The anticipation of a new life approaching its due date fills the heart with excitement and joy.
But what happens when that due date comes and goes, and the little one still hasn’t made an appearance?
Enter the enigmatic world of postterm delivery, where the journey of pregnancy takes an unexpected turn.
Join us as we explore the mysteries and complexities behind this fascinating phenomenon.
postterm delivery
Postterm delivery refers to a pregnancy that extends beyond the gestational age of 42 weeks, which is more than two weeks beyond the estimated due date.
This condition poses potential risks to both the mother and the baby.
Key Points:
- Postterm delivery occurs when a pregnancy extends beyond 42 weeks gestational age
- This is more than two weeks past the estimated due date
- There are potential risks involved for both the mother and the baby
- It is important to monitor postterm pregnancies closely
- Healthcare professionals should be aware of the potential complications that can arise
- Prompt delivery may be necessary in some cases to prevent adverse outcomes
postterm delivery – Watch Video
💡
Pro Tips:
1. Postterm delivery, also known as postmaturity syndrome, occurs when a baby is born after the 42nd week of pregnancy.
2. Studies have shown that postterm delivery is more common in first-time mothers, older mothers, and mothers with a family history of late deliveries.
3. Postterm babies are often larger in size, as they have had more time to grow in the womb. This can increase the risk of complications during delivery.
4. Babies born after the due date have a higher chance of experiencing meconium aspiration, where they inhale the first stool (meconium) in the womb. This can lead to respiratory issues and require immediate medical attention.
5. Postterm deliveries may be associated with an increased risk of stillbirth, as the placenta may start to deteriorate after the due date, affecting the supply of oxygen and nutrients to the baby.
Definition Of Postterm Delivery
Postterm delivery is when a pregnancy lasts beyond the standard 42-week mark. This occurs in about 5-10% of pregnancies. Postterm babies are at a higher risk of complications, which highlights the importance of understanding the risks.
Risk Factors For Postterm Delivery
Several factors contribute to the likelihood of a postterm delivery. One of the main risk factors is a history of previous postterm pregnancies. Women who have experienced postterm delivery in the past have a higher chance of recurrence. Other risk factors include:
- Maternal age above 35
- First-time motherhood
- Genetics
- Underlying health conditions such as diabetes or obesity
- Certain ethnic backgrounds.
Therefore, it is important to consider these factors when assessing the likelihood of a postterm delivery.-*
Complications Associated With Postterm Delivery
Postterm delivery is associated with several risks and complications for both the baby and the mother. The most significant concern is the increased chance of stillbirth as the placenta may not function optimally after the 42-week mark.
Furthermore, postterm babies may experience meconium aspiration syndrome, a condition in which they inhale amniotic fluid stained with meconium. This can lead to respiratory problems.
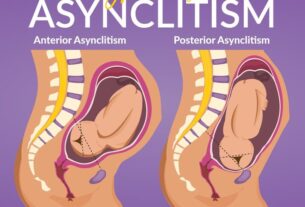
For women who go beyond their due date, there is a higher risk of complications during labor. These can include prolonged labor, difficulty with fetal positioning, and the need for assisted delivery methods like forceps or vacuum extraction.
To summarize, postterm delivery brings about potential risks such as stillbirth, meconium aspiration syndrome, and complications during labor. It is important for healthcare providers to closely monitor pregnancies that have exceeded the expected due date.
- Increased chance of stillbirth after the 42-week mark
- Meconium aspiration syndrome and respiratory problems
- Higher risk of prolonged labor, fetal positioning difficulties, and need for assisted delivery methods
Inducing Labor For Postterm Deliveries
When a pregnancy enters the postterm period, healthcare providers may recommend inducing labor to mitigate potential risks. Inducing labor typically involves the use of medications or techniques to initiate contractions and prompt childbirth. This process can help prevent complications associated with postterm deliveries. The timing and method of induction vary depending on the individual situation and medical history. It is essential for expectant mothers to discuss the benefits and risks of induction with their healthcare provider to make an informed decision.
Monitoring Fetal Well-Being In Postterm Pregnancies
Throughout a postterm pregnancy, regular monitoring of fetal well-being is crucial to identify potential issues. Healthcare providers may utilize various techniques, including non-stress tests, biophysical profiles, and umbilical cord blood flow studies, to assess the baby’s condition. These tests help evaluate the baby’s heart rate, movement, breathing, and overall well-being. Regular monitoring ensures prompt detection of indications of distress or complications, allowing for appropriate intervention to safeguard the baby’s health.
- Regular monitoring of fetal well-being is crucial to identify potential issues
- Techniques such as non-stress tests, biophysical profiles, and umbilical cord blood flow studies are used to assess the baby’s condition
- These tests evaluate the baby’s heart rate, movement, breathing, and overall well-being
- Prompt detection of indications of distress or complications is enabled through regular monitoring
- Appropriate intervention can be undertaken to safeguard the baby’s health.
Benefits Of Elective Induction For Postterm Deliveries
Elective induction, where labor is induced without a medical necessity, can offer certain benefits for postterm deliveries. It helps prevent complications associated with going beyond the due date, reducing the risk of stillbirth and meconium aspiration syndrome. Elective induction also allows for better control of the labor process, ensuring closer supervision and timely intervention if required. It provides expectant mothers and healthcare providers with peace of mind and allows for a more predictable and manageable birth experience.
Risks Of Waiting For Spontaneous Labor In Postterm Pregnancies
While waiting for spontaneous labor to commence after the due date may seem like a natural approach, there are potential risks associated with delaying delivery in postterm pregnancies. As the pregnancy progresses, the placenta’s function may decline, compromising the baby’s oxygen and nutrient supply. This increases the risk of stillbirth and birth complications. Furthermore, waiting for spontaneous labor can lead to anxiety and stress for expectant mothers, who may be concerned about the well-being of their baby. It is essential to balance the benefits of waiting against the potential risks and closely monitor the pregnancy if a spontaneous labor approach is chosen.
