In the joyous and transformative journey of motherhood, a silent threat lurks in the shadows, ready to strike when least expected.
Puerperal endometritis, an insidious infection that creeps into the depths of the womb, haunts the postpartum period.
Brace yourself as we unravel the mysteries of this hidden adversary and explore the remedies that lie within the realm of science.
puerperal endometritis
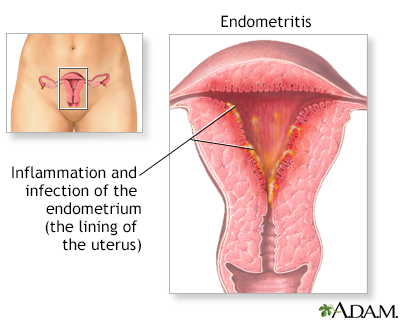
Puerperal endometritis is an infection of the lining of the womb that can occur up to six weeks after childbirth.
It is more common in women who have had a caesarean section and risk factors include long labors, membrane breaking before birth, and past history of pelvic inflammatory disease.
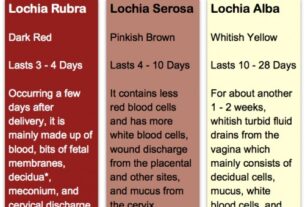
Symptoms include fever, lower tummy pain, and smelly discharge from the vagina.
Diagnosis is usually based on typical symptoms and treatment involves the use of antibiotics, commonly clindamycin and gentamicin.
If left untreated, the infection can spread and potentially lead to sepsis.
However, most women recover quickly with antibiotics, typically within 2-3 days.
Key Points:
- Puerperal endometritis is an infection of the womb lining that can occur after childbirth.
- It is more common in women who have had a caesarean section.
- Risk factors include long labors, membrane breaking before birth, and past history of pelvic inflammatory disease.
- Symptoms include fever, lower tummy pain, and smelly discharge from the vagina.
- Diagnosis is usually based on typical symptoms.
- Treatment involves antibiotics and most women recover within 2-3 days.
puerperal endometritis – Watch Video
💡
Pro Tips:
1. Puerperal endometritis is a condition that refers to the inflammation of the lining of the uterus that occurs after childbirth.
2. The prevalence of puerperal endometritis has significantly decreased throughout history due to improvements in obstetric practices, hygiene, and the introduction of antibiotics.
3. Puerperal endometritis can present with symptoms such as fever, lower abdominal pain, foul-smelling vaginal discharge, and uterine tenderness.
4. It is estimated that approximately 3-15% of women who give birth vaginally and 1-3% of women who have a cesarean section develop puerperal endometritis.
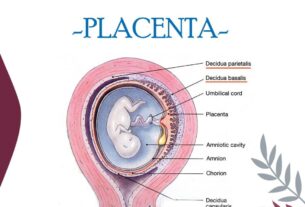
5. Puerperal endometritis can be caused by various factors, including prolonged labor, preterm birth, prolonged rupture of membranes, retained placental fragments, and genital tract infection.
Definition And Basics Of Puerperal Endometritis
Puerperal endometritis is an infection of the lining of the womb that occurs after childbirth, also known as postpartum endometritis. It affects the inner layer of the uterus, called the endometrium, typically within six weeks following delivery. If left untreated, this condition can lead to uncomfortable symptoms and complications. Understanding the causes, symptoms, and treatment options for puerperal endometritis is essential for early intervention and a successful recovery.
Timing And Occurrence Of Postpartum Endometritis
Postpartum endometritis is an infection that can occur within the first six weeks after childbirth. The symptoms typically appear between the second and tenth day after delivery, making this timeframe crucial for prompt diagnosis and treatment. It is crucial for women to be aware of the symptoms and to seek medical attention if they arise during this critical period following childbirth.
Increased Risk For Caesarean Section Births
Pregnant women who undergo a caesarean section have a higher risk of developing puerperal endometritis compared to those who have a normal vaginal delivery. This increased risk is a result of the surgical procedure, which involves an incision in the abdominal wall and uterus. The incision site serves as an entry point for bacteria, consequently raising the likelihood of infection. To mitigate this risk, healthcare professionals should take preventive measures, such as administering antibiotics before surgery, in order to reduce the incidence of postpartum endometritis in women undergoing caesarean sections.
Common Time Frame For Onset Of Symptoms
The onset of symptoms for puerperal endometritis commonly occurs between the second and tenth day after childbirth. It is during this period that women should be particularly vigilant and monitor their body for any signs of infection. The sooner the symptoms are recognized, the earlier the treatment can be initiated, reducing the risk of complications and promoting a faster recovery.
- Puerperal endometritis symptoms occur between the second and tenth day after childbirth.
- Women should be vigilant and monitor their bodies during this period.
- Early recognition of symptoms allows for prompt treatment initiation.
- Prompt treatment reduces the risk of complications.
- It promotes a faster recovery.
“The sooner the symptoms are recognized, the earlier the treatment can be initiated, reducing the risk of complications and promoting a faster recovery.”
Prevalence Of Puerperal Endometritis After Normal Delivery
Although puerperal endometritis is commonly associated with caesarean section births, it can still occur after a normal vaginal delivery. Approximately 1-3 out of every 100 women who have a normal delivery may develop endometritis. This highlights the importance of maintaining good hygiene practices and seeking medical attention if symptoms arise, regardless of the mode of delivery.
