Antepartum fetal death: Understanding causes, prevention, and healing
– Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy.
– Stillbirth affects about 1 in 160 pregnancies each year in the United States.
– Risk factors for stillbirth include medical conditions such as obesity, diabetes, high blood pressure, and substance abuse.
– Pregnancy conditions and history can also be risk factors, such as being pregnant with multiples, having intrahepatic cholestasis of pregnancy (ICP), having complications in a previous pregnancy (preterm birth, preeclampsia, fetal growth restriction), never having given birth before, having had a miscarriage or stillbirth in a previous pregnancy, and being pregnant after the age of 35.
– Unmarried people may have a higher risk of stillbirth due to a lack of social support.
– Health disparities and racism play a role in stillbirth rates.
– Social determinants of health can affect stillbirth rates, including living conditions, access to healthcare, and exposure to chronic stress caused by racism.
– Black people have the highest stillbirth rate, more than double the rate of other groups, except for American Indian/Alaskan Native people.
– Signs and symptoms of stillbirth include the cessation of fetal movement, cramps, pain, or bleeding from the vagina.
– Tests can be conducted to determine the cause of stillbirth, including amniocentesis, autopsy, genetic tests, and tests for infections.
– After experiencing a stillbirth, it is recommended to give oneself time to heal physically and emotionally before having another baby.
– Lowering the risk of stillbirth in a subsequent pregnancy involves getting a preconception checkup, treating existing medical conditions, achieving a healthy weight, avoiding harmful substances, reporting any pain or bleeding during pregnancy, and following recommended tests and monitoring.
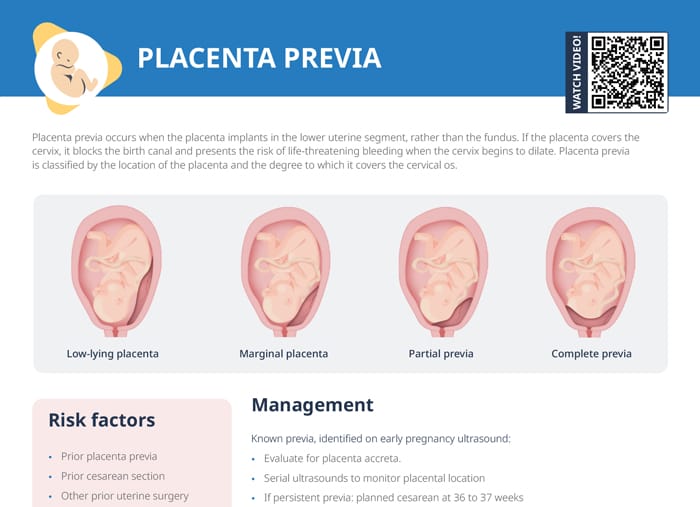
– Placental problems cause about 24% of stillbirths, while problems with the umbilical cord may lead to about 10% of stillbirths.
– Complications during pregnancy, health conditions like lupus and thyroid disorders, preterm labor, and fetal growth restriction can contribute to stillbirth.
– Rh disease, trauma or injuries, birth defects, and genetic conditions are also factors in stillbirth.
– Grieving after a stillbirth is a painful process, and families have various options for remembering their baby, such as spending time alone with the baby, naming the baby, holding the baby, and partaking in cultural or religious traditions.