- Delaying delivery in postterm pregnancies can pose risks such as compromised oxygen and nutrient supply to the baby.
- The risk of stillbirth and birth complications increases with prolonged waiting for spontaneous labor.
- Expectant mothers may experience anxiety and stress while waiting for labor.
- Balancing the benefits and risks of waiting is crucial, with close monitoring of the pregnancy.
“While waiting for spontaneous labor to commence after the due date may seem like a natural approach, there are potential risks associated with delaying delivery in postterm pregnancies.”
Preparing For A Postterm Delivery
Expectant mothers in the postterm period should take necessary steps to ensure a safe and smooth delivery. This involves keeping in regular contact with their healthcare provider and attending prenatal appointments. It is crucial to promptly address any concerns or symptoms. Creating a birth plan that outlines preferences and options for labor and delivery can help expectant mothers feel more empowered and prepared. Furthermore, organizing support systems, such as a trusted labor partner or a doula, can offer emotional and physical assistance throughout the birth process.
Postpartum Care For Postterm Deliveries
Postpartum care for postterm deliveries is essential to promote both the mother’s and baby’s well-being. This includes:
- Monitoring for any signs of postpartum complications
- Promoting breastfeeding
- Addressing any physical and emotional changes that occur during the postpartum period.
Regular check-ups with healthcare providers after delivery ensure that any issues are promptly detected and addressed. Mothers may find it helpful to join support groups or engage in postpartum activities to connect with other women in similar situations and seek guidance on adjusting to motherhood.
“The well-being of both the mother and baby greatly depends on postpartum care for postterm deliveries.”
- Monitor for any signs of postpartum complications
- Promote and support breastfeeding
- Address the physical and emotional changes during the postpartum period
It is crucial for mothers to have regular check-ups with healthcare providers after the delivery to detect and address any issues promptly. Additionally, joining support groups or participating in postpartum activities can provide valuable connections with other women in similar situations, enabling them to seek guidance and support while adjusting to motherhood.
Long-Term Outcomes For Babies Born Postterm
Research suggests that babies born postterm may have an increased risk of certain long-term health issues. These may include developmental delays, respiratory problems, and an increased likelihood of obesity later in life. However, it is important to note that the majority of postterm babies grow up to be healthy without significant long-term complications. Close monitoring and appropriate medical interventions can help mitigate these risks and ensure the best possible outcomes for babies born postterm. Regular pediatric check-ups and developmental assessments can provide further insight into the baby’s health and development.
In conclusion, understanding postterm delivery and its associated risks is essential for expectant mothers and healthcare providers to ensure the safe and healthy birth of a baby. By being aware of the potential complications and taking appropriate precautions, such as regular monitoring and considering induction, the well-being of both the mother and the baby can be protected. With thorough preparation and diligent postpartum care, the journey of postterm pregnancy and delivery can result in a positive and rewarding experience.
- Research suggests that babies born postterm may have an increased risk of certain long-term health issues such as developmental delays, respiratory problems, and obesity later in life.
- The majority of postterm babies grow up to be healthy without significant long-term complications.
- Close monitoring and appropriate medical interventions can help mitigate these risks for postterm babies.
- Regular pediatric check-ups and developmental assessments are important for monitoring the baby’s health and development.
💡
You may need to know these questions about postterm delivery
What is postterm delivery?
Postterm delivery refers to a situation where a pregnancy lasts longer than 42 weeks. While the average length of gestation is 40 weeks, postterm pregnancies extend beyond this timeframe. Postterm delivery can pose potential risks to both the mother and the baby, as it increases the likelihood of complications such as meconium aspiration, macrosomia, and fetal distress. Medical professionals closely monitor postterm pregnancies to ensure the well-being of both the mother and the baby, often considering interventions such as inducing labor to avoid any potential complications.
What is the most common cause of postterm delivery?
In addition to inaccurate dating based on the last menstrual period, other factors that increase the risk of postterm delivery include being a first-time mother, family history of postterm pregnancy, diabetes, obesity, and certain complications during pregnancy such as preeclampsia. However, it is important to note that even with these risk factors, the exact cause of postterm delivery remains unknown in accurately dated pregnancies. Further research is needed to better understand the underlying mechanisms and potential interventions to prevent postterm delivery.
How many weeks is a postmature baby?
A postmature baby is defined as a baby born after 42 weeks gestation, which is beyond the normal length of pregnancy. This means that a postmature baby is born 294 days or more after the first day of the mother’s last menstrual period. It is worth noting that only a small percentage, less than 6 percent, of all babies are born at this stage.
What is the difference between preterm and postterm labor?
The difference between preterm and postterm labor lies in the timing of when the baby is born. Preterm labor occurs when a baby is born before the completion of 37 weeks gestation, while postterm labor refers to babies being born after 42 weeks gestation. Preterm labor carries the risk of potential complications due to the baby’s organs and systems being less developed, while postterm labor carries the risk of the baby experiencing distress due to aging placenta and reduced amniotic fluid levels. The timing of labor plays a crucial role in determining the potential health outcomes for both the baby and the mother.
Reference source
https://www.acog.org/womens-health/faqs/when-pregnancy-goes-past-your-due-date
https://www.uptodate.com/contents/postterm-pregnancy-beyond-the-basics
https://www.chop.edu/conditions-diseases/postmaturity
https://www.futurelearn.com/info/courses/neonatal-assessment/0/steps/51130