Every expectant mother dreams of a smooth and safe pregnancy journey, but sometimes, unforeseen complications can arise.
One such complication is placenta accreta, a condition that strikes fear into the hearts of doctors and expectant mothers alike.
In this brief glimpse into the world of placenta accreta, we will explore the dangers it poses and shed light on the struggles faced by those affected.
Brace yourself for a captivating tale of resilience and medical marvels as we delve deeper into the mysteries of this perilous condition.
placenta accreta
Placenta accreta is a serious pregnancy condition in which the placenta grows too deeply into the uterine wall.
This condition occurs when part or all of the placenta remains attached after childbirth, which can cause severe blood loss.
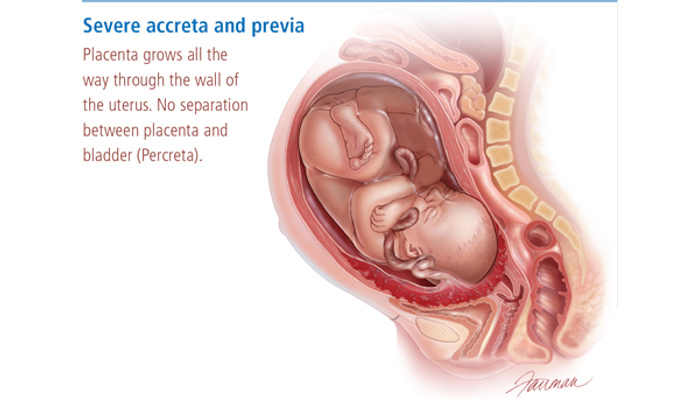
In more severe cases, the placenta can invade the muscles of the uterus (placenta increta) or grow through the uterine wall (placenta percreta).
Key Points:
- Placenta accreta is a condition where the placenta grows too deeply into the uterine wall during pregnancy.
- It can cause severe blood loss after childbirth if part or all of the placenta remains attached.
- In more severe cases, the condition can lead to placenta increta, where the placenta invades the muscles of the uterus.
- It can also result in placenta percreta, where the placenta grows through the uterine wall.
- Placenta accreta is a serious pregnancy condition.
- It requires medical intervention to manage and avoid complications.
placenta accreta – Watch Video
💡
Pro Tips:
1. Placenta accreta occurs when the placenta attaches too deeply into the uterine wall, making it difficult to detach during childbirth. This condition can potentially lead to life-threatening complications for both the mother and the baby.
2. Placenta accreta is often associated with previous uterine surgeries, such as cesarean sections or the removal of fibroids. These interventions can weaken the uterine lining, making it more prone to abnormal placenta growth.
3. While placenta accreta is relatively rare, its prevalence has been increasing over the past few decades, possibly due to the rising rates of cesarean deliveries and other uterine surgeries.
4. Placenta accreta can result in excessive bleeding during delivery, prompting the need for a hysterectomy to stop the hemorrhage. This means that women with placenta accreta will likely lose their fertility after childbirth.
5. To minimize the risks associated with placenta accreta, healthcare providers may use various diagnostic techniques, such as ultrasound and MRI, to identify the condition during pregnancy. This allows for better planning and preparation for delivery, ensuring that the appropriate medical team and resources are available to manage the situation effectively.
Definition Of Placenta Accreta
Placenta accreta is a serious pregnancy condition where the placenta grows too deeply into the uterine wall. After childbirth, it is normal for the placenta to detach and be expelled from the body. However, in cases of placenta accreta, part or all of the placenta remains attached. This can result in complications during and after delivery, as the placenta cannot be easily removed.
- Placenta accreta is a condition where the placenta grows too deeply into the uterine wall.
- After childbirth, the placenta should detach and be expelled from the body.
- In cases of placenta accreta, the placenta remains attached, leading to complications.
- The inability to fully remove the placenta can result in risks during and after delivery.
Placenta accreta is a serious condition where the placenta grows deeply into the uterine wall and remains attached, causing complications.
How Placenta Accreta Differs From A Normal Placenta
In a normal pregnancy, the placenta is attached to the uterine wall but can be easily separated during childbirth. However, with placenta accreta, the placenta invades the uterine wall more deeply than normal. This can cause it to become firmly embedded and difficult to detach. In some cases, the placenta can even invade the muscles of the uterus (placenta increta) or grow through the uterine wall and attach to nearby organs (placenta percreta). These variations of placenta accreta are even more dangerous and can result in significant complications.
Risks Associated With Placenta Accreta
Placenta accreta is a condition that carries significant risks for both the mother and the baby. The most alarming risk is severe blood loss following childbirth. Due to the difficulty in removing the placenta, attempts to detach it can result in excessive bleeding, potentially leading to hemorrhage. In severe cases, this may necessitate blood transfusions and emergency surgical interventions to control the bleeding. Additionally, placenta accreta raises the likelihood of developing infections and encountering complications like blood clots and organ damage.
Symptoms Of Placenta Accreta
In some cases, placenta accreta may not present any symptoms during pregnancy. However, common symptoms can include:
- Abnormal vaginal bleeding, particularly in the third trimester
- Bleeding after delivery that is difficult to control
- Pain or discomfort in the pelvis
- Enlarged uterus
- Difficulty during labor
It is important to note that placenta accreta is often diagnosed during routine prenatal screenings or after delivery, as the symptoms can be similar to other pregnancy complications.
Factors That Increase The Risk Of Placenta Accreta
There are several risk factors associated with the development of placenta accreta:
- Women who have previous cesarean sections or other uterine surgeries are at a higher risk.
