Imagine you’re experiencing the peace-of-mind of having an IUD, knowing you’re protected against unexpected pregnancy.
But what if suddenly, that tiny flicker of doubt creeps in?
What if you suspect you might be pregnant even with your IUD in place?
In this article, we’ll delve into the intriguing world of pregnancy with an IUD in situ, exploring the possible risks, discussions with healthcare providers, and the potential complications that may arise.
Brace yourself for a fascinating journey into this perplexing scenario.
pregnancy with iud in situ
Pregnancy with an IUD in situ is possible but rare.
The failure rate of IUDs is very low, around 0.02%, meaning pregnancy can occur in about 1 out of every 5,000 people with an IUD.
If an IUD shifts position or remains in the body longer than recommended, it may no longer be fully effective at preventing pregnancy.
It is important to contact healthcare providers if pregnancy is suspected while an IUD is in place, as complications can occur.
Terminating the pregnancy should be discussed with a healthcare professional, especially in cases of ectopic pregnancy.
Removing the IUD can reduce complications, but the pregnancy is still considered high risk.
Seeking care from an Obstetrician/Gynecologist (Ob/Gyn) is important to minimize the risk of serious complications.
If the decision is made to continue the pregnancy, the IUD will likely need to be removed and complications will be monitored throughout.
Key Points:
- Pregnancy with an IUD in situ is rare, occurring in about 1 out of every 5,000 people with an IUD.
- An IUD may not be fully effective at preventing pregnancy if it shifts position or remains in the body for too long.
- Contact healthcare providers if pregnancy is suspected while an IUD is in place to prevent complications.
- Termination of the pregnancy should be discussed with a healthcare professional, especially for ectopic pregnancies.
- Removing the IUD can reduce complications, but the pregnancy is still considered high risk.
- Care from an Obstetrician/Gynecologist (Ob/Gyn) is important to minimize serious complications, and if the pregnancy continues, the IUD will likely need to be removed and complications monitored.
pregnancy with iud in situ – Watch Video
💡
Pro Tips:
1. Did you know that while it is highly unlikely, it is still possible to get pregnant with an IUD in place? This is known as an “IUD failure,” and it occurs in about 0.1 to 0.8% of cases.
2. If pregnancy occurs with an IUD in situ, there is an increased risk of experiencing an ectopic pregnancy, where the fertilized egg implants outside the uterus. This condition can be dangerous and requires immediate medical attention.
3. Copper IUDs are more effective at preventing pregnancy than hormonal IUDs, with a failure rate of less than 1%. This is due to the copper producing an environment that is toxic to sperm, preventing fertilization.
4. Interestingly, the presence of an IUD does not typically affect the accuracy of at-home pregnancy tests. You can still use these tests to detect pregnancy while having an IUD in place.
5. In rare cases, medical professionals may intentionally use a hormonal IUD as a form of treatment for certain conditions during pregnancy, such as uterine fibroids. This is done under careful supervision and should only be considered in specific circumstances.
Rare But Possible: Pregnancy With An IUD
The use of intrauterine devices (IUDs) has become increasingly popular as a highly effective method of birth control. With a success rate of over 99%, it is considered one of the most reliable forms of contraception available.
However, despite its efficacy, there is still a small chance of becoming pregnant while an IUD is in situ.
It is essential to understand that the occurrence of pregnancy with an IUD is rare. The failure rate of IUDs is as low as 0.02%, meaning that pregnancy could potentially happen in approximately 1 out of every 5,000 people with an IUD. While this may seem like an insignificant risk, it is crucial to recognize that it is not impossible.
- Bullet point 1: IUDs are highly effective with a success rate of over 99%
- Bullet point 2: Failure rate of IUDs is as low as 0.02%
- Bullet point 3: Pregnancy with an IUD is rare, occurring in approximately 1 out of every 5,000 people
Understanding The Failure Rate Of IUDs
To understand how pregnancy can occur with an IUD, it is important to consider the failure rate associated with these contraceptive devices. The failure rate represents the percentage of IUD users who become pregnant despite correct insertion and positioning of the device.
Several factors contribute to the failure rate, including the type of IUD used, duration of use, and timing of insertion. Copper IUDs, for example Paragard, offer immediate protection against pregnancy by altering the uterine environment with copper. On the other hand, hormonal IUDs like Mirena or Kyleena may take up to seven days to become fully effective, unless inserted during a person’s period when they are effective immediately.
How Does Pregnancy With An IUD Happen?
There are several scenarios in which pregnancy can occur despite the presence of an IUD.
Firstly, if the IUD is not effective immediately or if it shifts its position, it could leave room for the fertilization of an egg by sperm. This can happen when the IUD fails to create an environment hostile to sperm or when it becomes dislodged from its ideal location, potentially allowing sperm to reach the egg.
