Perimenopause, often dubbed “the change,” is a phase in a woman’s life when her body begins the journey towards menopause.
It’s a time of transition that can bring about a myriad of physical and emotional changes, giving rise to a condition known as perimenopausal syndrome.
Curious to learn more about this fascinating stage?
Let’s delve into the mysteries of perimenopause and explore the ways to navigate its waves with grace and empowerment.
perimenopausal syndrome
Perimenopausal syndrome refers to the symptoms and physical changes that occur during the transitional phase before menopause.
This phase typically lasts for 4 to 8 years, beginning in a woman’s 40s or even earlier.
The most common symptom of perimenopause is hot flashes, which can last for 1 to 5 minutes and are often accompanied by a cold chill.
Night sweats, hot flashes that occur at night, can also disrupt sleep.
Other symptoms include irregular menstrual cycles, vaginal dryness, sleep problems, mood changes, bladder problems, and changes in sexual arousal and desire.
Treatment options for perimenopausal symptoms include lifestyle changes, over-the-counter remedies, hormone therapy, nonhormonal prescription drugs, and low-dose vaginal estrogen products.
It is important for women experiencing disruptive symptoms to seek evaluation and management from a doctor.
Key Points:
- Perimenopausal syndrome refers to symptoms and physical changes before menopause
- It typically lasts for 4 to 8 years, starting in a woman’s 40s or earlier
- The most common symptom is hot flashes, lasting 1 to 5 minutes and often accompanied by a cold chill
- Night sweats, hot flashes at night, can disrupt sleep
- Other symptoms include irregular menstrual cycles, vaginal dryness, sleep problems, mood changes, bladder problems, and changes in sexual arousal and desire
- Treatment options include:
- Lifestyle changes
- Over-the-counter remedies
- Hormone therapy
- Nonhormonal prescription drugs
- Low-dose vaginal estrogen products
perimenopausal syndrome – Watch Video
💡
Pro Tips:
1. Perimenopausal syndrome is a transitional phase experienced by women before entering menopause, typically in their late 40s or early 50s.
2. During perimenopause, hormonal fluctuations can affect mood and emotions, resulting in irritability, anxiety, and even panic attacks.
3. It is estimated that around 20-30% of women may experience perimenopausal syndrome to some degree, although the severity and duration can vary greatly from person to person.
4. Hot flashes are a common symptom of perimenopause, characterized by sudden and intense feelings of warmth, often accompanied by sweating and an increased heart rate.
5. While perimenopause usually lasts for a few years, it can extend longer for some women, with the average duration being around four years.
Age Range for Menopause
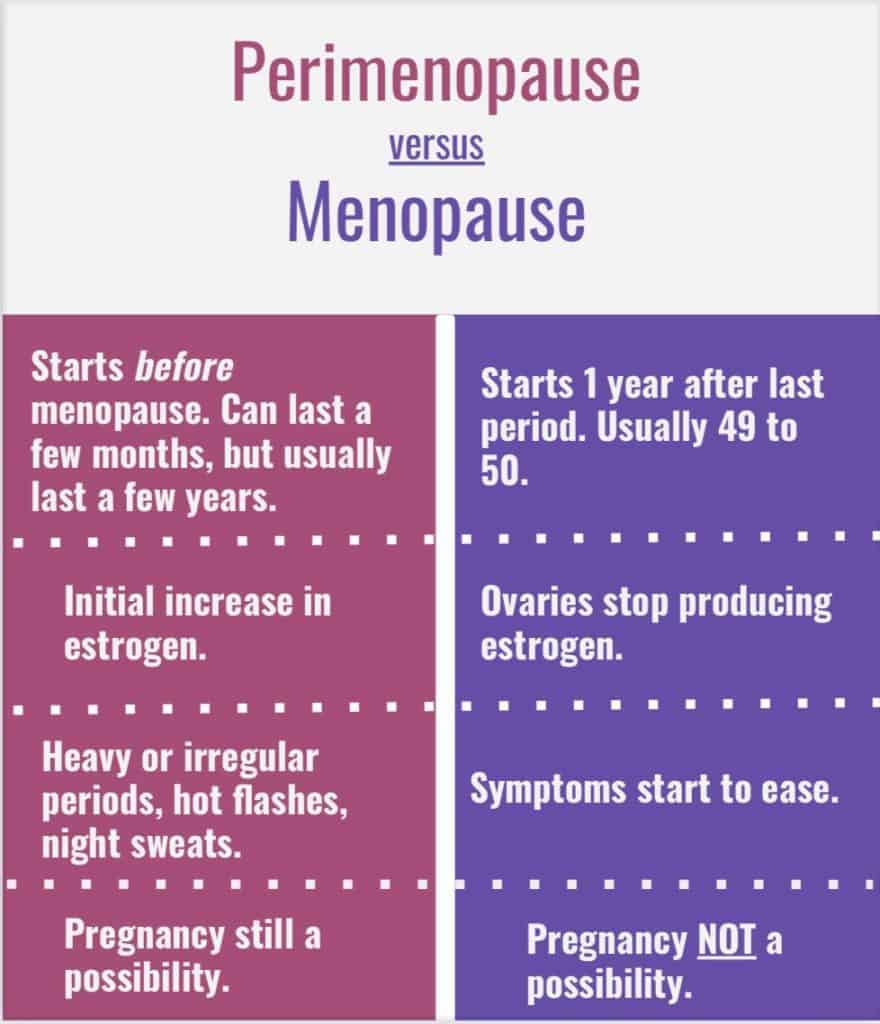
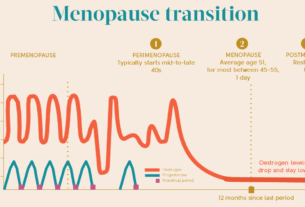
Menopause, the natural cessation of menstruation, typically occurs between the ages of 40 and 58, with an average age of 51. However, it is important to note that menopause is a transitional phase and not an abrupt event. The period leading up to menopause is known as perimenopause, which can last for 4 to 8 years.
During perimenopause, a woman’s hormone levels, particularly estrogen and progesterone, begin to fluctuate, leading to various physical and emotional changes.
Common symptoms during perimenopause include:
- Irregular menstrual cycles
- Hot flashes
- Sleep disturbances
- Vaginal dryness
- Mood changes
- Bladder problems