- Women with placenta previa, characterized by the placenta covering the cervix, are also more likely to develop placenta accreta.
- Advanced maternal age can increase the risk.
- Multiple pregnancies, such as twins or triplets, are a contributing factor.
- Certain medical conditions like chronic hypertension or diabetes can also increase the risk of placenta accreta.
Please remember to consult with a healthcare professional for personalized advice and management options.
Note: Placenta accreta is a serious medical condition that requires appropriate medical attention and care.
Diagnosis And Testing For Placenta Accreta
Diagnosing placenta accreta can be challenging as the condition may not present noticeable symptoms. However, prenatal ultrasounds and other imaging techniques can be used to identify placenta accreta. These tests can show the location and depth of the placenta, providing valuable information for healthcare providers. Additionally, blood tests may be conducted to measure certain markers associated with placenta accreta, such as alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG) levels.
- Prenatal ultrasounds and imaging techniques can be used to identify placenta accreta by showing the location and depth of the placenta.
- Blood tests, including AFP and hCG levels, can provide additional information to assist in diagnosing placenta accreta.
Management And Treatment Options For Placenta Accreta
Managing placenta accreta involves careful planning and coordination between healthcare providers. In many cases, delivery is scheduled before the due date to minimize the risk of complications. A team of specialists, including obstetricians, hematologists, and anesthesiologists, may be involved in the delivery to ensure the safety of both the mother and the baby. Treatment options may include blood transfusions, medications to control bleeding, and surgical interventions to remove the placenta or repair the uterus.
Potential Complications Of Placenta Accreta
Placenta accreta is a condition that can have serious consequences if not properly managed. The most immediate concern is excessive bleeding, also known as postpartum hemorrhage, which can lead to a life-threatening condition called hypovolemic shock due to severe blood loss. In certain cases, emergency hysterectomy, the surgical removal of the uterus, may be necessary to stop the bleeding. Moreover, placenta accreta can heighten the risk of infection and result in long-term complications like infertility or uterine scarring.
Long-Term Effects Of Placenta Accreta
The long-term effects of placenta accreta can vary depending on the severity of the condition and the interventions required.
Some key points to note include:
- For some women, there may be no long-term effects after treatment.
- However, others may experience complications such as:
- Chronic pelvic pain
- Abnormal vaginal bleeding
- Difficulties with future pregnancies
- Women who have undergone emergency hysterectomies may experience emotional and psychological effects, such as:
- Grief
- Feelings of loss
It is important to highlight that support from healthcare professionals and counseling services can be beneficial in addressing these concerns.
Prevention And Awareness Of Placenta Accreta
Placenta accreta, a condition where the placenta grows too deeply into the uterine wall, cannot be prevented entirely. However, there are measures that can help reduce the risks associated with this condition.
To improve outcomes, it is important to:
- Ensure proper prenatal care to closely monitor the pregnancy and detect any potential risk factors early on.
- Use prenatal ultrasounds and other imaging tests to identify placenta accreta and provide appropriate care as needed.
- Raise awareness about placenta accreta among healthcare providers, pregnant women, and the general public to promote early detection and prompt intervention.
By following these measures, we can improve outcomes for both mothers and babies affected by placenta accreta.
💡
You may need to know these questions about placenta accreta
How serious is placenta accreta?
Placenta accreta is a potentially life-threatening condition that should be taken very seriously. It can result in severe vaginal bleeding after delivery, which poses a significant risk to the mother. This bleeding can lead to complications such as disseminated intravascular coagulopathy, where the blood fails to clot properly, and respiratory and kidney failure. These potential complications highlight the seriousness of placenta accreta, emphasizing the importance of prompt medical attention and intervention to mitigate the risks associated with this condition.
What is the survival rate of placenta accreta mother?
The survival rate of placenta accreta mothers can vary depending on various factors. Previous studies have suggested a mortality rate of accreta as high as 7%, indicating a significant risk involved. However, it is important to note that advancements in medical technology, improved surgical techniques, and increased awareness may have positively impacted the survival rate of mothers diagnosed with placenta accreta in recent years. While exact survival rates may not be readily available, it is encouraging to consider the potential for improved outcomes in the present medical landscape.
What is the most common cause of placenta accreta?
Placenta accreta spectrum is most commonly caused by previous cesarean deliveries, making it imperative to consider the number of prior cesarean deliveries as a major risk factor. Studies show that the incidence of placenta accreta spectrum tends to rise as the number of cesarean deliveries increases. This information highlights the importance of a careful consideration and monitoring of patients with a history of cesarean deliveries to prevent and manage this condition effectively.
Can you have a healthy baby with placenta accreta?
While placenta accreta can be a concerning condition, it is still possible to have a healthy baby. With proper management and timely medical intervention, the risks associated with preterm birth can be minimized. Close monitoring during pregnancy, early detection of the condition, and collaboration between obstetricians and neonatologists can significantly increase the chances of a healthy baby being delivered, potentially avoiding the need for admission to a neonatal intensive care unit (NICU). Each case is unique, and it is crucial to consult with healthcare professionals to ensure the best possible outcome for both the mother and the baby.
Reference source
https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/placenta-accreta
https://www.mayoclinic.org/diseases-conditions/placenta-accreta/symptoms-causes/syc-20376431
https://www.mayoclinic.org/diseases-conditions/placenta-accreta/symptoms-causes/syc-20376431
https://www.preventaccreta.org/faq