It is worth noting that while hormonal IUDs primarily work by thickening cervical mucus and thinning the uterine lining, they also have some spermicidal effects. Therefore, even if the IUD is not perfectly positioned, it may still offer some level of protection against pregnancy.
Copper Vs. Hormonal IUDs: Differences In Immediate Protection
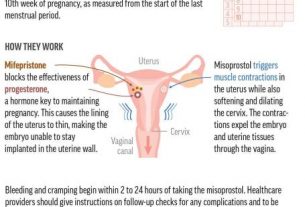
The mechanisms of action for copper IUDs and hormonal IUDs differ, resulting in varying levels of immediate protection against pregnancy. Copper IUDs, with their copper wire coils, create an environment that is hostile to sperm, preventing them from reaching and fertilizing an egg. This immediate protection makes copper IUDs highly effective right after insertion.
Hormonal IUDs, on the other hand, release progestin, a synthetic hormone that thickens cervical mucus, making it challenging for sperm to penetrate the cervix. However, it may take hormonal IUDs up to a week to provide this level of protection. Consulting a healthcare provider is crucial to discuss the timing and effectiveness of the chosen IUD, ensuring maximum contraceptive efficacy.
- Copper IUDs create a hostile environment for sperm
- Immediate protection from the moment of insertion
- Hormonal IUDs release progestin, which thickens cervical mucus
- Takes up to a week to provide full protection
- Consult healthcare provider for proper timing of IUD insertion.
Shifted Or Out Of Place: When An IUD Is No Longer Effective
While IUDs are generally highly effective in preventing pregnancy, there are instances where they may shift position or remain in the body for longer than recommended, which can make them less effective. If an IUD becomes dislodged or moves from its original position, it may no longer provide the necessary level of protection against pregnancy.
It is important to be aware of signs that might indicate the IUD is out of place, as these could also suggest a risk of pregnancy. Signs include the inability to feel the strings, abnormally long or short strings, feeling the IUD itself, pelvic pain, abnormal vaginal bleeding, severe cramping, and changes in vaginal discharge. If any of these symptoms occur, it is crucial to contact a healthcare provider immediately to evaluate the situation and determine the next steps.
- Inability to feel the strings
- Abnormally long or short strings
- Feeling the IUD itself
- Pelvic pain
- Abnormal vaginal bleeding
- Severe cramping
- Changes in vaginal discharge
Remember to reach out for medical assistance if you experience any of these symptoms.
Seek Medical Help: Suspecting Pregnancy With An IUD
If pregnancy is suspected while an IUD is in situ, it is essential to contact healthcare providers promptly. Pregnancy with an IUD can be dangerous, and professional guidance is crucial to ensure the best possible outcome.
A healthcare provider will be able to discuss appropriate options for terminating the pregnancy or continuing with the pregnancy, depending on the individual’s circumstances and preferences. Regardless of the decision made, healthcare professionals play a vital role in providing the necessary care to minimize risks and ensure the health and well-being of the person involved.
Options And Discussions: Termination Or Continuing The Pregnancy
When faced with a pregnancy with an IUD, individuals can experience a range of emotions and uncertainties. Open and honest discussions with healthcare providers are crucial in order to fully understand the options available and make informed decisions.
Terminating the pregnancy may be the most appropriate choice for some individuals, particularly in cases of ectopic pregnancy where the pregnancy occurs outside the uterus, posing severe health risks. Healthcare professionals can guide individuals through the process of pregnancy termination, which may involve medication or surgical procedures, depending on the stage of pregnancy.
On the other hand, some individuals may choose to continue the pregnancy. In such cases, the IUD will likely need to be removed, and complications will be closely monitored throughout the pregnancy. Seeking care from an Obstetrician/Gynecologist (Ob/Gyn) is crucial to reduce the risk of any serious complications and ensure proper prenatal care for both the pregnant person and the developing fetus.
Recommended Durations Of Use For Different IUDs
Different types of IUDs have varying recommended durations of use. Skyla is typically recommended for three years, Kyleena for five years, Mirena and Liletta for eight years, and Paragard for ten years. It is essential to adhere to these timeframes and contact a healthcare provider for IUD removal or replacement when the recommended duration has expired.
Using an IUD for longer than recommended may increase the risk of the device becoming less effective at preventing pregnancy. Regular follow-ups with healthcare providers are crucial to ensure the device remains in the correct position and continues to offer maximum contraceptive efficacy.