The severity of these symptoms may vary from woman to woman, with some experiencing no physical changes while others may be significantly affected. It’s important to understand that these changes are a natural part of the aging process and are generally considered normal. However, if the symptoms become disruptive or concerning, it is advisable to seek evaluation and management from a healthcare professional.
Note: Menopause is a normal transition phase in a woman’s life, characterized by the natural cessation of menstruation. During perimenopause, hormone levels fluctuate, leading to various physical and emotional changes.
Duration of Perimenopause
Perimenopause, the phase before menopause, can last for several years. On average, it spans between 4 to 8 years, although individual experiences may vary. During this time, hormone levels, especially estrogen, fluctuate irregularly, leading to changes in the menstrual cycle and various physical and emotional symptoms.
One of the hallmarks of perimenopause is the irregularity of menstrual periods. Women may experience shorter or longer cycles, skipped periods, or heavier or lighter bleeding. These fluctuations can be frustrating and may cause anxiety for some women.
It’s important to note that fertility decreases during perimenopause, but pregnancy is still possible until no periods occur for 12 consecutive months. Therefore, if pregnancy is not desired, it is essential to continue using contraception until menopause is confirmed.
- Perimenopause can last for several years.
- Hormone levels, especially estrogen, fluctuate irregularly.
- Menstrual cycles become irregular, with shorter or longer cycles, skipped periods, or heavier or lighter bleeding.
- Fertility decreases, but pregnancy is still possible until no periods occur for 12 consecutive months.
- It is important to use contraception until menopause is confirmed.
“Perimenopause is a phase before menopause that can last for several years. Hormone levels, especially estrogen, fluctuate irregularly during this time, leading to changes in the menstrual cycle and various physical and emotional symptoms.”
Factors Influencing Timing of Menopause
While the average age of menopause is 51, several factors can influence the timing of this natural transition. One such factor is genetics. Studies have shown that women with a family history of early or late menopause are more likely to experience menopause at a similar age. Genetic factors can play a significant role in determining the age at which a woman enters menopause.
Another factor that can influence the timing of natural menopause is smoking. Research has shown that smokers tend to experience menopause earlier than non-smokers. Smoking accelerates the decline of ovarian function, leading to an earlier depletion of eggs and subsequent menopause.
Apart from genetics and smoking, certain medical and surgical interventions, such as chemotherapy, pelvic radiation, and the removal of the ovaries, can induce premature menopause. However, these cases are not considered typical menopause but rather a medical intervention that leads to the cessation of ovarian function.
Common Symptom: Hot Flashes
Hot flashes are one of the most common and well-known symptoms of menopause. They typically manifest as a sudden sensation of heat spreading through the body, particularly the face, neck, and chest. Accompanying this sensation, some women may experience flushing or reddening of the skin, sweating, and a rapid heartbeat. The duration of a hot flash can range from 1 to 5 minutes, and it is often followed by a cold chill.
