Throughout history, pregnancy has been a remarkable journey filled with joy and anticipation.
However, adventures can sometimes take unexpected turns.
Imagine the awe of creating life, only to discover that the delicate connection between mother and child, the placenta, has decided to rewrite the script.
Placenta previa, a captivating yet challenging condition, introduces a startling obstacle that demands our attention.
Join us as we delve into the world of placenta previa, uncovering its secrets and exploring the remarkable resilience of both mothers and their unborn miracles.
placenta previa
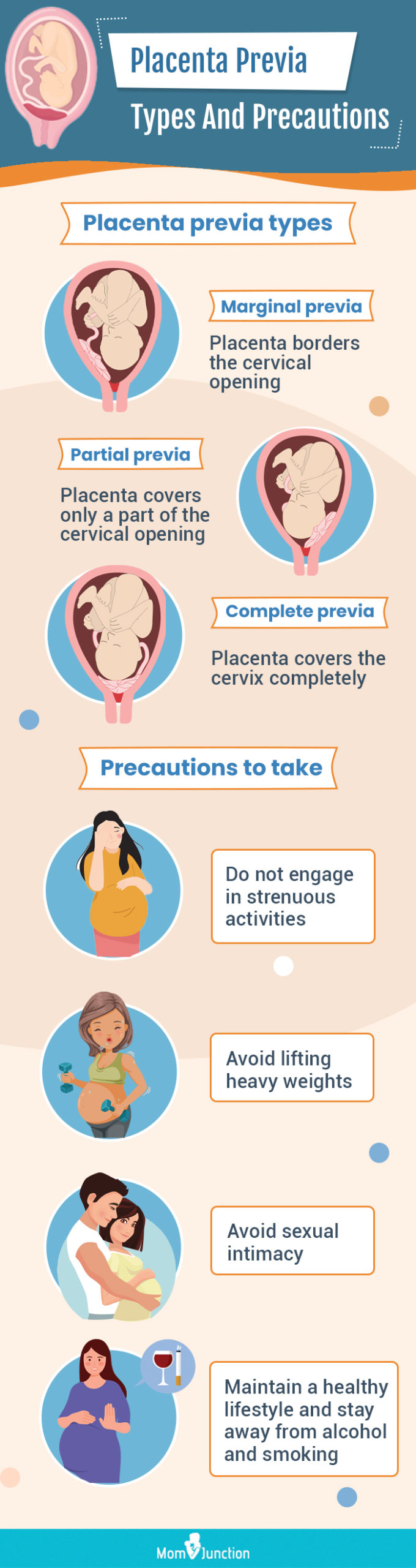
Placenta previa is a condition where the placenta covers all or part of the opening to the cervical opening at the top of the vagina.
It occurs in about 1 in 200 pregnancies and can lead to serious bleeding and complications later in pregnancy.
Risk factors for placenta previa include previous c-section, in vitro fertilization, smoking, cocaine use, age 35 or older, previous pregnancies, multiple pregnancies, and previous episodes of placenta previa.
Symptoms may include painless bleeding from the vagina during the second half of pregnancy and contractions.
Diagnosis is typically done through a routine ultrasound test, including transvaginal and translabial ultrasounds.
Treatment depends on the stage of pregnancy, severity of bleeding, and the health of the mother and baby.
In most cases, a c-section is recommended to prevent severe bleeding.
Close monitoring in the hospital and blood transfusions may be necessary for excessive bleeding.
Corticosteroids may be given to help with the baby’s lung development if preterm delivery is expected.
Certain activities should be avoided, such as orgasm-inducing sex, vaginal penetration or examinations, moderate/strenuous exercise, lifting more than 20 pounds, and standing for more than four hours.
Key Points:
- Placenta previa is when the placenta partially or fully covers the cervical opening at the top of the vagina.
- It occurs in 1 in 200 pregnancies and can lead to serious bleeding and complications.
- Risk factors for placenta previa include previous c-section, in vitro fertilization, smoking, cocaine use, age 35 or older, previous pregnancies, multiple pregnancies, and previous episodes of placenta previa.
- Symptoms may include painless bleeding during the second half of pregnancy and contractions.
- Diagnosis is typically done through routine ultrasound tests, including transvaginal and translabial ultrasounds.
- Treatment depends on the stage of pregnancy, severity of bleeding, and the health of the mother and baby, with c-section being the most common recommendation.
placenta previa – Watch Video
💡
Pro Tips:
1. Placenta previa, a condition where the placenta partially or completely covers the cervix, occurs in approximately 1 in 200 pregnancies.
2. Placenta previa is more common in women who have had previous pregnancies, cesarean sections, or other uterine surgery.