- Different IUDs have different recommended durations:
- Skyla: 3 years
- Kyleena: 5 years
- Mirena and Liletta: 8 years
- Paragard: 10 years
It is important to follow these timeframes and consult a healthcare provider for IUD removal or replacement when the recommended duration has expired. Long-term usage beyond the recommended period may reduce its effectiveness in preventing pregnancy. Regular check-ups with healthcare professionals help ensure the IUD remains in the correct position and provides optimal contraceptive efficacy.
Warning Signs: When The IUD May Be Out Of Place
Monitoring the position of the IUD and recognizing warning signs of potential displacement or malpositioning is crucial to ensure continued contraceptive effectiveness. If the IUD shifts or moves from its ideal location, there is a possibility that it may no longer provide the necessary protection against pregnancy.
Signs that the IUD may be out of place and the individual may be at risk of pregnancy include the inability to feel the strings, unusually short or long strings, the ability to feel the IUD itself, pelvic pain, abnormal vaginal bleeding, severe cramping, and changes in vaginal discharge. If any of these symptoms arise, it is crucial to consult with a healthcare provider to evaluate the situation and take appropriate action.
Symptoms And Testing: Detecting Pregnancy With An IUD
Symptoms of pregnancy with an IUD are similar to typical early pregnancy symptoms. These may include missed periods, nausea and vomiting, headaches, sore and enlarged breasts, tiredness or fatigue, mild cramping, and light spotting. However, it is important to note that these symptoms alone are not definitive proof of pregnancy, as they can also be attributed to other factors.
If pregnancy is suspected, it is recommended to take an at-home pregnancy test. However, the accuracy of these tests depends on following the instructions carefully and not testing too early after conception. It is also advised to consult a healthcare provider and consider a pregnancy test performed in a medical office for more accurate results and professional guidance.
In conclusion, while pregnancy with an IUD in situ is rare, it is not impossible. Understanding the potential risks, symptoms, and recommended actions is crucial for individuals using an IUD as a form of contraception. Immediate medical attention should be sought if any problems with the IUD or suspicion of pregnancy arise to ensure the best possible outcomes. Remember, healthcare providers are there to provide support, guidance, and appropriate care to address any concerns and ensure the safety of all parties involved. The decision to terminate or continue with a pregnancy should be made in consultation with healthcare professionals based on individual circumstances and preferences.
💡
You may need to know these questions about pregnancy with iud in situ
Can you have a viable pregnancy with an IUD?
While it is possible to have a successful pregnancy with an IUD, it is essential to be aware of the potential risks involved. Although a healthy baby can be conceived with an IUD, there is a higher chance of experiencing an ectopic pregnancy, which is considered a medical emergency. It is crucial to consult with your obstetrician promptly if you suspect a pregnancy after IUD placement to ensure appropriate medical attention and guidance.
Is it possible to have a non ectopic pregnancy with an IUD?
While the insertion of an IUD significantly lowers the likelihood of an intrauterine pregnancy, it does not guarantee protection against an ectopic pregnancy. In some rare instances, a non-ectopic pregnancy can occur with an IUD in place, albeit at a much lower rate than with no contraception. It is crucial for individuals with an IUD who experience symptoms such as abdominal pain, vaginal bleeding, or syncope to seek medical attention promptly, as these could be signs of an ectopic pregnancy.
It is crucial to remember that while an IUD is an effective form of contraception, it is not foolproof in preventing all types of pregnancy. While rare, there have been cases of non-ectopic pregnancies occurring with an IUD in place. Therefore, if you have an IUD and experience any suspicious symptoms, it is important to consult a healthcare professional to rule out the possibility of an ectopic pregnancy.
What are the outcomes of pregnancy with intrauterine device in situ a meta analysis?
A meta-analysis examining the outcomes of pregnancy with an intrauterine device (IUD) in situ concluded that conceiving with an IUD in place leads to a higher risk of various complications. These complications include an increased rate of miscarriages, placenta previa, placental abruption, chorioamnionitis, and cesarean delivery. This highlights the significant impact of an IUD in pregnancy on both maternal and fetal health, emphasizing the need for appropriate contraception management and regular IUD checks to ensure optimal reproductive outcomes.
What if I have an IUD but I’m worried I’m pregnant?
Although it is uncommon to become pregnant with an IUD, there is still a small possibility. If you have concerns about pregnancy while using an IUD, it is important to consult a doctor promptly. They can provide necessary guidance and conduct tests to alleviate any worries and ensure your well-being. Remember, it is better to address any potential concerns with a medical professional to receive accurate information and personalized advice.
Reference source
https://pubmed.ncbi.nlm.nih.gov/4032941/
https://www.verywellhealth.com/how-to-manage-an-iud-pregnancy-906758
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6366366/
https://www.verywellhealth.com/pregnant-with-iud-5210621