The exact cause of hot flashes is still not fully understood, but it is believed to be related to hormonal fluctuations, specifically the decline of estrogen levels during menopause. Thankfully, for most women, hot flashes decrease in frequency and intensity over time. However, for some women, they can be quite bothersome and disruptive to their daily lives.
Key points:
- Hot flashes are a common symptom of menopause.
- They cause a sudden sensation of heat, especially in the face, neck, and chest.
- Other symptoms may include flushing, sweating, and rapid heartbeat.
- Hot flashes typically last 1 to 5 minutes and may be followed by a cold chill.
- Hormonal fluctuations, particularly a decline in estrogen levels, are believed to be the cause.
- Hot flashes improve in frequency and intensity for most women over time.
- However, for some women, they can have a significant impact on daily life.
Hot flashes can be bothersome and disruptive.
Night Sweats and Sleep Disruption
Night sweats, which are essentially hot flashes that occur during sleep, can be particularly disruptive to a woman’s quality of sleep. Just like hot flashes, night sweats are characterized by a sudden sensation of heat and sweating, often followed by a cold chill.
The episodes of night sweats can be recurrent throughout the night, leading to frequent awakenings and difficulty falling back asleep. As a result, sleep disruption and daytime fatigue can become significant issues for menopausal women experiencing night sweats.
This lack of quality sleep can also contribute to mood changes, irritability, and difficulty concentrating, further exacerbating the impact on overall well-being.
The impact of night sweats on sleep quality during menopause is significant.
It is essential to address night sweats and prioritize strategies to improve sleep during menopause.
Strategies to improve sleep during menopause:
- Establish a regular sleep schedule
- Create a relaxing bedtime routine
- Ensure a comfortable sleep environment
- Avoid caffeine and alcohol close to bedtime
- Engage in regular exercise
- Try relaxation techniques such as deep breathing or meditation
By implementing these strategies, menopausal women can reduce the impact of night sweats on their sleep and overall well-being.
Treatment Options for Hot Flashes and Night Sweats
Fortunately, various treatment options are available to alleviate the symptoms of hot flashes and night sweats. The approach to treatment can vary depending on the severity of the symptoms and the individual’s preferences.
Lifestyle changes play a significant role in managing hot flashes and night sweats. It is recommended to avoid triggers like spicy foods, caffeine, alcohol, and hot drinks. Dressing in layers and using breathable fabrics can also help regulate body temperature. Engaging in stress-reducing activities, such as yoga, meditation, or deep breathing exercises, may also contribute to symptom relief.
For those seeking nonprescription remedies, plant-derived supplements like black cohosh, soy, and evening primrose oil have been suggested as potential options. However, it is important to consult with a healthcare provider before starting any new supplement to ensure safety and efficacy.
Hormone therapy, including estrogen and progesterone, can be prescribed to alleviate menopausal symptoms, including hot flashes and night sweats. However, the decision to undergo hormone therapy should be individualized and carefully weighed, taking into consideration the woman’s medical history, current health status, and personal preferences.
Nonhormonal prescription drugs, such as selective serotonin reuptake inhibitors (SSRIs) and selective norepinephrine reuptake inhibitors (SNRIs), have also been shown to provide relief for hot flashes. These medications, typically used to treat depression or anxiety, can be prescribed at lower doses specifically targeting menopause symptoms.
It is advisable to discuss the various treatment options with a healthcare provider to determine what approach is most suitable based on individual circumstances and preferences.
- Lifestyle changes can help manage hot flashes and night sweats.
- Plant-derived supplements like black cohosh, soy, and evening primrose oil are potential nonprescription remedies.
- Hormone therapy, including estrogen and progesterone, should be carefully considered.
- Nonhormonal prescription drugs like SSRIs and SNRIs may provide relief.
- Consultation with a healthcare provider is recommended.
Vaginal Atrophy and Dryness
During menopause, declining estrogen levels can result in vaginal atrophy, which leads to thinning, dryness, and reduced elasticity of vaginal tissues. This condition can cause symptoms like vaginal dryness, itching, and discomfort. Dyspareunia, or pain during sexual intercourse, is also a common problem.
Vaginal atrophy can have a significant impact on a woman’s quality of life and sexual intimacy. Fortunately, there are self-care strategies and treatment options available to alleviate these symptoms and restore comfort.
Over-The-Counter Remedies for Pain During Intercourse
For women who experience pain during intercourse due to vaginal dryness and atrophy, over-the-counter lubricants and moisturizers can offer relief. Lubricants work by reducing friction during sexual activity and can be applied directly before intercourse. Moisturizers, on the other hand, are designed to hydrate and restore the vagina’s natural moisture over time. They can be used regularly.