3. In some cases, placenta previa can be detected during a routine ultrasound in the second trimester of pregnancy.
4. Women with placenta previa may experience painless vaginal bleeding, particularly in the third trimester, due to the placenta’s proximity to the cervix.
5. Placenta previa can increase the risk of complications during childbirth, such as excessive bleeding, premature birth, and the need for a cesarean section.
Introduction to Placenta Previa
Placenta previa is a medical condition that occurs during pregnancy when the placenta, which normally attaches to the uterine wall, covers all or part of the cervical opening at the top of the vagina. This can lead to serious complications and is a major concern in the medical field. Expectant mothers should be knowledgeable about the risks, symptoms, and treatment options related to placenta previa in order to have a safe pregnancy and delivery.
Incidence and Prevalence of Placenta Previa
Placenta previa is a relatively uncommon condition, affecting around 1 in 200 pregnancies. Despite its low incidence rate, it should not be underestimated due to the potential for severe bleeding and other complications later in pregnancy. The prevalence of placenta previa can vary based on factors such as the specific population being studied and the presence of risk factors within that group.
- Placenta previa occurs in approximately 1 in 200 pregnancies.
- The condition can lead to severe bleeding and other complications.
- The prevalence of placenta previa varies depending on the population and presence of risk factors.
Potential Complications and Risks
Placenta previa is a condition that can have serious implications for both the mother and the baby. The most alarming complication that arises from this condition is the occurrence of severe bleeding, which can happen in the later stages of pregnancy or during labor. This can put the lives of both the mother and the baby at risk, necessitating immediate medical intervention.
In addition to the risk of bleeding, placenta previa increases the likelihood of preterm birth. The placenta may not be able to adequately support the baby’s growth, resulting in premature delivery.
There are other potential complications associated with placenta previa as well. One such complication is placenta accreta, wherein the placenta attaches itself too deeply to the uterine wall. This can lead to difficulties during delivery and may require medical assistance.
Furthermore, placenta previa can also result in fetal growth restriction, impacting the baby’s development.
To summarize the potential risks of placenta previa:
- Severe bleeding, which can be life-threatening
- Increased risk of preterm birth
- Placenta accreta, when the placenta attaches too deeply to the uterine wall
- Fetal growth restriction
It is crucial for expectant mothers with placenta previa to receive specialized prenatal care and to be closely monitored throughout their pregnancy to ensure the best possible outcomes for both the mother and the baby.
Identifying Risk Factors for Placenta Previa
Risk factors for placenta previa:
- Previous cesarean section deliveries
- In vitro fertilization
- Smoking
- Cocaine use
- Maternal age of 35 or older
- Previous pregnancies
- Multiple pregnancies (such as twins or triplets)
- History of placenta previa in previous pregnancies
Pregnant women should be aware of these risk factors and consult with their healthcare providers for appropriate monitoring and management.
Common Symptoms and Signs of Placenta Previa
One of the primary symptoms of placenta previa is painless bleeding from the vagina during the second half of pregnancy. This bleeding can be light or heavy and may occur intermittently. Another symptom that may indicate placenta previa is contractions, which are not to be confused with normal pregnancy contractions.
These signs should not be ignored and should be reported to a healthcare professional immediately for further evaluation.
- Painless bleeding from the vagina during the second half of pregnancy
- Bleeding can be light or heavy and may occur intermittently
- Contractions that are not to be confused with normal pregnancy contractions
“These signs should not be ignored and should be reported to a healthcare professional immediately for further evaluation.”
Diagnostic Methods for Evaluating Placenta Previa
The diagnosis of placenta previa is typically made through a routine ultrasound test. This non-invasive imaging technique allows healthcare providers to visualize the position of the placenta in relation to the cervical opening. Ultrasound is considered the gold standard for diagnosing placenta previa due to its accuracy and safety. In some cases, additional diagnostic methods, such as magnetic resonance imaging (MRI) or physical examination, may be used to confirm the diagnosis or evaluate further complications.
- Ultrasound: non-invasive imaging technique
- MRI: additional diagnostic method
- Physical examination: used for diagnosis confirmation or complications evaluation
Various Types of Ultrasound Used for Detection
Different types of ultrasound can be used to detect and evaluate placenta previa. Two commonly used types are transvaginal ultrasound and translabial ultrasound, which provide detailed images of the pelvic area and the placenta. Another technique that can be employed is three-dimensional ultrasound, which provides a three-dimensional image of the placenta’s position and its proximity to the cervical opening. These ultrasound techniques are safe, non-invasive, and crucial in diagnosing and monitoring placenta previa during pregnancy.
- Transvaginal ultrasound
- Translabial ultrasound
- Three-dimensional ultrasound
“These ultrasound techniques are safe, non-invasive, and play a crucial role in diagnosing and monitoring placenta previa during pregnancy.”
