Expected Date of Confinement: A Guide to Preparing for Parenthood
Expected Date of Confinement:
– The article discusses the estimated due date of a pregnant woman and various methods to calculate it.
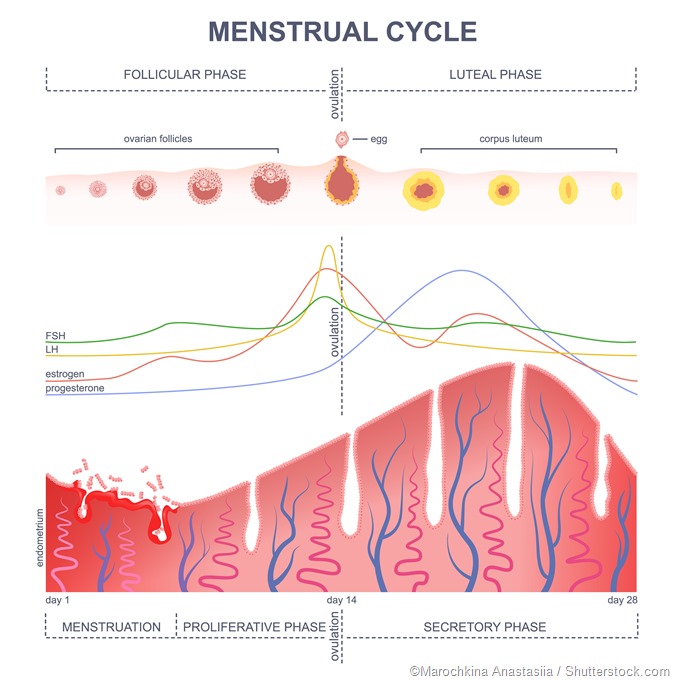
– These methods include using the last menstrual period (LMP), ultrasound, conception date, or in vitro fertilization (IVF) transfer date.
– The default calculation assumes a gestational age of 280 days or 40 weeks from the LMP.
– Only 4% of births occur on the estimated due date, so considering a range of due dates can be helpful.
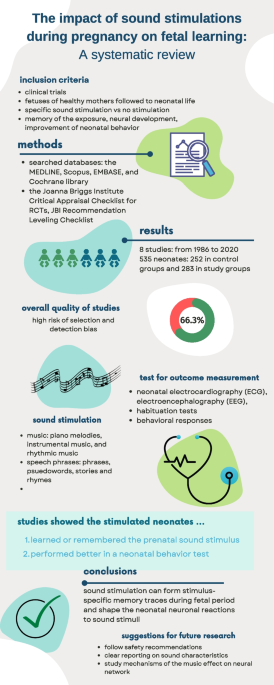
– Ultrasound uses soundwaves to compare fetal growth to typical growth rates to estimate the due date.
– Using the conception date is similar to using the LMP but has a difference of about two weeks.
– IVF can provide a more precise estimation of the due date, as the exact transfer date is known.
– The average gestational age at birth is 40 weeks.
– The due date estimate for IVF pregnancies can be determined based on various factors such as LMP, ovulation, egg retrieval, insemination, and embryo transfer date.
– Babies born between 37-39 weeks are considered early term, 39-41 weeks full-term, and 41-42 weeks late-term.
– Babies born before 37 weeks are preterm, while those born after 42 weeks are postterm.
– Doctors use these ranges as a reference to determine if any action is necessary.
– If a woman goes into labor before 37 weeks, doctors may stop labor to avoid a preterm baby with health issues.
– If a woman has not gone into labor after 42 weeks, doctors may induce labor.
