cervix and can be effectively treated with antibiotics. However, if left untreated or if the infection spreads beyond the cervix, it can lead to PID, causing inflammation in the pelvic region and potentially leading to severe complications.
Can you get PID without STD?
Although pelvic inflammatory disease (PID) is commonly associated with sexually transmitted diseases (STDs), it is possible to develop PID without having an STD. While STDs are a significant contributing factor to PID, there are other causes that can lead to the infection and swelling of the female reproductive organs. For instance, certain bacteria from the vagina, such as those responsible for bacterial vaginosis, can ascend into the upper genital tract and result in PID. Additionally, non-sexual factors like intrauterine device (IUD) use or previous pelvic surgeries can also increase the risk of developing PID even without an STD. Therefore, while STDs are a common cause, it is important to consider other potential sources when diagnosing PID.
PID is an inflammatory condition that affects different parts of the female reproductive system, including the vagina, uterus, fallopian tubes, and ovaries. It typically occurs as a result of a bacterial infection, but not exclusively due to STDs. Sexual activity can introduce bacteria into the reproductive organs, but other non-sexual factors can also lead to the development of PID. It is crucial for individuals experiencing symptoms of PID, such as pelvic pain, abnormal vaginal discharge, or fever, to seek medical attention and undergo thorough testing to identify the underlying cause, whether it be an STD or another source of infection. By understanding the diverse factors that contribute to PID, healthcare providers can provide appropriate treatment and guidance to patients.
How do you fix pelvic inflammatory disease?
Pelvic inflammatory disease (PID) can be treated with various types of antibiotics that can effectively cure the infection. However, it is important to note that antibiotic treatment does not undo any scarring that may have occurred due to the infection. This highlights the urgency for women to seek immediate medical care if they experience pelvic pain or any other symptoms of PID. Seeking prompt treatment not only helps in combating the infection but also reduces the risk of long-term complications associated with scarring.
Reference source
https://www.cdc.gov/std/pid/stdfact-pid.htm
https://www.womenshealth.gov/a-z-topics/pelvic-inflammatory-disease
https://www.nhs.uk/conditions/pelvic-inflammatory-disease-pid/causes/
https://www.medicinenet.com/pelvic_inflammatory_disease_without_having_an_std/article.htm