Higher Incidence In Women Who Have Had A Caesarean Section
Women who have undergone a caesarean section have a higher incidence of puerperal endometritis compared to those who have had a vaginal delivery. The surgical procedure increases the risk of infection due to the introduction of bacteria to the incision site. It is crucial for healthcare providers to closely monitor women who have had a caesarean section to detect any signs of infection early on and initiate appropriate treatment.
Risk Factors For Developing Postpartum Endometritis
Several risk factors have been identified for the development of postpartum endometritis. These include:
- long labors
- membranes breaking before birth
- meconium-stained amniotic fluid
- difficulty removing the placenta
- multiple internal examinations during labor
- infection in the genital area
- a history of pelvic inflammatory disease (PID) or bacterial vaginosis (BV)
- Group B streptococcus infection
- HIV infection
- obesity
- diabetes
- delivery in circumstances of poor hygiene
It is essential for healthcare providers to consider these risk factors when assessing postpartum women for signs of endometritis and to provide appropriate preventive measures when possible.
“Healthcare providers must be vigilant in identifying and addressing these risk factors to ensure proper care and treatment for postpartum women.”
Recognizing The Symptoms Of Puerperal Endometritis
Recognizing the symptoms of puerperal endometritis is crucial for early detection and treatment. Common symptoms include:
- Fever
- Lower abdominal pain
- Smelly discharge from the vagina
- Increased bleeding from the vagina
- Pain during sex
- Pain during urination
- General feeling of being unwell
Women who experience these symptoms should seek medical attention promptly to prevent complications and ensure a successful recovery.
Diagnosis And Testing For Postpartum Endometritis
In most cases, the diagnosis of postpartum endometritis is based on typical symptoms and signs. Healthcare providers may perform a physical examination to assess the uterus and may order additional tests, such as blood work and a pelvic ultrasound, to confirm the diagnosis and rule out other conditions. However, routine testing is usually not necessary if the symptoms are clear and the woman’s condition is stable.
- Typical symptoms of postpartum endometritis include:
- Fever
- Abdominal pain
-
Foul-smelling vaginal discharge
-
Signs that may be observed during a physical examination:
- Enlarged, tender uterus
- Tenderness or pain in the lower abdomen
- Abnormal vaginal discharge
It is important for healthcare providers to accurately diagnose and treat postpartum endometritis to prevent complications. If a woman is experiencing symptoms or signs of the condition, it is recommended to seek medical attention.
“Postpartum endometritis can lead to serious complications if left untreated, so early diagnosis and appropriate management are crucial.”
Treatment Options For Puerperal Endometritis
The primary treatment for puerperal endometritis involves the use of antibiotics to eliminate the infection. The most commonly prescribed antibiotics for this condition are clindamycin and gentamicin. These antibiotics are effective in targeting the bacteria responsible for the infection. With prompt and appropriate treatment, most women recover from puerperal endometritis within 2-3 days. Complications are rare when treated with antibiotics, but if left untreated, the infection can spread to other parts of the body and potentially lead to sepsis, a life-threatening condition.
To prevent puerperal endometritis, healthcare providers may offer antibiotics to women undergoing a caesarean section to reduce the likelihood of infection. Additionally, antibiotics may be administered during labor if the woman has Group B streptococcus in her vagina to protect both her and the newborn baby from infections caused by this bacterium. Hygiene practices, including proper handwashing and disinfection of medical equipment, can also contribute to reducing the risk of developing puerperal endometritis.
💡
You may need to know these questions about puerperal endometritis
What is the cause of postpartum endometritis?
Postpartum endometritis is predominately caused by the ascent of bacteria from the lower genital or gastrointestinal tract into the uterus. This infection leads to a range of symptoms including uterine tenderness, pelvic or abdominal pain, fever, malaise, and occasionally discharge. Diagnosis of postpartum endometritis is primarily clinical, with culture rarely providing significant assistance in confirming the condition.
What are the symptoms and signs of puerperal endometritis?
Puerperal endometritis is characterized by a range of symptoms and signs. Patients often experience chills, headaches, malaise, and loss of appetite. In some cases, the only noticeable symptom is a mild fever. Additionally, individuals may display pale skin, rapid heart rate, and an increased number of white blood cells. The uterus is typically enlarged, tender, and soft to the touch. Discharge may vary, ranging from reduced amounts to excessive and foul-smelling, with or without the presence of blood.
How long does postpartum endometritis last?
Fortunately, the majority of women experiencing postpartum endometritis can expect a swift recovery with the aid of antibiotics. Typically, within the span of 2-3 days after commencing antibiotic treatment, noticeable improvement in symptoms can be observed. Fortunately, complications stemming from postpartum endometritis are infrequent, allowing women to swiftly regain their optimal health and well-being.
What is a puerperal infection?
A puerperal infection refers to a bacterial infection that occurs within 28 days following childbirth, miscarriage, or induced abortion. This condition involves an infection of the genital tract caused by bacteria. Puerperal infections can lead to various symptoms and complications, and it is crucial to promptly diagnose and treat them to ensure the well-being of the mother. Such infections can be caused by a range of bacteria and require proper medical attention to prevent any potential health risks.
Reference source
https://www.uptodate.com/contents/postpartum-endometritis
https://www.msdmanuals.com/en-pt/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/postpartum-endometritis
https://www.msdmanuals.com/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/postpartum-endometritis
https://patient.info/pregnancy/postpartum-endometritis-leaflet