When selecting products, it is crucial to choose ones specifically designed for vaginal use. Avoid scented or perfumed products as they can irritate the delicate vaginal tissues. It may be necessary to experiment with different brands and types of lubricants and moisturizers to find the most effective option for individual needs.
If over-the-counter remedies do not provide sufficient relief, it is recommended to consult with a healthcare provider. They may prescribe low-dose vaginal estrogen products, such as creams or rings, which can help restore the structure and function of the vaginal tissues.
Severe Symptoms and Low-Dose Vaginal Estrogen Products
When perimenopausal symptoms, particularly vaginal atrophy, become severe and significantly impact a woman’s quality of life, low-dose vaginal estrogen products may be necessary. These products deliver a localized dose of estrogen directly to the vaginal tissues, helping to restore moisture, elasticity, and comfort.
It is important to note that low-dose vaginal estrogen products differ from systemic hormone therapy, as they only act locally in the vaginal area and have minimal absorption into the bloodstream. Therefore, they carry lower risks compared to systemic estrogen therapy and can be a safe and effective option for women experiencing troublesome vaginal symptoms.
As with any medication, it is important to discuss the potential risks and benefits with a healthcare provider to determine the most suitable approach for individual needs.
Definition and Diagnosis of Perimenopausal Syndrome
Perimenopausal syndrome is the term used to describe the period in a woman’s life when she begins experiencing the symptoms associated with menopause. A definitive diagnosis of perimenopause is made when a woman has missed her period for 12 consecutive months without any other identifiable causes.
It’s important to understand that each woman’s experience of menopause is unique. While some women may transition through perimenopause with minimal physical changes or discomfort, others may experience a range of symptoms, including hot flashes, night sweats, vaginal changes, mood swings, and sleep disturbances.
While the severity and duration of perimenopausal symptoms can vary, they are generally considered a natural and normal part of the aging process. However, if these symptoms become disruptive or concerning, it is advisable to seek evaluation and management from a healthcare professional, who can provide appropriate guidance and treatment options.
💡
You may need to know these questions about perimenopausal syndrome
What are the first signs of perimenopause?
The initial indicators of perimenopause often encompass changes in menstrual cycles, including unpredictable lengthening or shortening. One may encounter cycles where ovulation does not occur, causing a disruption in the release of eggs by the ovaries. Furthermore, menopause-like symptoms such as hot flashes, sleep disturbances, and vaginal dryness can manifest during this phase. Fortunately, various treatments exist to mitigate and alleviate these symptoms, offering relief and support during perimenopause.
What is the typical age for perimenopause?
Perimenopause, a phase preceding the final menstrual cycle, typically commences a few years beforehand. This transitional period spans two stages, with the early stage generally commencing in women aged 40 to 44, though it can begin as early as the 30s. As women embark on this transformative journey, their reproductive system undergoes gradual changes leading up to menopause.
What are the 4 phases of perimenopause?
Perimenopause, the transitional phase leading to menopause, can be divided into four distinct phases. The first phase is characterized by regular periods, despite being in the early stages of perimenopause. This phase may bring some subtle changes but is generally marked by the continuation of a woman’s usual menstrual cycle.
The second phase, known as the early menopause transition, begins when irregular periods emerge. Women may experience changes in the duration and flow of their menstrual cycles during this phase. The third phase, the late menopause transition, commences with the occurrence of cycles longer than 60 days. As the body adjusts to hormonal shifts, these longer periods can be seen as an indication of progressing perimenopause. Finally, the late perimenopause phase arrives when twelve consecutive months have passed since a woman’s final period. At this point, menopause is considered complete, and the woman enters into the postmenopausal stage.
What is the difference between premenopause and perimenopause?
Premenopause and perimenopause represent different stages in a woman’s reproductive life. Premenopause refers to the period between a woman’s first period and the start of perimenopause, marking the beginning of her menstrual cycles. During this phase, a woman’s hormones are generally balanced, and she experiences regular menstrual cycles. On the other hand, perimenopause is the transitional phase leading up to menopause, usually lasting around six years. It commonly occurs in women aged 40s to early 50s and is characterized by hormonal fluctuations and irregular periods. This stage marks the decline in a woman’s fertility as her body prepares for menopause. Overall, premenopause represents the onset of menstrual cycles, while perimenopause signifies the shift towards the end of reproductive years.
Reference source
https://www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666
https://www.mountsinai.org/health-library/report/menopause
https://future-woman.com/four-stages-perimenopause/
https://www.pennmedicine.org/updates/blogs/womens-health/2016/december/the-change-before-the-change