Importance of Early Detection During the Second Trimester
It is essential to detect placenta previa early, preferably during the second trimester, to allow for appropriate monitoring and management. Even in the absence of vaginal bleeding, routine ultrasound examinations can identify the condition. This early detection provides an opportunity for healthcare providers to assess the risk factors, evaluate the severity of placenta previa, and plan for necessary interventions or precautions to ensure the safety of both mother and baby throughout the remainder of the pregnancy.
Treatment Options Based on Individual Circumstances
The treatment of placenta previa depends on various factors, including the stage of pregnancy, the severity of bleeding, and the overall health of the mother and baby. In most cases, a cesarean section delivery is recommended to prevent severe bleeding during labor. However, treatment plans may vary based on individual circumstances.
For instance, if placenta previa is detected early in pregnancy without symptoms, close monitoring and follow-up ultrasounds may be the primary course of action.
Precautions and Lifestyle Adjustments with Placenta Previa
To minimize the risk of complications and worsen the condition of placenta previa, individuals diagnosed with this condition should follow certain precautions and make lifestyle adjustments. These include:
-
Avoiding orgasm-inducing sexual activities: Engaging in sexual activities that may lead to orgasm can increase the risk of bleeding and potentially worsen the condition. It is advisable to abstain from such activities to minimize these risks.
-
Refraining from vaginal penetration or examinations: The vagina is a sensitive area, and any form of penetration or examination can potentially lead to bleeding or injury to the placenta. It is important to avoid these activities to prevent complications.
-
Limiting moderate to strenuous exercise: Engaging in vigorous physical activity can put strain on the placenta and lead to bleeding. It is recommended to restrict exercise to low-impact or light activities to avoid exacerbating the condition.
-
Avoiding heavy lifting (more than 20 pounds): Lifting heavy objects can increase intra-abdominal pressure, which may result in bleeding for individuals with placenta previa. It is advisable to avoid lifting anything heavier than 20 pounds to minimize the risk of complications.
-
Limiting standing for longer than four hours: Prolonged periods of standing can put pressure on the placenta and potentially lead to bleeding. Individuals should try to avoid staying in a standing position for more than four hours at a time.
By adhering to these precautions, individuals with placenta previa can help reduce the chances of bleeding and mitigate other detrimental consequences associated with this condition.
💡
You may need to know these questions about placenta previa
Can a baby survive placenta previa?
Placenta previa is a manageable condition, and with proper care and guidance from pregnancy care providers, the chances of a safe delivery are high. However, in some cases, depending on the severity of the condition and other factors, a baby’s survival may be at risk. It is crucial for pregnant individuals experiencing any bleeding or discomfort to communicate this to their healthcare provider promptly to ensure appropriate intervention and support for the baby’s well-being. Early detection and timely medical attention increase the likelihood of a successful outcome for both the baby and the parent.
How serious is placenta previa?
Placenta previa is a serious condition that requires close monitoring and care throughout the pregnancy. One of the most concerning complications is severe vaginal bleeding, which can be life-threatening for both the mother and the baby. This bleeding can occur at any point during the pregnancy, labor, delivery, or shortly after giving birth. Additionally, there is a heightened risk of preterm birth, which brings its own set of challenges and complications. It is crucial for healthcare providers to carefully monitor individuals with placenta previa to minimize these serious risks and ensure the well-being of both the mother and the baby.
What is the main cause of placenta previa?
Placenta previa, a condition where the placenta partially or fully covers the cervix, can primarily be attributed to low implantation of the fertilized egg. This phenomenon occurs when the egg attaches itself in the lower part of the uterus rather than higher up, leading to the placenta obstructing the opening of the cervix. In addition to low implantation, conditions such as abnormalities in the uterine lining, such as fibroids, or scarring of the uterine lining (endometrium) can also contribute to the development of placenta previa. These factors disrupt the normal architecture of the uterus, affecting the position and proper development of the placenta.
How long can you carry a baby with placenta previa?
The duration for carrying a baby with placenta previa relies on several factors such as the risk of bleeding and the gestational age of the baby. In cases where the risk of bleeding outweighs the benefits of carrying the baby to full term, delivery may be recommended after 36 weeks. Typically, a C-section is performed for nearly all women with placenta previa as the preferred method of delivery.
Reference source
https://www.marchofdimes.org/find-support/topics/pregnancy/placenta-previa
https://my.clevelandclinic.org/health/diseases/24211-placenta-previa
https://www.mayoclinic.org/diseases-conditions/placenta-previa/symptoms-causes/syc-20352768
https://www.betterhealth.vic.gov.au/health/healthyliving/placenta-previa