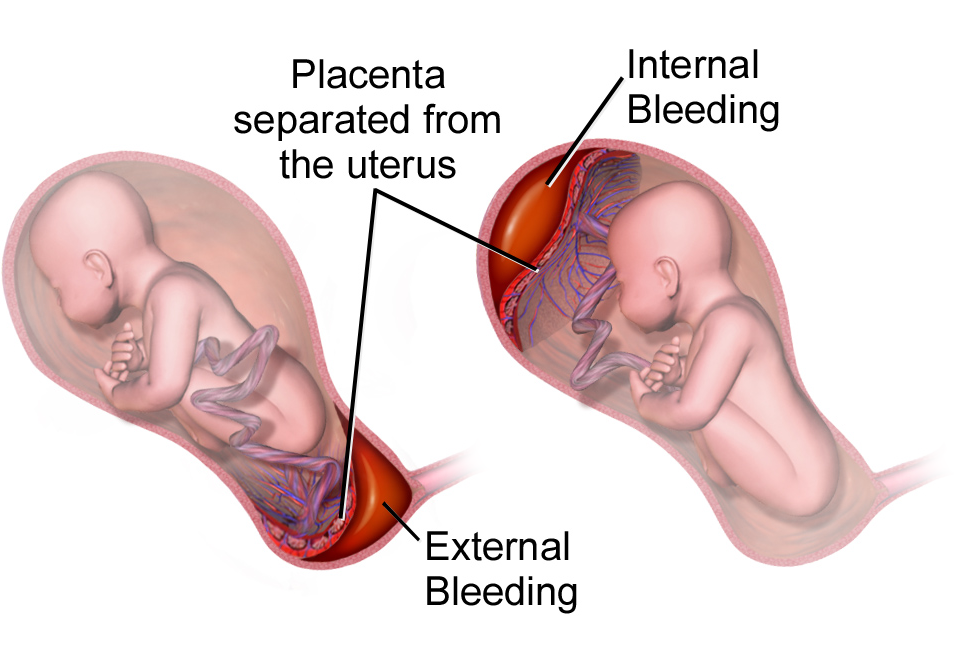
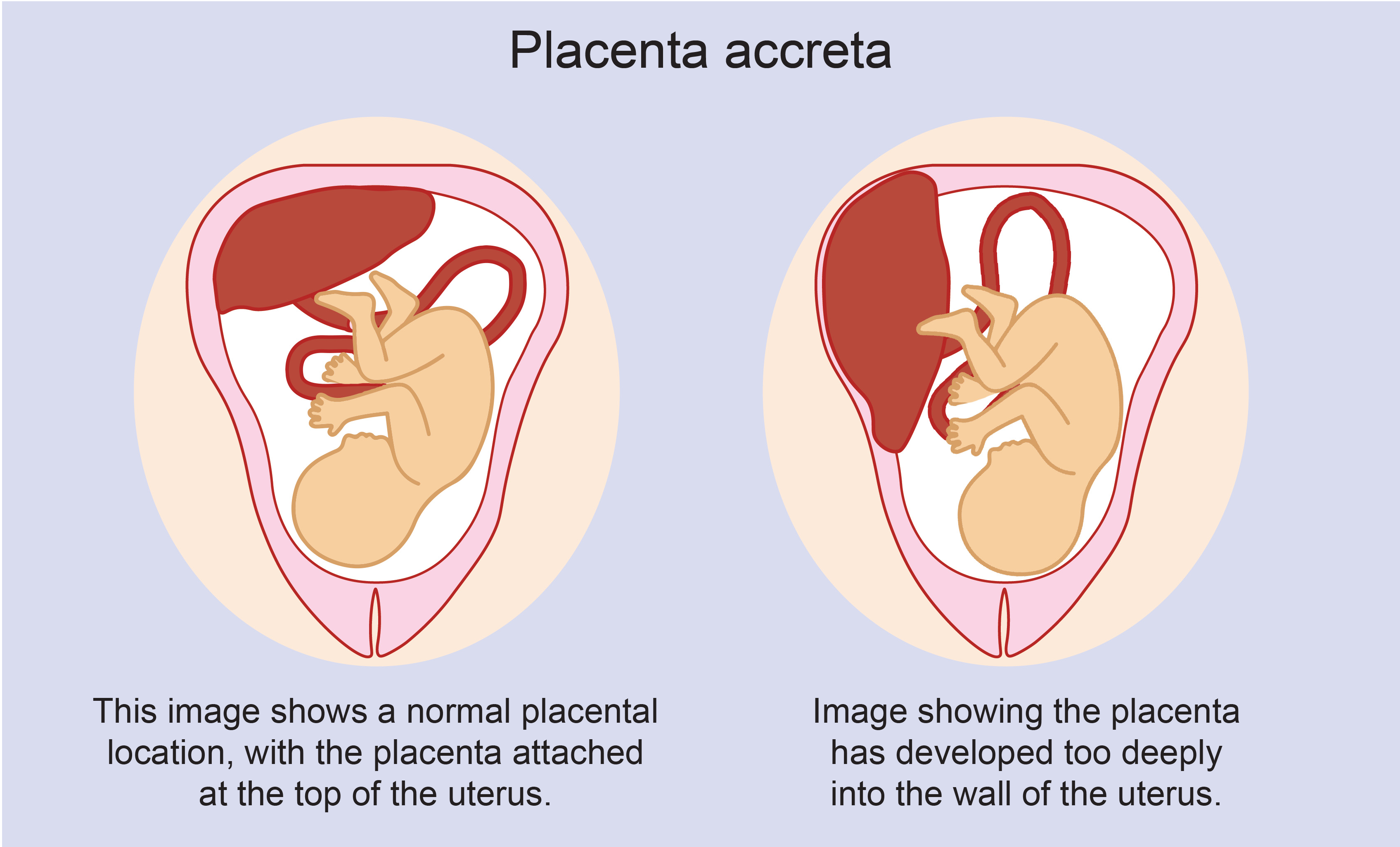
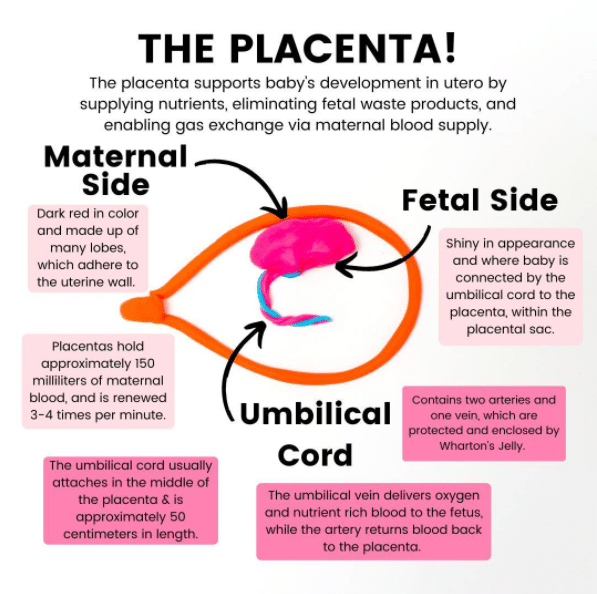
– Allowing the pregnancy to proceed beyond 42 weeks can lead to complications where the placenta may stop functioning properly while the baby continues growing, resulting in inadequate support for the baby.
– The article is a due date calculator that estimates the delivery date for pregnant women.
– The calculator can estimate the due date based on the woman’s last menstrual period (LMP), ultrasound, conception date, or IVF transfer date.
– The due date is also known as the estimated date of confinement.
– Gestational age is typically 37 to 42 weeks, with 40 weeks often used as an estimate.
– Ultrasound can be used to estimate the due date by comparing the fetus’s growth to typical growth rates.
– Using the conception date can also estimate the due date, but there is a two-week difference compared to using the last menstrual period.
– In vitro fertilization (IVF) can provide a more precise estimation of the due date since the exact transfer date is known.
– This article discusses how the due date for a pregnancy can be estimated using various methods in IVF treatment.
– The estimated due date can be based on the last menstrual period, day of ovulation, egg retrieval, insemination, or the date of embryo transfer.
– The window for a normal pregnancy is considered to be between 37 to 42 weeks.
– Doctors may take action if a woman goes into labor too early or if she hasn’t gone into labor after 42 weeks.
– Allowing the pregnancy to proceed beyond 42 weeks can lead to complications with the placenta not functioning properly.